Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.32 no.1 Bogotá Jan./Mar. 2017
https://doi.org/https://doi.org/10.22516/25007440.125
Factors Associated with Conversion of Laparoscopic Colecistectomy to Open Colescytectomy
Ledmar Vargas R (1), Milena Agudelo S. (1) Roger Lizcano C. (1), Melissa Martínez B. (1), Leonardo Velandia B. (1), Sergio Sánchez H. (1), Óscar Jiménez P. PhD. (2), Marco Quintero MD (3)
(1) Medical student at the University of Boyacá in Tunja, Colombia
(2) Dentistry PhD, Chief of the Department of Public Health and Full Professor at the University of Boyacá in Tunja, Colombia
(3) Intensive Care Specialist, General Surgeon, Fellow in Hepato-pancreato-biliary Surgery at the Regional Hospital of Sogamoso in Sogamoso, Colombia
Received:Â Â Â 31-05-16 Â Â Accepted:Â Â Â 16-12-16
Abstract
Introduction: Acute cholecystitis is an inflammation of the vesicular wall whose treatment is purely surgical: a laparoscopic cholecystectomy is the procedure of choice. This can be converted intraoperatively due to complications of the intervention, patient factors or factors associated with the surgeon. The aim of this study was to establish the frequency and the association of conversions of laparoscopic cholecystectomies based on hematological laboratory tests and abdominal ultrasound as well as sociodemographic factors.
Materials and Methods: This is a descriptive, cross-sectional, observational and retrospective study that was carried out from January 1 to November 3, 2015. Clinical histories of patients who had been with diagnosed with benign vesicular pathologies who underwent vesicular surgical procedures were reviewed.
Results: Of the cases reviewed, 35.5% patients underwent laparoscopic cholecystectomies, and of these cases 42.8% of the procedures were converted to conventional surgery. The majority of the patients were women (72.8%), but conversions were most frequent among men. The most frequent preoperative diagnosis was cholelithiasis (98.3%). Age greater than 50 years presented an odds ratio of 0.55, while leukocytosis had an odds ratio of 0.40, both variables were statistically significant (P = <0.05).
Conclusions: It was determined that ages over 50 years and/or a leukocyte count over 10,000 mm3 are risk factors for failure of laparoscopic cholecystectomies. In addition, factors related to the surgeon must be taken into account.
Key Words
Cholecystectomy, laparoscopic cholecystectomy, leukocytes, conversion to open surgery, complications
INTRODUCTION
Worldwide, acute cholecystitis, an inflammation of the vesicular wall, is the second most common cause of acute abdomen. It is one of the primary reasons patients visit emergency rooms. About 95% of all cases are due to lithiasis. (1) The only treatment for this pathology is surgery, (2) and laparoscopic cholecystectomy (LC) is the procedure of choice. (3) During the procedure, laparoscopy can be converted into open surgery depending on whether complications develop and patients related to the patient and to the surgeon. (4)
In Latin America, the frequency of conversion from LC to open cholecystectomy varies from 10% to 20%. (5) The percentage of conversion to open surgery in the United States is 4.6% in elective surgery and 9.4% in emergency surgery. (6) In Colombia, some studies indicate that conversion occurs in between 0.8% and 12% of cases. (7, 8)
There are multiple predictive factors of conversion including patient age, pathologies, previous surgery, and leukocyte count. (8) A study carried out at San Ignacio University Hospital in Bogotá found that risk factors for LC conversion were leukocyte counts over 10,000 per mm3 and patient age over 50 years. (7)
Other studies have determined that C-reactive protein (CRP) predicts conversion risk. (9-11) Ultrasound may be of vital importance for determining the difficulty of surgery, (12, 13) and training of health care personnel may increase the likelihood of intraoperative alteration, (14) The most important complications that can occur in a conversion include infection of the surgical wound, postoperative hernias and adhesions. 6)
We conducted this study to establish the frequency of LC conversions and risk factors associated with open cholecystectomy based on laboratory blood tests, abdominal ultrasound and sociodemographic factors reported in the medical histories of the patients.
MATERIALS AND METHODS
This is a descriptive, cross-sectional, observational and retrospective study that was carried out from January 1 to November 3, 2015. A total of 71 clinical histories for patients who had been diagnosed with benign vesicular pathologies and who had undergone vesicular surgical procedures at the Regional Hospital of Sogamoso were included. Various factors involved in LC conversion to open surgery were described, compared and analyzed. Non-probabilistic sampling was used for convenience. Patients who had been diagnosed with benign biliary disease, undergone cholecystectomies, had laboratory results including acute phase reactants such as leukocytes, and had imaging results recorded in their clinical histories were included.
Exclusion criteria were incomplete data and previous abdominal surgery in other hospitals.
Study variables selected included each patient's sex, age, preoperative diagnosis, laboratory tests including PCR, total and differential bilirubin, and alkaline phosphatase, and intraoperative complication. After study variables had been chosen, data were collected from the clinical records and a database was created in Excel 2007.
Statistical analysis
Data were presented in tables containing absolute and relative frequencies (percentages). Univariate and bivariate relative risk descriptive statistical analysis was performed to determine risk factors associated with the conversion of LC to open surgery. We used Excel 2007 for the database and SPSS statistics 22 to determine relative risks.
Ethical Considerations
According to the criteria for health research established in Resolution 8430 of 1993, this is a risk-free investigation. In addition, after the Ethics Committee of the Hospital had evaluated and analyzed the study, it decided to approve informed consent for the review of medical records and the subsequent publication of results.
RESULTS
Of the total of 71 clinical histories reviewed, 12 were excluded because they did not meet the inclusion criteria. The management of all patients was surgical. LCs were performed in 35.5% of the patients and of these, 42.8% were converted to conventional surgery. The reasons for conversion reported in the surgical reports were epiploic adhesions (66.6%), cysts could not be seen (11.1%), vesicular aggregates (11.1%); and cystic fistulas (11.1%).
The majority of patients who underwent surgery were women (72.8%), but conversion to open cholecystectomies was much more common in men: 100% compared to only 36.8% of the women.
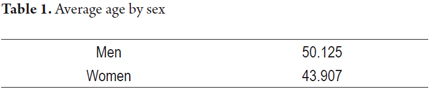
The mean age was 45.6 years (Table 1) and preoperative diagnoses were cholelithiasis (98.3%), acute cholecystitis (38.9%), choledocholithiasis (6.7%) and others (37.8%). A patient could have multiple diagnoses of benign gallbladder disease: only 32.2% presented just one pathology and the remaining 67.8% had concomitant pathologies of which almost half (45.7% %) exhibited two pathologies.
Of the pathologies mentioned above, the highest percentage of conversions was found in patients with acute cholelithiasis (100%) followed by acute cholecystitis with 44.4%. The diagnosis of cholelithiasis was made through abdominal ultrasound in 100% of the patients studied. In addition, abdominal ultrasound was also used to measure gallstones. The smallest was only 1 mm in diameter, and the largest had a 42 mm diameter. There was no significant relationship between the size of the calculi and surgical difficulty, since the mean size of calculi was 15.5 mm in patients whose LCs were converted into open surgery while the mean diameter of the rest was 15.6 mm. Abdominal ultrasound was used to diagnose 26.09% of the cases of acute cholecystitis. Use of the Tokyo criteria increased sensitivity to 85%Â allow us to determine that 71% were cases of grade II (moderate acute) cholecystitis which indicated serious inflammation which could make the surgeon's task more difficult.
Statistical analysis of bivariate relative risk yielded important results. Patients aged over 50 years were 55% more likely have LC converted to open surgery (odds ratio [OR] = 0.55) which was statistically significant (p <0.05). In addition, according to laboratory results, 88.9% of the converted patients had leukocytosis with leukocyte levels over than 10,000 per mm3 indicating that patients with leukocytosis have a statistically significant 40% higher risk of undergoing conversion (OR = 0.40, p <0.05).
DISCUSSION
The study mentioned above that was carried out at San Ignacio University Hospital in Bogotá found that leukocytosis and advanced age were factors that related to conversion of LC to open cholecystectomy. Similarly, this present study demonstrated that these two factors were determinants of surgical conversion and, therefore, of length of hospital stays. (6)
Epidemiologically, it was found that benign vesicular pathologies are more frequent among women because of hormonal factors probably related to the influence of estrogens. (15) This is one of the reasons more cholecystectomies are performed on women than on men. From the results, it is evident that the need for surgical conversion is greater in males. This is justified by the fact epiploic adhesions and inability to see cysts occurred more frequently in men than in women. (16) In addition, subcutaneous adipose tissue is more abundant in men and further complicates the surgeon's task. In some cases, it forces the surgeon to change the intervention into an open cholecystectomy (17).
According to the literature, preoperative ultrasound parameters of vesicular wall thickness and number and size of gallstones are the best indicators of operative difficulty for laparoscopic cholecystectomies. (13) An ultrasound diagnosis of cholelithiasis is quite effective, (18) and diagnosis of acute cholecystitis has established ultrasound criteria including thickness of the vesicular wall equal to or greater than 4 mm, presence of vesicular wall edema, intra-vesicular lithiasis projected in the neck, sizes greater than 100 x 60 mm, fluid in the vesicular area, dilated bile ducts and bile stasis. All of this shows that it is highly dependent on the operator. (13, 18, 19) However, it should be noted that the investigation did not find a relation of the echographic image with conversions of LC due to lack of data in the imaging reports.
Other studies have determined that PCR can be a predictor of conversion, (17, 20, 21) but this study could not determine any associations of laboratory results from PCR and other tests because they were not available in the clinical histories, since the doctors did not request them in the majority of these cases because they are not included in the institution's protocols for these cases.
It is established, then, that these factors are decisive for deciding what type of surgical intervention a patient requires. Prior analysis of these factors can prevent a patient from having more than one surgical intervention which will reduce possible complications surgical conversion such as infections of surgical incisions, postoperative hernias and adhesions. (10, 22) Reduction of complications will reduce hospital stays and hospitalization costs. (9)
The main limitation of this study, the small population sample, could be overcome by enlarging the sample size.
CONCLUSIONS
Conversion to open surgery should never be interpreted as a failure, but as a decision to benefit the patient, despite the risks involved. To avoid these risks, and through the results of our study, we can conclude that conversions occur most frequently among male patients and older patients and that all laboratory tests that demonstrate acute inflammatory process are also determinants, especially high leukocyte values.
Acknowledgements
We would like to thank Dr. Moreno, pathologist and head of Academic Quality of the Regional Hospital of Sogamoso, for his collaboration in suggesting corrections. We also thank all of the file clerks who helped us search the medical records.
REFERENCES
1. Beyrouti MI, Beyrouti R, Affes N, et al. The lithiasic acute cholecystitis: laparoscopic treatment (About 106 cases). Tunis Med. 2011;89(4):355-9. [ Links ]
2. Almora CL, Arteaga Y, Plaza T, et al. Diagnóstico clínico y epidemiológico de la litiasis vesicular. Revisión bibliográfica. Rev Ciencias Médicas. 2012;16(1):200-14. [ Links ]
3. Ibáñez A, Escalona P, Devaud J, et al. Colecistectomía laparoscópica: experiencia de 10 años en la Pontificia Universidad Católica de Chile. Rev Chil Cir. 2007;59(1):10-5. [ Links ]
4. Ocádiz J, Blanco J, García A, et al. Conversión de la colecistectomía laparoscópica, más allá de la curva de aprendizaje. Acta Med Grupo Ángeles. 2011;9(4):192-5. [ Links ]
5. Zuluaga L, Clavijo W, Tavera A. Colecistectomía laparoscópica ambulatoria en una unidad quirúrgica no hospitalaria. Rev Colomb Cir. 2000;15:2-7. [ Links ]
6. Márquez F, Peláez D, Pezzano E, et al. Comportamiento de factores de riesgo de conversión de la Colelap a colecistectomía abierta. Hospital General de Barranquilla, enero de 2014-abril de 2015. Biociencias. 2015;10(2):81-8. [ Links ]
7. Vergnaud J, Penagos S, Lopera C, et al. Colecistectomía laparoscópica: experiencia en hospital de segundo nivel. Rev Colomb Cir. 2000;15:8-13. [ Links ]
8. Granados J, Nieva R, Olvera G, et al. Criterios de conversión de cirugía laparoscópica a cirugía abierta y complicaciones poscolecistectomía: Una estadificación preoperatoria. Asoc Mex Cir Endosc. 2001;2(3):134-41. [ Links ]
9. Díaz S, Correa M, Giraldo L, et al. Experiencia en colecistectomía por laparoscopia en la Clínica Universitaria CES. Rev Colomb Cir. 2012;27:275-80. [ Links ]
10. Haleem S, Ansari M, Mussarat J, et al. Comparative assessment of TNF-alpha and C-reactive protein in patients subjected to open instead of laparoscopic cholecystectomy. Indian J Surg. 2007;69(3):99-104. [ Links ]
11. Jessica Mok K, Goh Y, Howell L, et al. Is C-reactive protein the single most useful predictor of difficult laparoscopic cholecystectomy or its conversion? A pilot study. J Minim Access Surg. 2016;12(1):26-32. [ Links ]
12. Bejarano M. Exactitud diagnóstica de la ecografía en patología vesicular. Rev Cir Col. 2014;17(4):207-12. [ Links ]
13. Pinto Paz M. Relación entre la ecografía preoperatoria y la dificultad de la colecistectomía laparoscópica Hospital Militar Central. Rev Gastroenterol. 2002;22(2). [ Links ]
14. Torres CJR, Torres LE, Weber SA, et al. Entrenamiento y curva de aprendizaje en colecistectomía laparoscópica y abierta. Resultados de la Encuesta Nacional de Lesiones de la Vía Biliar. Cir Gen. 2007;29(2):100-8. [ Links ]
15. Naranjo Rodríguez A, Rodríguez Ramos C. Litiasis biliar, colangitis aguda y colecistitis aguda. En: Ponce J, Castells A, Gomollon F (editores). Tratamiento de las enfermedades gastroenterológicas. 3.ª edición. Madrid: Elsevier España S.A.; 2011. p. 415-26. [ Links ]
16. Sakpal S, Bindra S, Chamberlain R. Laparoscopic cholecystectomy conversion rates two decades later. JSLS. 2010;14(4):476-83. [ Links ]
17. Pedrosa Mendoza LE, Vázquez Ríos BS. Imagenología. La Habana: Editorial Ciencias Médicas; 2005. [ Links ]
18. Pérez MJ, Cabrera W, Varela G, et al. Distribución regional de la grasa corporal. Uso de técnicas de imagen como herramienta de diagnóstico nutricional. Nutr Hosp. 2010;25(2):207-23. [ Links ]
19. Kanakala V, Borowski D, Pellen M, et al. Risk factors in laparoscopic cholecystectomy: a multivariate analysis. Int J Surg. 2011;9(4):318-23. [ Links ]
20. Lin C, Collins J, Britt R, et al. Initial cholecystectomy with cholangiography decreases length of stay compared to preoperative MRCP or ERCP in the management of choledocholithiasis. Am Surg. 2015;81(7):726-31. [ Links ]
21. Domínguez L, Rivera A, Bermúdez C, et al. Análisis de los factores de conversión durante colecistectomía laparoscópica a abierta en una cohorte prospectiva de 703 pacientes con colecistitis aguda. Cir Esp. 2011;89(5):300-6. [ Links ]
22. Straatman J, Harmsen A, Cuesta M, et al. Predictive value of C-reactive protein for major complications after major abdominal surgery: A systematic review and pooled-analysis.PLoS One 2015;10(7):e0132995. [ Links ]











 text in
text in