Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.4 Bogotá Oct./Dec. 2016
Evidence Based Medicine Perspective on Long-Term Adverse Effects of Proton Pump Inhibitors
Jaime A. Cardona-Ospina MD (1,2), Diego Alejandro Medina-Morales MD (1), Alfonso J. Rodríguez-Morales MD MSc (2), Jorge E. Machado-Alba MD MSc PhD.(3)
(1) Pharmacoepidemiology and Pharmacovigilance Research Group in the Technological University of Pereira-Audifarma S.A. in Pereira, Colombia
(2) Faculty of Health Sciences at the Technological University of Pereira in Pereira, Colombia
(3) PhD in Pharmacology, Tenured Professor of Pharmacology at the Technological University of Pereira. Pharmacoepidemiology and Pharmacovigilance Research Group at the Technological University of Pereira-Audifarma S.A. in Pereira, Colombia
Received:Â Â Â 25-01-16Â Accepted:Â Â Â 01-11-16
Abstract
Proton pump inhibitors (PPIs) are the most effective gastric secretion suppressors and are among the most widely prescribed and widely available drugs in the United States of America. In some cases they are prescribed without justification. In recent years, concerns have arisen over reports of major adverse reactions related to the use of PPIs. However, the quality of the evidence has not been conclusive, and in some cases the magnitude of the risk has not been clinically significant. The objective of this review is to present the available evidence regarding the most important adverse events related to PPIs.
Keywords
Proton pump inhibitors, adverse drug side effects, adverse drug reactions, evidence-based medicine, pharmacovigilance (Source: DeCS).
Introduction
Proton pump inhibitors (PPIs) are drugs that suppress gastric secretions by inhibiting H + K + -ATPase in the parietal cells of the body and the gastric fundus. When ingested these prodrugs pass into the general circulation and diffuse through the membranes of the parietal cells to the canaliculi where the acidic pH (about 0.8) induces the formation of a tetracyclic sulfonamide which is covalently bound to the Sulfhydryl groups of cysteine ââin H + K + -ATPase. This irreversibly inactivates it resulting in inhibition of gastric acid secretion until new proton pumps are synthesized. Currently, there are five PPIs on the market: omeprazole, esomeprazole, lansoprazole, pantoprazole and rabeprazole. Although they use different pyridine or benzimidazole groups, their pharmacological properties are similar.
These drugs are among the most widely prescribed in the United States especially since low-cost generics sold over-the-counter without prescriptions allows patients to easily obtain them. (1) The necessity of prescribing them for long-term treatment, reports of various adverse drug reactions (ADRs), overuse in primary care, emergency services and hospitalization, and prescriptions without proper indications have led to reflections about safe use which have resulted in the publication of several studies on this topic. (2, 3) This paper reviews the current literature about the most important clinical ADRs.
Adverse Reactions Associated with PPIs
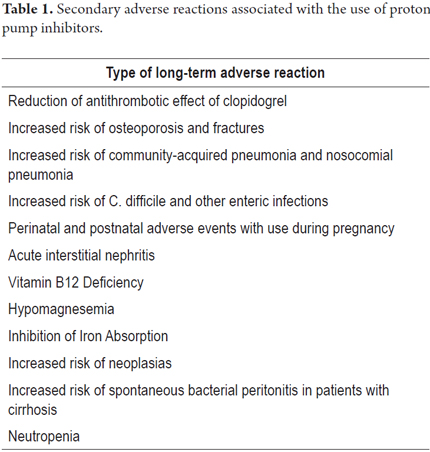
ADRs associated with the use of PPIs can be classified into two groups: short term or primary reactions and long term or secondary reactions. One to five percent of patients report primary adverse reactions including headaches, diarrhea, constipation, nausea and rashes. These are common to the pharmacological group although frequencies have not been compared among PPIs. (4) ADRs associated with prolonged use have been subject to more studies due to their clinical importance (Table 1).
Reduction of Antithrombotic Effect of Clopidogrel
One cause of concern is that pharmacokinetic data indicates that there may be an interaction between clopidogrel, which requires activation by the CYP2C19 isoenzyme, and omeprazole, which inhibits the CYP2C19 isoenzyme. Pantoprazole and esomeprazole use alternate routes. In vitro experiments have reported a reduction of clopidogrel's biological action on platelet functioning, but later studies yielded conflicting answers about the clinical relevance of this interaction and about variations of results among PPI molecules. (5) The 2010 COGENT study concluded that use of omeprazole together with clopidogrel reduces the risk of gastrointestinal events compared to the use of clopidogrel plus a placebo and that it does not increase the risk of cardiovascular events (death, nonfatal myocardial infarction, revascularization, and/or strokes). However, this study was suspended early due to loss of sponsorship. (6) It included 3,627 out of 5,000 patients with an average follow-up of 133 days. There were 136 cardiovascular events (omeprazole: 69, placebo: 67, p = 0.050) and 105 gastrointestinal events (omeprazole: 38, placebo 67, p = 0.007). Although there was no statistically significant difference between cardiovascular events in both groups, a clinically important association for with simultaneous use could not be ruled out. Also, a subsequent analysis of high-risk cardiovascular patients included in that study who received concomitant treatment with omeprazole found a significant reduction in gastrointestinal events without any increase in cardiovascular risk. (7)
On the other hand, a 2012 metaanalysis of 27 studies of a total of 159,998 patients concluded that the combined use of PPIs and clopidogrel was associated with increased risks of major cardiovascular events (HR: 1.40; 95% CI: 1.19-1.64) and acute coronary syndrome (HR: 1.42; 95% CI: 1.14-1.77) but not with death from all causes (HR: 1.30; 95% CI: 0.91-1.91-1.86) cardiovascular death (HR: 1.21: 95% CI: 0.60-2.43) or stent thrombosis (HR: 1.52; 95% CI: 0.87-2.65). (8) However, during the individual analysis of pantoprazole alone, it was associated with an increased risk of major cardiovascular events (HR: 1.52; 95% CI: 1.18-1.94). Another metaanalysis of 23 studies of a total of 222,311 participants found that cardiovascular risks increased significantly when omeprazole, esomeprazole, lansoprazole were used simultaneously with clopidogrel (OR: 1.24, 95% CI: 1.07-1.43, OR 1.32, 95% CI %: 1.09-1.60; OR: 1.41; 95% CI: 1.21-1.64, respectively). Nevertheless, an analysis of seven observational studies in the same metaanalysis found an increase in cardiovascular risk from PPIs without clopidogrel (OR: 1.28; 95% CI: 1.14-1.44) over no medication at all. (9)
In conclusion, the probability of major cardiovascular events may in fact increase, but the probability of fatal outcomes does not. Nevertheless, the heterogeneity of outcomes and data indicating increased cardiovascular risks in patients receiving PPIs without clopidogrel suggest a residual confounding factor or the presence of an alternate mechanism that accounts for this effect.
Risk of Osteoporosis and Fractures
Absorption of calcium in the small intestine is facilitated by ionization of insoluble salts at low pH. Initially, it was postulated that increases in gastric pH would produce a compensatory physiological response with increased bone resorption secondary to elevation of parathyroid hormone secretion which would lead to increased risk of osteoporosis and fractures. However, given the presence of a proton pump in osteoclasts, a reduction in bone resorption due to the drug's inhibitory effect is also possible.
In 2010, a cross-sectional study used The Manitoba Bone Mineral Density Database to establish the relationship between chronic use of PPIs and osteoporosis or accelerated loss of bone density. The study compared people who used PPIs with those who did not. Multiple studies show slight increases of the general risk of fractures, but also show an apparently lower risk of spinal fractures. Nevertheless, the heterogeneity of results is significant. The same studies also show reductions in femoral mineralization with increased risks of osteopenia and osteoporosis. (10, 11) It has also been found that for hip fracture (OR: 1.25; 95% CI: 1.14-1.37), when adjusted for time of PPI use, there is a statistically significant increase of risk associated with use of PPIs for short-term users ( OR: 1.24; 95% CI: 1.19-1.28) but not for long-term users (OR: 1.30; 95% CI: 0.98-1.70). (12) Although the association is likely, the heterogeneity of the data does not allow for a definitive conclusion.
Increased Risk of Community-acquired pneumonia and Nosocomial Pneumonia
Acidic gastric pH functions as a barrier to growth of microorganisms in the gastrointestinal tract. Multiple studies have documented increased bacterial growth with the use of PPIs although this is generally of no clinical importance. (13) Nevertheless, episodes of aspiration of microscopic amounts of gastric contents secondary to gastroesophageal reflux under conditions of altered pH of the pulmonary secretions or altered phagocytic function are cause for concern about increased risks of community-acquired pneumonia and healthcare-associated pneumonia (HCAP). (14)
With regard to the risk of community-acquired pneumonia, observational studies seem to support an association especially for use of less than 30 days at high doses. In 2012, a meta-analysis of nine cohort and case-control studies analyzed the risk of community-acquired pneumonia based on current use of PPIs (OR: 1.39, 95% CI: 1.09-1.76), use for less than 30 days (OR: 1.65, 95% CI: 1.25-2.19), for more than 180 days (OR: 1.10, 95% CI: 1.00-1.21), at low doses (OR: 1.17, 95% CI: 1.11-1.24) and at high doses (OR: 1.50; 95% CI: 1.33-1.68) (15).
Results consistently support an association between usage of PPIs and healthcare-associated pneumonia. In 2011, a metaanalysis showed an increased risk with PPIs (RR: 1.22, 95% CI: 1.01-1.48, I(2) 30.6%) with no differences between anti-H2 and PPIs but with PPIs being more effective for the prophylaxis of stress ulcers and with a significantly lower rate of gastrointestinal bleeding. (16, 17) The evidence supports an association of PPI use with increased risk of community-acquired pneumonia and healthcare-associated pneumonia, but no pathophysiological mechanisms have yet been elucidated.
Risk of C. Difficile Infections and Other Enteric Infections
In addition to increased intestinal bacterial growth, PPIs have immunomodulatory and anti-inflammatory effects and have been suggested to favor bacterial translocation. Since some microorganisms have shown different tolerances to different gastric pH levels, the risk of infection by certain pathogens could increase. This is especially true for Salmonella spp., Campylobacter jejuni, enteroinvasive Escherichia coli (EIEC), Clostridium difficile, Vibrio cholerae and Listeria spp. (18) Several metaanalyses have found increased risks of infections, especially for C. difficile. Nevertheless, results are not homogenous for interactions between and among variables, in particular for concomitant use of antibiotics.
In 2012 Kwok et al. found an OR of 1.74 (95% CI: 1.47-2.85, I (2) = 78%, p = 0.005) for greater risks of C. difficile infections when patients received PPIs and antibiotic treatment simultaneously (OR: 1.96; 95% CI: 1.03-3.70). The Rothman synergy index was 1.36, with a 0.19 hazard ratio attributable to the interaction of PPIs and antibiotics which indicates that risk increases beyond the sum of the effects of each drug. (19) However, in 2012 Tleyjeh et al. concluded that this conclusion was based on such low quality evidence that a causal relationship cannot be established. They suggested that, if the risk of C. difficile infections increases, the number needed to harm (NNH) would be 3,925 patients in one year. (20)
Risk of Adverse Perinatal and Postnatal Events
Multiple cohort studies and metaanalyses have studied associations between PPI use and congenital malformations and other adverse perinatal events. (21) The results suggest that PPIs, especially omeprazole are safe, even when administered during the first trimester of pregnancy. However, recent data show an increase in the risk of childhood asthma in children of mothers exposed to any type of antiulcer agent (OR: 1.23; 95% CI: 1.01-1.51). (22)
Risk of Acute Kidney Injury
Studies have also been published about potential associations of PPI use with acute renal injury and interstitial nephritis. Klepser et al. found an association between renal disease and use of PPIs (OR: 1.72; 95% CI: 1.27-2.32) which persisted even after adjustment for confounding variables. (23) However, given the nature of the studies and the number of events reported, no definitive conclusions can be drawn.
Vitamin B12 Deficiency
Cyanocobalamin is obtained from a diet rich in proteins that must be cleaved by pancreatic proteases activated by gastric acid secretion. This must then be absorbed into the terminal ileum after binding to the intrinsic factor. A cross-sectional study conducted in 2008 compared 125 patients over 65 years of age who had used PPIs for more than 3 years with patients who had not used PPIs. The study found no differences in vitamin B12 levels ( P = 0.730) even after adjusting for the presence or absence of Helicobacter pylori, age, sex, and C-reactive protein levels. Furthermore, no differences were found in homocysteine ââlevels or in mean corpuscular volume values. ââ(24)
More recently, 36 hospitalized patients between 60 and 80 years of age were assessed for vitamin B12 deficiencies. Seventeen were long term users of PPIs and nineteen did not take PPIs. They were all assessed for baseline levels of vitamin B12 and assessed again for the effect of administration of a vitamin B12 nasal spray after 8 weeks. Chronic PPI users were found to have lower basal levels of the vitamin and higher levels of methylmalonic acid (75% vs. 11%, p = 0.006). (25) An association between vitamin B12 deficiency and concomitant treatment with metformin and PPIs or anti-H2 has also been found. (26) Due to the small size of the samples and the design of the studies, it is difficult to draw definitive conclusions, but the great possibility of vitamin B12 deficiency should be considered, especially for elderly patients undergoing constant therapy or who have poor nutritional status and for patients with diabetes mellitus and concomitant treatment with metformin.
Risk of Hypomagnesaemia
In 2006, an association between hypomagnesemia and PPIs was reported. Since then, there have been at least 13 reports of associated hydroelectrolytic alterations including hypomagnesaemia, hypocalcemia, hypokalemia and hypophosphatemia. (27) Clinical manifestations described range from gastrointestinal symptoms of nausea, vomiting and diarrhea to musculoskeletal symptoms such as cramps and tremors to arrhythmias, seizures and pulmonary edema. (28-30) Apparently the pathophysiological process by which hypomagnesaemia occurs is a class effect that is related to alteration of gastrointestinal absorption of this ion. (30) The duration of treatment is likely to be a risk factor since the majority of cases reported have been in people who used PPIs for more than one year, although this condition has also been reported with three-month treatments. (30) The FDA recommends testing serum magnesium prior to the initiation of long-term therapy (greater than 1 year) or initiation of concurrent medication with other hypomagnesemia-related medications such as diuretics and digoxin. (31).
Inhibition of Iron Absorption
Iron is present in the diet in two forms: ferrous iron which easily absorbed, and ferric iron which cannot be directly absorbed but must first be transformed into the ferrous form through a reaction dependent on acid pH. Current evidence about the relationship between PPIs and iron deficiency is supported by cases of patients with iron deficiency anemia who did not respond to supplements until PPIs were discontinued. In addition, there have been reports of hematological changes indicating iron deficiency in patients who have taken PPIs for more than 1 year, and of patients with hereditary hemochromatosis who, after long-term PPI use, showed a significant reduction in phlebotomy requirements. (32) However, no decreases in body iron stores were found in a study of patients who consumed omeprazole for more than 4 years and others with Zollinger-Ellison syndrome treated with PPIs for 6 years. (33) Current results suggest that, although a relationship is theoretically possible, it has not been clinically demonstrated and is unlikely to be of significance in patients with normal iron stores. (32)
Risk of Gastrointestinal Neoplasms
Prolonged treatment with PPIs raises gastric pH which increases gastrin secretion and plasma levels. The trophic effects of gastrin lead to hyperplasia of enterochromaffin-like cells. For this reason it has been suggested that treatment with PPIs could lead to development of gastric polyps, gastric cancer, colorectal cancer and/or carcinoid tumors. (33) Some data suggest an increased risk of atrophic gastritis, especially in people with H. pylori. However, there is insufficient evidence of progression to malignant disease. (33) A 2013 metaanalysis of six randomized clinical trials evaluated the risk of premalignant or malignant lesions with the use of PPIs for more than 6 months, but found no associations even in patients with gastroesophageal reflux disease and maintenance therapy. (34)
A 15-year follow-up study has shown that long-term PPI therapy at regular doses is not associated with a significantly increased risk of colorectal cancer. (35) At present, there is no clinical evidence of increased risk of gastric or colon malignant or premalignant lesions, but there are no epidemiological studies that have evaluated potential associations between PPI treatment and the risks of cancer of the esophagus, cancer of the pancreas or carcinoid tumors.
Spontaneous Bacterial Peritonitis in Patients with Cirrhosis
It has been suggested that PPIs may increase the risk of infections in patients with cirrhosis and predispose them to spontaneous bacterial peritonitis (SBP) due to increased intestinal permeability and increased bacterial growth. (36) Evidence is based on retrospective studies of cirrhotic patients hospitalized with ascites. For these patients, recent use of PPI was independently associated with SBP but there were no changes in one month, three month, or one year survival rates. (36) In 2012, Goel et al. also found that incidence of SBP was significantly more likely among patients who had recently used PPIs (in the previous seven days) (71.0%) than among control patients (42.0%). However, they also showed that there was no difference between patients who had received PPIs eight to ninety days previously from those who had not used them (p = 0.58) (37). In 2014, Kwon et al. found that both PPI therapy and H2 antagonists were associated with SBP and that PPI use in the previous 30 days was associated with higher mortality rates, independent of the severity of baseline liver disease (OR: 1.96, 95% CI: 1.19-3.22, p = 0.008). (38) In contrast, in 2012 Bajaj et al. found no association between PPI use and the rate of serious infections (HR: 1.08; 95% CI: 0.90-1.31) (39). Due to the lack of conclusive information, no conclusions can be drawn in about any association between the use of PPIs and SBP.
Leukopenia, Neutropenia and Agranulocytosis
Associations between leukopenia, neutropenia, or agranulocytosis and PPIs have not been well described in the literature. It has been argued that these associations may be explained by immunological reactions or by direct toxicity, and it has been suggested that they may be a class effect. However, other assumptions suggest a different mechanisms according to the PPI considered. (40) More studies are needed to clarify the cause-effect relationship of this association.
Conclusion
Although an association between PPI consumption and several long-term ADRs has been suggested, the quality of the evidence supporting increased risks in each case is heterogeneous and, in many cases, of marginal quality. Nevertheless, there are b and important associations with increased risk of osteopenia, osteoporosis, fractures and nosocomial pneumonia. Given their impact on long-term outcomes, clinicians should be alert to the need to balance the risks, costs and benefits involved in the sue of PPIs.
It should be borne in mind that indiscriminate use, above all when there are no indications, of therapeutic measures increases the risk of undesirable events and the appearance of even infrequent reactions. Therefore, the administration of PPIs should be guaranteed only for those patients with a clear indication supported by the evidence, and the drug should be suspended when necessary.
REFERENCES
1. Vakil N. Prescribing proton pump inhibitors: is it time to pause and rethink? Drugs. 2012; 72(4):437-45. [ Links ]
2. Batuwitage BT, Kingham JG, Morgan NE, et al. Inappropriate prescribing of proton pump inhibitors in primary care. Postgrad Med J 2007; 83(975): 66-8. [ Links ]
3. Ramirez E, Lei SH, Borobia AM, et al. Overuse of PPIs in patients at admission, during treatment, and at discharge in a tertiary Spanish hospital. Curr Clin Pharmacol 2010; 5(4): 288-97. [ Links ]
4. Chubineh S, Birk J. Proton Pump Inhibitors: The Good, the Bad, and the Unwanted. South Med J. 2012; 105(11):613-8. [ Links ]
5. Gilard M, Arnaud B, Le Gal G, et al. Influence of omeprazol on the antiplatelet action of clopidogrel associated to aspirin. J Thromb Haemost. 2006; 4(11):2508-9. [ Links ]
6. Bhatt DL, Cryer BL, Contant CF, et al. Clopidogrel with or without omeprazole in coronary artery disease. N Engl J Med. 2010; 363(20):1909-17. [ Links ]
7. Vaduganathan M, Cannon CP, Cryer BL, Liu Y, Hsieh WH, Doros G, et al. Efficacy and Safety of Proton-Pump Inhibitors in High-Risk Cardiovascular Subsets of the COGENT Trial. Am J Med. 2016. [ Links ]
8. Huang B, Huang Y, Li Y, et al Adverse cardiovascular effects of concomitant use of proton pump inhibitors and clopidogrel in patients with coronary artery disease: a systematic review and meta-analysis. Arch Med Res. 2012; 43(3):212-24. [ Links ]
9. Kwok CS, Jeevanantham V, Dawn B, et al. No consistent evidence of differential cardiovascular risk amongst proton-pump inhibitors when used with clopidogrel: meta-analysis. Int J Cardiol. 2013; 167(3):965-74. [ Links ]
10. Ngamruengphong S, Leontiadis GI, Radhi S, et al. Proton pump inhibitors and risk of fracture: a systematic review and meta-analysis of observational studies. Am J Gastroenterol. 2011; 106(7):1209-18. [ Links ]
11. Arj A, Razavi Zade M, Yavari M, et al. Proton pump inhibitors use and change in bone mineral density. Int J Rheum Dis. 2016. [ Links ]
12. Kwok CS, Yeong JK, Loke YK. Meta-analysis: risk of fractures with acid-suppressing medication. Bone. 2011; 48(4):768-76. [ Links ]
13. Williams C, McColl KE. Review article: proton pump inhibitors and bacterial overgrowth. Aliment Pharmacol Ther. 2006; 23(1):3-10. [ Links ]
14. Proton pump inhibitors: bacterial pneumonia. Prescrire Int. 2012; 21(130):210-2. [ Links ]
15. Giuliano C, Wilhelm SM, Kale-Pradhan PB. Are proton pump inhibitors associated with the development of community-acquired pneumonia? A meta-analysis. Expert Rev Clin Pharmacol. 2012; 5(3):337-44 [ Links ]
16. Eom CS, Jeon CY, Lim JW, et al. Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis. CMAJ. 2011; 183(3):310-9. [ Links ]
17. Lin PC, Chang CH, Hsu PI, et al. The efficacy and safety of proton pump inhibitors vs histamine-2 receptor antagonists for stress ulcer bleeding prophylaxis among critical care patients: a meta-analysis. Crit Care Med 2010; 38(4):1197-205. [ Links ]
18. Bavishi C, Dupont HL. Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment Pharmacol Ther 2011; 34(11-12):1269-81. [ Links ]
19. Kwok CS, Arthur AK, Anibueze CI, et al. Risk of Clostridium difficile infection with acid suppressing drugs and antibiotics: meta-analysis. Am J Gastroenterol 2012; 107(7):1011-9. [ Links ]
20. Tleyjeh IM, Bin Abdulhak AA, Riaz M, et al. Association between proton pump inhibitor therapy and clostridium difficile infection: a contemporary systematic review and meta-analysis. PLoS One.2012; 7(12):e50836. [ Links ]
21. Gill SK, OBrien L, Einarson TR, et al. The safety of proton pump inhibitors in pregnancy: a meta-analysis. Am J Gastroenterol. 2009; 104(6):1541-5. [ Links ]
22. Hak E, Mulder B, Schuiling-Veninga CC, et al. Use of Acid-Suppressive Drugs in Pregnancy and the Risk of Childhood Asthma: Bidirectional Crossover Study using the General Practice Research Database. Drug Saf. 2013; 36(11):1097-104. [ Links ]
23. Klepser DG, Collier DS, Cochran GL. Proton pump inhibitors and acute kidney injury: a nested case-control study. BMC Nephrol. 2013; 14(1):150. [ Links ]
24. den Elzen WP, Groeneveld Y, de Ruijter W, et al. Long-term use of proton pump inhibitors and vitamin B12 status in elderly individuals. Aliment Pharmacol Ther. 2008; 27(6):491-7. [ Links ]
25. Rozgony NR, Fang C, Kuczmarski MF, et al. Vitamin B(12) deficiency is linked with long-term use of proton pump inhibitors in institutionalized older adults: could a cyanocobalamin nasal spray be beneficial? J Nutr Elder. 2010; 29(1):87-99. [ Links ]
26. Damiao CP, Rodrigues AO, Pinheiro MF, et al. Prevalence of vitamin B12 deficiency in type 2 diabetic patients using metformin: a cross-sectional study. Sao Paulo Med J. 2016. [ Links ]
27. Epstein M, McGrath S, Law F. Proton-pump inhibitors and hypomagnesemic hypoparathyroidism. N Engl J Med. 2006; 355(17):1834-6. [ Links ]
28. Mackay JD, Bladon PT. Hypomagnesaemia due to proton-pump inhibitor therapy: a clinical case series. QJM. 2010; 103(6):387-95. [ Links ]
29. Hoorn EJ, van der Hoek J, de Man RA, et al. A case series of proton pump inhibitor-induced hypomagnesemia. Am J Kidney Dis. 2010; 56(1):112-6. [ Links ]
30. Florentin M, Elisaf MS. Proton pump inhibitor-induced hypomagnesemia: A new challenge. World J Nephrol. 2012; 1(6):151-4. [ Links ]
31. U.S. Food and Drug Administration. FDA Drug Safety Communication: Low magnesium levels can be associated with long-term use of Proton Pump Inhibitor drugs (PPIs) http://www.fda.gov/drugs/drugsafety/ucm245011.htm2011 [cited 2014 02/09] [ Links ].
32. Reimer C. Safety of long-term PPI therapy. Best Pract Res Clin Gastroenterol. 2013; 27(3):443-54 [ Links ]
33. Yang YX, Metz DC. Safety of proton pump inhibitor exposure. Gastroenterology. 2010; 139(4):1115-27. [ Links ]
34. Eslami L, Nasseri-Moghaddam S. Meta-analyses: does long-term PPI use increase the risk of gastric premalignant lesions? Arch Iran Med. 2013; 16(8):449-58. [ Links ]
35. Robertson DJ, Larsson H, Friis S, et al. Proton pump inhibitor use and risk of colorectal cancer: a population-based, case-control study. Gastroenterology. 2007; 133(3):755-60. [ Links ]
36. Trikudanathan G, Israel J, Cappa J, et al. Association between proton pump inhibitors and spontaneous bacterial peritonitis in cirrhotic patients – a systematic review and meta-analysis. Int J Clin Pract. 2011; 65(6):674-8. [ Links ]
37. Goel GA, Deshpande A, Lopez R, et al. Increased rate of spontaneous bacterial peritonitis among cirrhotic patients receiving pharmacologic acid suppression. Clin Gastroenterol Hepatol. 2012; 10(4):422-7. [ Links ]
38. Kwon JH, Koh SJ, Kim W, et al. Mortality associated with proton pump inhibitors in cirrhotic patients with spontaneous bacterial peritonitis. J Gastroenterol Hepatol. 2014; 29(4):775-81. [ Links ]
39. Bajaj JS, Ratliff SM, Heuman DM, et al. Proton pump inhibitors are associated with a high rate of serious infections in veterans with decompensated cirrhosis. Aliment Pharmacol Ther. 2012; 36(9):866-74. [ Links ]
40. Gouraud A, Vochelle V, Descotes J, et al. Proton pump inhibitor-induced neutropenia: possible cross-reactivity between omeprazole and pantoprazole. Clin Drug Investig. 2010; 30(8):559-63. [ Links ]











 text in
text in