Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.4 Bogotá oct./dic. 2016
Prognostic Factors Associated with Mortality in Cirrhotic Patients with Bleeding Varices at Two Hospitals in Bogotá D.C. Colombia
Julián David Martínez MD (1,2), Martín Alonso Garzón MD (2,3), Mario H. Rey MD (2), Geovanny Hernández MD (3), Óscar Beltrán MD (3), Jorge Ceballos MD (3), Enrique Ponce de León MD (3), Adriana Varón Puerta MD (3)
(1) Faculty of Medicine of the National University of Colombia in Bogotá DC, Colombia
(2) Gastroenterology Unit of the Hospital Universitario de la Samaritana in Bogotá DC, Colombia
(3) Hepatology Unit of the Fundación Cardioinfantil in Bogotá DC, Colombia
Received:Â Â Â 24-09-15Â Accepted:Â Â Â 01-10-16
Abstract
Background: Ninety percent of cirrhotic patients will develop esophageal varices, and bleeding will occur in 30% of these patients at some point in their lives.
Objective: The objective of this study was to identify prognostic factors associated with mortality in cirrhotic patients with bleeding varices.
Method: We present a retrospective cohort study of patients with bleeding digestive varices over a period of 30 months.
Results: This study included 63 patients (33 men and 30 women) whose average age was 56 years (SD: 16 years). 52.4% of these patients' Child-Pugh classification was B. The average stay in the hospital was 10 days. Twelve (19%) died. Hypovolemic shock (p = 0.033) and red blood cell transfusion (p = 0.05) were related to mortality. Bivariate analysis showed that the variable most closely related to mortality was hepatic impairment with Child-Pugh C classification (p = 0.00). Comparisons of numerical variables found that the creatinine value (Mean: 1.74 mg/dl, p = 0.043) and length of hospital stay (mean time:10 days, p = 0.057) were higher in patients who died. In the bivariate analysis, Child-Pugh C (Exp (B) = 0.068, p = 0.002) and creatinine (Exp (B) = 0.094, p = 0.034) remained statistically related to the outcome of interest.
Conclusions: Mortality from bleeding varices in the patients in this study is comparable to current international standards. Because advanced liver disease and impaired renal function are associated with increased mortality, patients with bleeding varices who have predictors for mortality during decompensation due to bleeding warrant close monitoring and early interventions to avoid negative outcomes.
Keywords
Hemorrhaging, digestive, varices, esophageal varices.
Introduction
Portal hypertension leads to the development of portosystemic collateral venous vessels. Of these, esophagogastric are the most important because bleeding develops frequently and is a serious and often fatal complication. More than 90% of patients with cirrhosis will develop esophageal varices (EV) and at some point in their life, 30% of them will develop bleeding. In 40% of the compensated cirrhotics, EV will be found in digestive endoscopy: of these, patients with ascites account for 60%. (1)
Increases in the size of varicose veins significantly increase the risk of bleeding. Decompensated cirrhotics (Child-Pugh B and C classification), alcoholics, red spots on the surface of the EV, and a hepatic venous pressure gradient over 20 mm Hg are the main factors associated with increased size and risk of bleeding. For EVs that have been detected, the annual incidence of hemorrhaging is 5% for small EVs and 15% for medium and large EVs (2). Hemorrhaging of varices is the most common cause (70%) of gastrointestinal bleeding in patients with cirrhosis. Mortality rates range from 6% to 42%. Initial bleeding may be the cause of death, although serious complications such as infections, renal failure, hepatic encephalopathy, and rebleeding are also important causes of death. (3)
Endoscopic treatment of varices aims to reduce internal wall pressure by obliterating the veins. The two most commonly used methods are injection of sclerosing substances and elastic band ligation. Ligation consists of mechanical strangulation of the varice by the placement of small rubber rings which destroy the vessel and cause only a limited inflammatory reaction in the esophageal mucosa. The control of acute bleeding is achieved in 90% of cases. Risk of rebleeding is also reduced. (4)
Terlipressin is a synthetic vasopressin analogue that has a longer half-life and fewer side effects than does vasopressin itself. It decreases portal pressure significantly within four hours of administration. Compared with placebos, it controls acute bleeding from esophageal varices in 80% more cases at 48 hours and 67% more cases at 5 days. (5)
A metaanalysis of 20 studies has shown that terlipressin significantly reduced relative risk of mortality by 34% making terlipressin the drug of choice preceding endoscopic therapy for esophageal variceal bleeding. (6)
This study identifies prognostic factors associated with mortality in cirrhotic patients with digestive bleeding of variceal origin.
Materials and Methods
A retrospective cohort study was conducted between January 2010 and December 2012. Patients included in the study had been admitted to the emergency departments of Fundación Cardioinfantil (FCI) or Hospital Universitario de la Samaritana, both of which are university institutions in Bogotá, Colombia. Patients had been admitted for upper gastrointestinal bleeding and also had histories of chronic liver disease and/or portal hypertension syndrome or clinical suspicion of these conditions. In addition to initial resuscitation with crystalloids, parenteral terlipressin (Glypresin, Serring, Germany) was administered. Subsequently, on average twelve hours later, after resuscitation and achievement of adequate hemodynamic conditions, esophagogastroduodenoscopy (Olympus Exera II CV 180, Tokyo, Japan) was performed to determine the origin of bleeding. When esophageal or gastric varices were found and considered to be the source of bleeding, band ligated was performed (Cook Medical MBL-6-I, USA). For this study we have included demographic variables, background factors, Child-Pugh classifications, MELD scores, bleeding control, rebleeding while hospitalized, mortality and lengths of hospital stays.
The study protocol was approved by the ethics committees of the two institutions.
Results
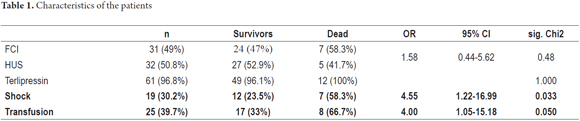
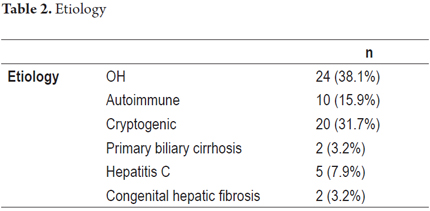
We included 63 patients in the analysis. Mean patient age was 56 ± 16 years. Mean creatinine and platelet counts were within normal ranges found in the general population. Mean number of days of hospitalization was 10. The average MELD (Model for End-Stage Liver Disease) score in the study population was 12. Of these, 19% (12 patients) died. Mortality was similar in both hospitals and among both sexes. In the study population, hematemesis was the most frequent symptom. Terlipressin and antibiotics were used in most cases. Alcoholic and cryptogenic cirrhosis accounted for most of the cases. Most patients Child-Pugh B classification of severity of the disease. Nearly half of the patients had large varices (Tables 1 and 2).
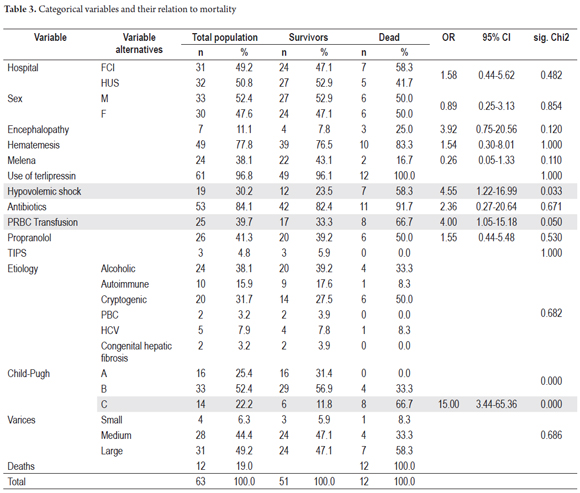
Of the categorical variables evaluated, the history of hypovolemic shock and the need for transfusion of blood products had statistically significant relations to mortality. The bivariate analysis shows that the independent variable most closely related to mortality was Child-Pugh C classification.
Binary Logistic Regression
To discard the confounding variables and to determine variables definitely related to mortality, binary logistic regression was performed. Mortality was considered to be the dependent variable. The 63 cases were included in the model. Bivariate analysis for statistical significance of association or difference showed that Child-Pugh C (Exp (B) = 0.068, p = 0.002) and creatinine (Exp (B) = 0.094, p = 0.034) were statistically related to the outcome of interest (model = 0.000, percentage of patients adequately classified = 85.7%) (Table 3).
Discussion
In cirrhotic patients, digestive bleeding of variceal origin is a serious cause of decompensation leading to high mortality rates of around 20%. (7) Severity according to the Child-Pugh scale, alcoholic etiology, renal involvement, and requirements for packaged red blood cell transfusions have been recognized as predictors of mortality.
A notable decrease in mortality of these patients has occurred in the last decade. It is associated with early therapeutic interventions including optimization of support in intensive care, the use of vasopressors to reduce portal pressure, the use of prophylactic antibiotics and timely endoscopic intervention. (8)
This study found a mortality rate of 19.04% which is comparable to current international standards (9) and which is significantly lower than the 30% reported by the authors in 2003. (10, 11) At that time tools such as endoscopic ligation of varices were not in use. Bleeding varices were treated exclusively with sclerotherapy with ethanolamine oleate and vasopressin as a portal pressure reducing agent, and antibiotic prophylaxis was not systematically prescribed for patients with bleeding varices.
We found no significant differences between mortality rates at the two institutions nor in relation to sex of the patients. Two earlier Latin American publications, one from Argentina and one from Peru, also found that consumption of alcohol was the main cause of chronic liver disease in patients with bleeding varices. Most patients in these studies were admitted with either Child-Pugh B or Child-Pugh C functional classifications and more than half had medium and large esophageal varices at the time of the first endoscopy. (11, 12) These results are similar to those of our study.
Significant differences were observed in the gender balances of patients, the study population of Berreta et al. in Argentina) was 98% male while that of Parra et al. in Peru was 55.5% male. In our cohort, 52.4% were men. Mortality in the Bereta study was 19.8%, while that of Perez et al. was 17.5%, both of which are comparable to our results.
Endoscopic management is performed within international standards in a timely manner under the premise of providing the patient with airway protection and hemodynamic stability. In our study, the success of endoscopic treatment with adequate resuscitation and early initiation of vasopressors was 94%. These results considered good in international reports.
In this study bleeding was controlled with vasoactive agents, primarily terlipressin (97%), and there were no differences in mortality with the use of this treatment compared to data from similar studies available in the literature. (13, 14)
Previous Latin American studies of bleeding varices in Colombia, Argentina and Peru have not reported the use of vasopressor agents. The administration of these vasoactive substances is an international recommendation for the management of all patients with high digestive tract bleeding varices. (8)
Also following international recommendations for the management of this type of patients, eighty-four percent of the patients in this study received prophylactic antibiotic therapy. This recommendation has been made because of the usefulness of antibiotics for reducing mortality, risk of rebleeding and renal compromise as shown in the metaanalysis by Soares-Weiser et al. (6, 15, 16)
With respect to the use of transjugular intrahepatic portosystemic shunts (TIPS), Garcia-Pagan et al. recommend early placement of shunts to reduce the risk of rebleeding and mortality. They recommend that his be done within the first 72 hours after admission for patients with Child-Pugh C of less than 14 points and in patients with Child-Pugh B who have acute bleeding. (17). In our study, only 3 patients received TIPS as rescue therapy. This suggests that lack of experience in our environment delays the decision to use this tool.
Prognostic factors for mortality in patients with bleeding varices in the digestive tract have been studied extensively. Abraldes et al. found that f cirrhosis, Child-Pugh classification, and blood pressure on admission predicted the risk of therapeutic failure in the first 5 days. (18)
Piqueras et al. found higher mortality rates in patients over 65 years of age, patients with high Child-Pugh scores, patients with hepatocellular carcinoma, patients with encephalopathy and patients with bacterial infections. (19) An earlier study by Gomez et al. in Colombia reported that patient mortality was directly associated with advanced Child-Pugh classification, size of esophageal, and infections in the ascitic fluid. (10) Berreta reported that failure of initial endoscopic therapy and Child-Pugh C classification were predictors of hospital mortality. (11) García-Pagán defined high-risk patients as those with active bleeding at admission and those with Child-Pugh B and C functional classes. (17) Augustin found that Child-Pugh C functional class with creatinine level over 1 mg/dL had a high mortality risk associated with bleeding within the six weeks following admission. (13) Perez et al. reported similar results. Of the categorical variables evaluated in this study, patients' histories of shock and requirements for transfusion were statistically related to mortality. Child-Pugh C (Exp (B) = 0.068, p = 0.002) and creatinine levels (Exp (B) = 0.094, p = 0.034) had a statistically significant associations with the outcome of interest.
Mortality rates of patients with bleeding varices at the two university hospitals are comparable to current international standards. Advanced liver disease according to the Child-Pugh classification and impaired renal function are related to mortality in cirrhotic patients with bleeding varices. For this reason patients who have predictors of mortality during decompensation due to bleeding varices require especially close monitoring and may require early intervention to avoid negative outcomes.
Financing
No sponsorship of any kind was received to carry out this study.
Conflicts of interest
The authors declare no conflict of interest.
References
1. Berzigotti A, Seijo S, Reverter E, et al. Assessing portal hypertension in liver diseases. Expert Rev Gastroenterol Hepatol. 2013;7(2):141-55. [ Links ]
2. Bosch J, Berzigotti A, Garcia-Pagan JC, et al. The management of portal hypertension: rational basis, available treatments and future options. J Hepatol. 2008;48(Suppl 1):S68-92. [ Links ]
3. Garcia-Tsao G, Lim JK. Management and treatment of patients with cirrhosis and portal hypertension: recommendations from the Department of Veterans Affairs Hepatitis C Resource Center Program and the National Hepatitis C Program. Am J Gastroenterol. 2009;104(7):1802-29. [ Links ]
4. Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362(9):823-32. [ Links ]
5. Ioannou G, Doust J, Rockey DC. Terlipressin for acute esophageal variceal hemorrhage. Cochrane Database Syst Rev. 2003;(1):CD002147. [ Links ]
6. Ioannou GN, Doust J, Rockey DC. Systematic review: terlipressin in acute oesophageal variceal haemorrhage. Aliment Pharmacol Ther. 2003;17(1):53-64. [ Links ]
7. Seo YS, Kim YH, Ahn SH, et al. Clinical features and treatment outcomes of upper gastrointestinal bleeding in patients with cirrhosis. J Korean Med Sci. 2008;23(4):635-43. [ Links ]
8. de Franchis R, Baveno V Faculty. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53(4):762-8. [ Links ]
9. Boyd R, Butler J. Best evidence topic report. Terlipressin or somatostatin for the treatment of bleeding oesophageal varices. Emerg Med J. 2005;22(6):433-4. [ Links ]
10. Gómez D, Garzón MA. Várices esofágicas: experiencia clínica en un hospital de referencia regional. Rev Colomb Gastroenterol. 2003;18:20-3. [ Links ]
11. Berreta J, Kociak D, Corti R, et al. Predictors of intrahospitalary mortality in the upper gastrointestinal variceal bleeding due to chronic liver disease treated endoscopically. Acta Gastroenterol Latinoam. 2008;38(1):43-50. [ Links ]
12. Parra Pérez VF, Raymundo Cajo RM, Gutiérrez de Aranguren CF. Related factors to re-bleeding and mortality in cirrhotic patients with acute variceal bleeding at Hipolito Unanue Hospital, Lima, Perú. Rev Gastroenterol Peru. 2013;33(4):314-20. [ Links ]
13. Augustin S, Gonzalez A, Genesca J. Acute esophageal variceal bleeding: Current strategies and new perspectives. World J Hepatol. 2010;2(7):261-74. [ Links ]
14. Moitinho E, Escorsell A, Bandi JC, et al. Prognostic value of early measurements of portal pressure in acute variceal bleeding. Gastroenterology. 1999;117(3):626-31. [ Links ]
15. Thomopoulos KC, Labropoulou-Karatza C, Mimidis KP, et al. Non-invasive predictors of the presence of large oesophageal varices in patients with cirrhosis. Dig Liver Dis. 2003;35(7):473-8. [ Links ]
16. Nevens F. Non-invasive variceal pressure measurements: validation and clinical implications. Verh K Acad Geneeskd Belg. 1996;58(4):413-37. [ Links ]
17. Garcia-Pagan JC, Caca K, Bureau C, et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362(25):2370-9. [ Links ]
18. Abraldes JG, Villanueva C, Banares R, et al. Hepatic venous pressure gradient and prognosis in patients with acute variceal bleeding treated with pharmacologic and endoscopic therapy. J Hepatol. 2008;48(2):229-36. [ Links ]
19. Piqueras B, Banares R, Rincon D, et al. Predictive factors of the mortality of digestive hemorrhage caused by esophageal varices in elderly patients. Gastroenterol Hepatol. 2001;24(2):51-5. [ Links ]











 texto en
texto en