Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.32 no.2 Bogotá abr./jun. 2017
https://doi.org/10.22516/25007440.145
Reporte de casos
Hemobilia Secondary to Aneurysm of the Hepatic Artery
1Residente de gastroenterología y endoscopia digestiva, Universidad del Rosario. Unidad de gastroenterología, Hospital de la Samaritana. Bogotá, Colombia
2Gastroenterólogo, facultad de medicina de la Universidad Nacional de Colombia. Unidad de gastroenterología del Hospital de La Samaritana. Bogotá, Colombia
3Gastroenterólogo. Unidad de gastroenterología, Hospital de la Samaritana. Bogotá, Colombia
We present the case of a patient with upper digestive tract hemorrhaging and jaundice due to an aneurysm of the right hepatic artery.
Keywords: Hemobilia; hemorrhages of high digestive tract; hepatic artery aneurysm
Se presenta el caso de un paciente con hemorragia de vías digestivas altas e ictericia asociadas a un aneurisma de la arteria hepática derecha.
Palabras clave: Hemobilia; hemorragias de vías digestivas altas; aneurisma de arteria hepática
Introduction
Hemobilia, defined as the presence of blood in the bile duct, is a rare cause of digestive hemorrhaging which is not often considered and is therefore seldom diagnosed.
The first case was described by Francis Glisson in 1654, but Quinke described the classic case of hemobilia’s clinical features in 1871. The classic triad is jaundice, pain in the right hypochondrium and upper digestive hemorrhaging. 1,2,3 In 1903, Kehr first performed surgery on a patient with hemobilia secondary to rupture of an aneurysm of the hepatic artery (AHA). 4
The causes of hemobilia vary and can be traumatic, iatrogenic (resulting from surgical or endoscopic manipulation of the bile duct), inflammatory, infectious, neoplastic and vascular (aneurysms, vasculitis and arteriovenous malformations).
AHA accounts for about 0.4% of all aneurysms and for almost one-fifth of all visceral arterial aneurysms. 3,4,5 Increasing incidence in recent years is probably due to the availability of better diagnostic images. 6 Etiologies of AHA include atherosclerosis; autoimmune diseases with vascular involvement such as polyarteritis nodosa, systemic lupus erythematosus and Takayasu’s arteritis; Marfan syndrome; tuberculosis and surgical or endoscopic manipulation of the bile duct. Most frequently they occur in the hepatic hilum and less frequently within the liver. Most patients remain asymptomatic, but abdominal pain, digestive bleeding and hypovolemic shock can result from hemobilia. When an aneurysm ruptures, mortality occurs about 40% of time. 5,6,7,8,9
We present the case of a patient with upper digestive tract hemorrhaging and jaundice due to the presence of an aneurysm in the right hepatic artery.
Clinical case
The patient was a 38-year-old man, with a history of severe cognitive impairment due to chronic convulsive syndrome and paranoid schizophrenia. He had no other pathological, surgical, or traumatic antecedents. He was admitted to another institution after 15 days of hematemesis, melena, mucocutaneous jaundice and pain in the right hypochondrium. An esophagogastroduodenoscopy performed upon admission showed fresh blood in the duodenum but did not identify its origin. A subsequent ileal colonoscopy also failed to identify the source of bleeding, so an endoscopic videocapsule was used, but it also failed to find any hemorrhaging. Internal bleeding continued as his hemoglobin fell to 6.8 g/dL. The patient received a transfusion of two units of packed red blood cells and was transferred sent to our institution. Upon admission, he had generalized jaundice but was hemodynamically stable. He suffered pain on palpation of the right hypochondrium, and a rectal examination showed melena.
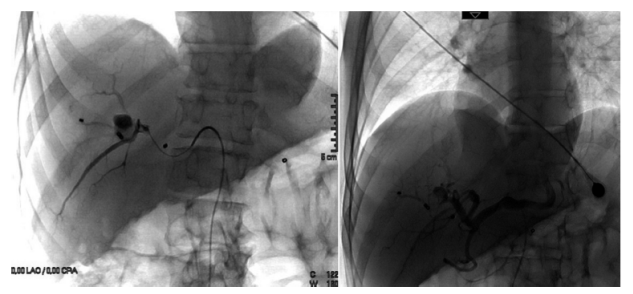
Principal laboratory results included hemoglobin of 8.9 g/dL, mean corpuscular volume of 72 fL, total bilirubin of 6 mg/dL, direct bilirubin of 4.3 mg/dL, and alkaline phosphatase of 1067 IU/L. Upper digestive tract endoscopy showed active bleeding from around the ampulla of Vater giving rise to a suspicion of hemobilia. Abdominal ultrasound showed a vascular lesion in the hepatic hilus suggestive of a dilated aneurysm. Abdominal computed tomography (CT) angiography demonstrated a dilated aneurysm measuring 37 x 39 x 34 mm with a 50% thrombus inside in close relation with the gallbladder and apparently dependent on the right hepatic artery. Selective arteriography showed an aneurysm of the right hepatic artery as described above and with a thrombus in its interior. Embolization was performed and three micro-coils were used to completely close the neck of the aneurysm. Five days later, another abdominal CT scan showed that the size of the lesion had decreased to 19 x 18 x 15 mm but that the aneurysm was filled with turbulent contrast medium. Another arteriography and embolization with micro-coils achieved complete exclusion of the aneurysm with distal and proximal occlusion (Figure 1).
The patients subsequent development was favorable: abdominal pain disappeared, the jaundice resolved, and there have been no recurrences of gastrointestinal bleeding since the procedure.
Discussion
Hemobilia is a rare cause of upper gastrointestinal bleeding that is diagnosed even less frequently than it occurs because diagnosis usually requires a high level of clinical suspicion and experienced medical personnel. Its exact incidence is unknown, but a very high mortality rate of up to 25% has been reported. 10 This case highlights the importance of suspecting this pathology in patients who develop melena. 11
This patient presented the classic clinical signs of hemobilia: pain in the right hypochondrium, jaundice and evidence of upper gastrointestinal bleeding. About 40% of those affected present this triad, but the remaining cases do not.
As described in the medical literature, initial diagnosis of hemobilia is elusive in most patients, so it becomes necessary to use several endoscopic procedures by different observers. Even then it is often impossible to reach the diagnosis. For this reason, it is advisable that patients with melena have clinical and endoscopic reevaluations be performed by physicians with extensive experience in the care of gastroenterological emergencies.
Esophagogastroduodenoscopy is the diagnostic method of choice because, in addition to ruling out other causes of hemorrhaging, it can observe the flow of blood from the duodenal papilla. 12 Complementary diagnostic studies include abdominal ultrasonography, abdominal CT scana, abdominal magnetic resonance (MRI) and selective arteriography.
AHAs are extremely rare causes of obstructive jaundice and hemobilia. They are infrequently diagnosed, but their incidence has been increasing thanks to the development of better imaging techniques. In most cases, the AHA are asymptomatic so that when they present their symptoms are associated with poor prognosis if diagnosis is delayed.
Upper digestive tract hemorrhaging or hemobilia secondary to AHA justifies urgent management since the rupture can be fatal. There are multiple complementary studies for diagnosis including CT angiography which allows detection with good reliability and hepatic angiography which continues to be the gold standard among diagnostic and therapeutic options together with selective transarterial embolization. This is the first choice for managing AHA. It has success rates of 80% to 100% and lower mortality rates than in surgical procedures. 4,5 Other therapeutic options include surgical repair and stenting which should be reserved for cases in which transarterial embolization is not possible. 5
Conclusion
Hemobilia should always be suspected in patients with evidence of blood in the duodenum and especially in those who present the classic triad. AHA is one of the conditions that can cause hemobilia and, if not considered, may not be diagnosed. Hepatic angiography remains the gold standard for diagnosis and treatment in these cases.
REFERENCIAS
1. Sandblom P. Hemobilia (biliary tract hemorrhage): history, pathology, diagnosis, treatment. Springfield: Charles C. Thomas; 1972. [ Links ]
2. Merrell S, Schneider P. Conferences and review. Hemobilia, evolution of current diagnosis and treatment. West J Med. 1991;155(6):621-5. [ Links ]
3. Petrou A, Brennan N, Soonawalla Z, et al. Hemobilia due to cystic artery stump pseudoaneurysm following laparoscopic cholecystectomy: case presentation and literature review. Int Surg. 2012;97(2):140-4. Doi: https://doi.org/10.9738/CC52.1 [ Links ]
4. Beltrán F, Castillo A, Hidalgo H. Hemobilia secundaria a pseudoaneurisma roto: reporte de caso. Rev Gastroenterol Peru. 2015;35(1):89-92. [ Links ]
5. Panno C, Gutiérrez S, Echeverría R, et al. Hemobilia secundaria a pseudoaneurisma de la arteria hepática. Acta Gastroenterol Latinoam. 2015;45(2):133-6. [ Links ]
6. Peter G, Shaheer R, Narayanan P, et al. Hepatic artery aneurysm: a rare case of obstructive jaundice with severe hemobilia. Ann Gastroenterol. 2014;27(3):288-9. [ Links ]
7. Suarez Grau JM, Rubio Chaves C, Pareja Ciuro F, et al. Obstructive jaundice secondary to hepatic artery aneurysm. Cir Cir. 2008;76(3):253-6. [ Links ]
8. García C, Pérez Ramírez P, Martorell-Lossius A, et al. Aneurismas de las arterias viscerales. Cir Esp. 2005;78(4):246-50. Doi: https://doi.org/10.1016/S0009-739X(05)70926-X [ Links ]
9. Alhawsawi A, Aljiffry M, Walsh M, et al. Hepatic artery aneurysm associated whith prune belly syndrome: a case report and review of the literature. J Surg Educ. 2009;66(1):43-7. Doi: https://doi.org/10.1016/j.jsurg.2008.10.004 [ Links ]
10. Baillie J. Hemobilia. Gastroenterol Hepatol (N Y). 2012;8(4):270-2. [ Links ]
11. Gerson LB, Fidler JL, Cave DR, et al. Clinical guideline: diagnosis and management of small bowel bleeding. Am J Gastroenterol 2015;110(9):1265-87. Doi: https://doi.org/10.1038/ajg.2015.246 [ Links ]
12. Rencuzogullari A, Okoh AK, Akcam TA, et al. Hemobilia as a result of right hepatic artery pseudoaneurysm rupture: An unusual complication of laparoscopic cholecystectomy. Int J Surg Case Rep. 2014;5(3):142-4. Doi: https://doi.org/10.1016/j.ijscr.2014.01.005 [ Links ]
Received: August 02, 2016; Accepted: April 21, 2017











 texto em
texto em