Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.4 Bogotá Oct./Dec. 2016
Sarcopenic dysphagia
Daniela Patino-Hernandez MD (1,3), Miguel Germán Borda MD (1,2,3), Â Luis Carlos Venegas Sanabria MD (1, 2, 3)
Diego Andrés Chavarro-Carvajal MD (1, 2, 3), Carlos Alberto Cano-Gutiérrez MD (1, 2, 39
(1) Instituto de Envejecimiento, Facultad de Medicina, Pontificia Universidad Javeriana. Bogotá, Colombia.
(2) Unidad de Geriatría, Hospital Universitario San Ignacio, Bogotá, Colombia.
(3) Semillero de Investigación en Neurociencias y Envejecimiento, Pontificia Universidad Javeriana. Bogotá, Colombia.
Received:Â Â Â 08-03-16 Â Accepted:Â Â Â 01-11-16
Abstract
Sarcopenic dysphagia is a swallowing difficulty associated with loss of mass, strength and generalized muscular function. Its prevalence is higher among elderly patients and those with malnutrition or with disuse of the swallowing musculature. It is associated with adverse outcomes such as aspiration pneumonia and accumulation of waste in the oropharyngeal cavity after swallowing as well as with poor quality of life and prolonged hospital stays. A review of the literature available on the subject was done in order to provide a guide for early detection and management of this clinical entity which is needed for clinical practice.
Keywords
Swallowing disorders, sarcopenia, aging.
Introduction
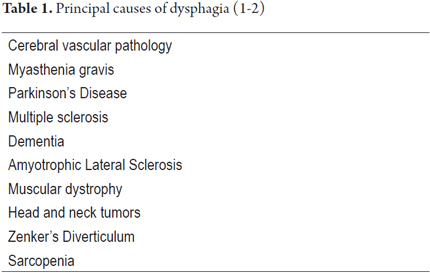
Dysphagia affects 11.4% to 38% of the elderly in the community and 40% to 68% of the elderly in long-stay units. (1) Its frequency and severity increase in association with chronic diseases related to age. (2, 3) Dysphagia can be divided into two major groups: esophageal dysphagia and oropharyngeal dysphagia. Esophageal dysphagia is caused by conditions that compromise the structure or function of the esophagus while oropharyngeal dysphagia is a disorder of gastrointestinal motility. (4) It makes it difficult or impossible to move food bolus safely from the mouth to the esophagus and can lead to tracheobronchial aspiration. There is a constellation of heterogeneous etiologies that can cause oropharyngeal dysphagia, the most important of which are listed in Table 1. (5) Â
Several head and neck muscles are used simultaneously and in conjunction to coordinate swallowing. Any reduction of muscle mass or strength of these muscles can potentially have an impact on the swallowing function. (6) Sarcopenia is a geriatric syndrome that has been defined by the European Working Group on Sarcopenia in Older People (EWSGOP) as decreasing strength, function and generalized muscle mass and as a potential cause of dysphagia. (7)
Both dysphagia and sarcopenia are common in the elderly population, but patients with sarcopenia may or may not suffer from dysphagia. (1) Dysphagia can trigger or promote fragility in elderly people. In addition, there is a clear relationship between changes in nutritional status and adverse health outcomes in this population. (3) Hence, detection and management of this pathology are both important.
Definition
To define sarcopenic dysphagia it is necessary to differentiate among dysphagia, presbyphagia and sarcopenic dysphagia proper (8). Dysphagia is defined as any disruption in the swallowing process which occurs as the result of physiological or anatomical changes in the mouth, pharynx, larynx or esophagus. (3)
Presbyphagia includes all age-related changes in the swallowing mechanism. These changes can be caused by difficulty in forming and propelling a bolus, a decrease in the pressure of the tongue, obstruction of the passage of the bolus, stoppage of the bolus when swallowing, a decrease in the sensation of smell and taste (which makes swallowing more difficult), and loss of teeth. All these can also make mastication difficult (9).
Sarcopenic dysphagia, although also associated with age, (10) is diagnosed when there is also difficulty in swallowing due to sarcopenia in the masticatory muscles and other groups of the skeletal musculature. It is characterized by loss of muscle mass and strength of the swallowing muscles including the intrinsic muscle of the tongue and mimetic, masticatory, suprahyoid, infrahyoid, palatine, pharyngeal and esophageal muscles. (1)
Causes
The risk of dysphagia increases with age so much so that prevalence is as high as 74% among elderly people living in long-stay units. (11). The reduction of muscle mass and the elasticity of connective tissue associated with age leads to loss of strength and range of motion of the tongue and other muscles involved in swallowing which negatively affects the swallowing process. (12)
The most frequent cause of oropharyngeal dysphagia is cerebrovascular disease in which case physicians routinely check for swallowing disorders according to protocol. However, this does not occur with sarcopenic dysphagia: it is rarely diagnosed because it has neither defined diagnostic criteria nor standardized methods of evaluation. (1)
The tongue plays a fundamental role in swallowing: it is responsible for formation, movement and manipulation of the bolus. For this reason evaluation of the muscles of the tongue is important for evaluation of swallowing. A study by Maeda et al. has evaluated the relationships among tongue pressure, aging, nutrition, performance of basic activities of daily life and the appearance of sarcopenic dysphagia. The study found that decreased maximum voluntary pressue pressure and dysphagia are related to sarcopenia. (13)
Another study by Shiozu et al. showed that the swallowing function, nutritional status and level of basic daily life activities among elderly patients who had sarcopenia were all significantly lower than among elderly patients without sarcopenia. (14)
Sarcopenia can cause dysphagia, but dysphagia can also cause sarcopenia by decreasing the dietary supply of amino acids. Once lingual atrophy occurs, secondary malnutrition develops and perpetuates the condition. (12-15) This occurs because swallowing muscles are formed primarily from type II muscle fibers which are more bly affected by malnutrition and sarcopenia than are type I fibers. (16) In addition, prolonged hospitalizations and consequent periods of immobility, sometimes combined with fasting, accelerate muscle atrophy through disuse which increases sarcopenia. (3) Nevertheless, it has also been observed that sarcopenia is associated with dysphagia among people with no relevant pathological antecedents. As a result, the actual prevalence of sarcopenic dysphagia is unknown. (6)
Consequences
Dysphagia has two principal functional outcomes: aspiration, when food or liquid enters the airway, and accumulation of debris in the throat after swallowing. (17) This increases the likelihood of clogging and aspiration and also of bacterial colonization.
Aspiration pneumonia is a very common complication in patients with oropharyngeal dysphagia: it has been reported in up to 50% of patients in the first year and has a mortality rate close to 45%. (4-10). Weight loss secondary to low intake of food in patients with dysphagia increases the risk of opportunistic infections. (3) When there are signs of possible malignancy such as sudden weight loss, dysgeusia or hemorrhaging in a patient with dysphagia, the patient should be referred for evaluation by otolaryngology. (4) Malnutrition is secondary to limited intake of liquids and food, (18) and decreased intake may also alter the level of consciousness, generate physical weakness and cause poor coordination of the swallowing mechanism. (3)
Other complications associated with dysphagia include hydroelectrolytic disorders, dehydration and cramping. (2, 13, 18, 19) Even mild to moderate dysphagia affects the quality of life of the individual who suffers from it: mild dysphagia causes discomfort and a high probability of cramping which can cause embarrassment, prevent afflicted individuals from feeling comfortable eating in public and reduce the pleasure of eating. (20-22)
In addition, it has a significant impact on the lengths of hospital stays and is an indicator of poor prognosis. (2)
Detection
Diagnosis of sarcopenic dysphagia requires appropriate clinical judgment by a geriatrician and a gastroenterologist who must know about, and be familiar with, this entity. Their evaluations require exhaustive study of dysphagia and sarcopenia. (7, 23)
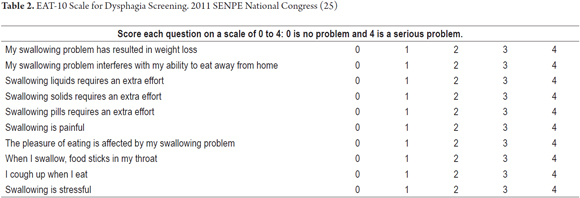
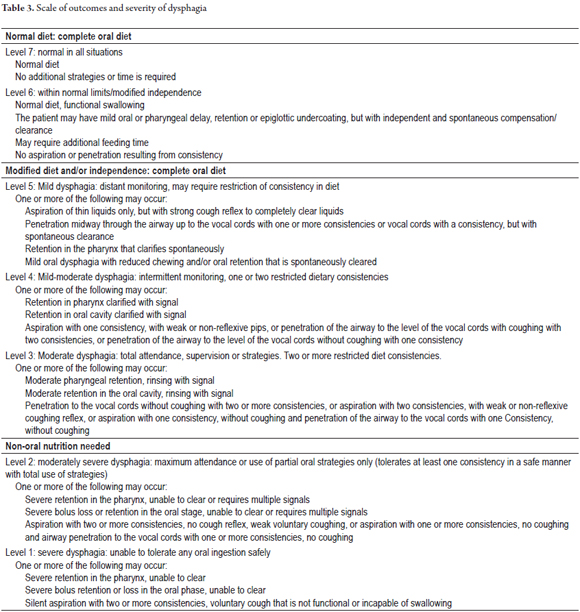
Screening, physical examinations and complementary tests can all play roles in diagnosis of dysphagia. Several screening tools have been proposed. One of them is the EAT-10 (the 10 item eating assessment tool). This is a questionnaire with ten questions associated with dysphagia. Respondents score each question on a 0 to 4 scale within which 0 signifies "without difficulty" and 4 signifies "severe problem". A score of 3 or greater suggests swallowing problems (Table 2). (24) This scale has been translated and validated in Spanish and is a good predictor of the risk of aspiration in people with dysphagia. (24, 25) Another scoring system is called the dysphagia severity scale. This is a 7 level scale within which higher levels indicate lesser degrees of compromise of the swallowing function. A score of 1 to 6 indicates dysphagia, whereas a score of 1 to 4 also suggests aspiration (Table 3). (26)
Finally, there are other screening methods for dysphagia such as tests of swallowing water or food, pulse oximetry, and cervical auscultation. (1) The volume-to-viscosity clinical exploration method evaluates both the efficacy and safety of the swallowing function. (5) Once a positive result has been obtained from these tests, it is important conduct videofluoroscopy and/or videoendoscopic evaluations.
On the other hand, sarcopenia should be evaluated according to the diagnostic criteria defined by the EWSGOP mentioned above. (7) Muscle mass is evaluated by DEXA (dual energy X-ray absorptiometry), bioelectrical impedance analysis (BIA), CT scan, MRI, ultrasonography or anthropometry (perimeter of calf or arm). Muscular strength is evaluated through manual dynamometry or measurement of flexion and extension of the knee. Muscle function is measured through gait speed, the get-up-and-go test, or short battery of physical performance. (7)
Sarcopenia of the muscles involved in swallowing can be assessed by measuring the muscle mass of the geniohyoid muscle, by measuring the width of the tongue, or by lifting the head. (18) Tamura and colleagues described the measurement of the width of the central portion of the tongue through ultrasonography as an indirect way to measure lingual sarcopenia. This technique is useful because it is easy and is not invasive. (12) Another method of detection described by Yoshida et al. is measurement of lingual pressure in patients who can communicate. (13) Although decreased lingual pressure is associated with age, it has been suggested that the underlying mechanism may be sarcopenia in the musculoskeletal system of the head and neck. In addition, lower tongue pressure is associated with decreases in the cough reflex to avoid asphyxia, which is why evaluation is important. (13)
Computed axial tomography (CT) to measure swallowing muscle mass has also been described. Feng et al. found that the area of the cross-section of ââthe geniohyoid muscle decreases in proportion to a person's age, and that this diameter is smallest in patients who suffer aspiration. (27) Nevertheless, standardized methods for adequate measurement have not yet been clearly elucidated in the literature. (1)
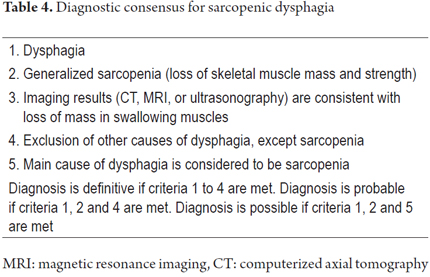
On the other hand, during the Nineteenth Annual Meeting of the Japanese Society of Dysphagia Rehabilitation a consensus was reached regarding diagnostic criteria for sarcopenic dysphagia. The following factors are considered:
1. Presence of dysphagia
2. Presence of generalized sarcopenia
3. Consistent imaging with loss of muscle mass
4. Exclusion of causes of dysphagia other than sarcopenia
5. The main cause of dysphagia is considered to be sarcopenia if there are co-morbidities causing sarcopenia.
A diagnosis of sarcopenic dysphagia is definitive if criteria 1 to 4 are met, a diagnosis is likely if criteria 1, 2 and 4 are met, and a diagnosis of sarcopenic dysphagia is possible if criteria 1, 2 and 5 are met (Table 4). (1)
Treatment
Both sarcopenia and dysphagia should be treated for proper management of sarcopenic dysphagia. Dysphagia rehabilitation should include oral health care (brushing of postprandial teeth, appropriate cleaning of dental prostheses, etc.) because it contributes to reduced incidence of aspiration pneumonia. (28) Although the effectiveness of dysphagia rehabilitation techniques appears to be limited, muscular strength training of the swallowing muscles is of great importance. (29) Similarly, the technique of head elevation improves the swallowing function and symptoms of dysphagia. (30)
In addition, it compensatory procedures such as the modification of the texture of solid foods and the thickness of liquids can be implemented. (27) Foods can be cut into small pieces or puréed, while liquids can be thickened to slow transit through the oral and pharyngeal phases of swallowing to avoid aspiration. (1)
Finally, sarcopenia should be treated with a combination of rehabilitation training and nutrition. The type of feeding should be based on the causes of malnutrition, sarcopenia and dysphagia for each individual patient. (16) Although the type of exercise recommended for patients with sarcopenia is still under discussion, an essential component is a minimum of three 30 minute sessions every week. It has also been suggested that physical exercise has a role beyond simply increasing muscle mass because it generates a reduction of inflammation, helps infiltration of fat into the muscles, and increases the presence of muscle satellite cells. (31) Dietary supplements that include amino acids or protein before exercise has also been described, and avoidance of cigarette smoking is recommended. In addition, underlying pathologies that cause or worsen sarcopenic dysphagia should be treated. (1)
Conclusions
Sarcopenic dysphagia is a common clinical entity whose prevalence increases as the average age of population increases. It is associated with risks of malnutrition, aspiration pneumonia, hydroelectrolytic disorders, poorer quality of life and longer hospital stays. Therefore, early detection and timely intervention is necessary to reduce morbidity and mortality in the elderly population.
REFERENCES
1. Wakabayashi H. Presbyphagia and sarcopenic dysphagia: association between aging, sarcopenia, and deglutition disorders. J Frailty Aging. 2014;3:97-103. [ Links ]
2. Altman KW, Yu GP, Schaefer SD. Consequence of dysphagia in the hospitalized patient. Dysphagia. 2011;26(2):200-1. [ Links ]
3. Sura L, Madhavan A, Carnaby G, et al. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012;7:287-98. [ Links ]
4. Khan A, Carmona R, Traube M. Dysphagia in the elderly. Clin Geriatr Med. 2014;30(1):43-53. [ Links ]
5. Pérez Díaz DS, Ortega Fernández O, Cabré Roure M, et al. Disfagia orofaríngea en el anciano. En: Abizanda Soler P, Rodríguez Mañas L (editores). Tratado de medicina geriátrica. Fundamentos de la atención sanitaria a los mayores. España: Elsevier; 2015. p. 237-44. [ Links ]
6. Maeda K, Akagi J. Sarcopenia is an independent risk factor of dysphagia in hospitalized older people. Geriatr Gerontol Int. 2016;16(4):515-21. [ Links ]
7. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412-23. [ Links ]
8. Jahnke V. Dysphagia in the elderly. HNO. 1991;39(11):442-4. [ Links ]
9. Humbert IA, Robbins J. Dysphagia in the elderly. Phys Med Rehabil Clin N Am. 2008;19(4)853.66. [ Links ]
10. Cabre M, Serra-Prat M, Palomera E, et al. Prevalence and prognostic implications of dysphagia in elderly patients with pneumonia. Age Ageing. 2010;39(1):39-45. [ Links ]
11. Namasivayam AM, Steele CM. Malnutrition and dysphagia in long-term care: a systematic review. J Nutr Gerontol Geriatr. 2015;34(1):1-21. [ Links ]
12. Tamura F, Kikutani T, Tohara T, et al. Tongue thickness relates to nutritional status in the elderly. Dysphagia. 2012;27(4):556-61. [ Links ]
13. Yoshida M, Kikutani T, Tsuga K, et al. Decreased tongue pressure reflects symptom of dysphagia. Dysphagia. 2006;21(1):61-5. [ Links ]
14. Shiozu H, Higashijima M, Koga T. Association of sarcopenia with swallowing problems, related to nutrition and activities of daily living of elderly individuals. J Phys Ther Sci. 2015;27(2):393-6. [ Links ]
15. Carrier N, Ouellet D, West GE. Nursing home food services linked with risk of malnutrition. Can J Diet Pract Res. 2007;68(1):14-20. [ Links ]
16. Wakabayashi H, Sakuma K. Rehabilitation nutrition for sarcopenia with disability: a combination of both rehabilitation and nutrition care management. J Cachexia Sarcopenia Muscle. 2014;5(4):269-77. [ Links ]
17. Rofes L, Arreola V, Almirall J, et al. Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterol Res Pract. 2011;2011:13. [ Links ]
18. Fund TC. Malnutrition and dehydration in nursing homes. Health Care Food Nutr Focus. 2000;17(386):3-7. [ Links ]
19. Amaral TF, Matos LC, Teixeira MA, et al. Undernutrition and associated factors among hospitalized patients. Clin Nutr. 2010;29(5):580-5. [ Links ]
20. Hewitt A, Hind J, Kays S, et al. Standardized instrument for lingual pressure measurement. Dysphagia. 2008;23(1):16-25. [ Links ]
21. Ickenstein GW, Riecker A, Höhlig C, et al. Pneumonia and in-hospital mortality in the context of neurogenic oropharyngeal dysphagia (NOD) in stroke and a new NOD step-wise concept. J Neurol. 2010;257(9):1492-9. [ Links ]
22. Farri A, Accornero A, Burdese C. Social importance of dysphagia: its impact on diagnosis and therapy. Acta Otorhinolaryngol Ital. 2007;27(2):83-6. [ Links ]
23. Swigert NB, Steele C, Riquelme LF. Dysphagia screening for patients with stroke: challenges in implementing a Joint Commission Guideline. ASHA Lead. 2007;12(3):4-29. [ Links ]
24. Belafsky PC, Mouadeb DA, Rees CJ, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117(12):919-24. [ Links ]
25. Burgos R, Sarto B, Segurola H, et al. Translation and validation of the Spanish version of the EAT-10 (Eating Assessment Tool-10) for the screening of dysphagia. Nutr Hosp. 2012;27(6):2048-54. [ Links ]
26. ONeil KH, Purdy M, Falk J, et al. The dysphagia outcome and severity scale. Dysphagia. 1999;14(3):139-45. [ Links ]
27. Feng X, Todd T, Lintzenich CR, et al. Aging-related geniohyoid muscle atrophy is related to aspiration status in healthy older adults. J Gerontol A Biol Sci Med Sci. 2013;68(7):853-60. [ Links ]
28. Van Der Maarel-Wierink CD, Vanobbergen JNO, Bronkhorst EM, et al. Oral health care and aspiration pneumonia in frail older people: A systematic literature review. Gerodontology. 2013;30(1):3-9. [ Links ]
29. Antunes EB, Lunet N. Effects of the head lift exercise on the swallow function: A systematic review. Gerodontology. 2012;29(4):247-57. [ Links ]
30. Robbins J, Gangnon RE, Theis SM, et al. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53(9):1483-9. [ Links ]
31. Phu S, Boersma D, Duque G. Exercise and sarcopenia. J Clin Densitom. 2015;18(4):488-92. [ Links ]











 text in
text in