Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.32 no.3 Bogotá jul./set. 2017
https://doi.org/10.22516/25007440.157
Review articles
Esophagograms: Images Worth a Thousand Words
1 Departamento de Cirugía Gastrointestinal y Endoscopia Digestiva, Instituto Nacional de Cancerología, Bogotá D. C. (Colombia). Correo electrónico: bborraez@hotmail.com
2 Departamento de Radiología e Imágenes Diagnósticas, Colsanitas, Bogotá (Colombia).
3 Departamento de Cirugía Oncológica, Instituto Nacional de Cancerología, Bogotá D. C. (Colombia).
4 Profesor asistente de cirugía, Facultad de Medicina, Universidad Nacional de Colombia, Bogotá. Colombia.
5 Departamento de Gastroenterología y Endoscopia, Fundación Universitaria Sanitas, Clínica Colombia, Bogotá D. C. (Colombia).
6 Departamento de Cirugía, Facultad de Medicina Pritzker de la Universidad de Chicago, Chicago (Illinois). U.S.A.
7 Departamento de Cirugía Esófago-Gástrica, Fundación Favaloro, Buenos Aires (Argentina).
The study of esophageal diseases requires multiple diagnostic tests since no one test alone can provide full information on upper digestive tract anatomy and functionality. For general surgeons and gastrointestinal surgeons, the esophagogram is an essential tool that can suggest a diagnosis while simultaneously providing an idea of the anatomy of the organ and outlining an easily evaluated map without the need of a radiologist. This information can be used to establish a surgical plan. The aim of this article is to show readers the usefulness of esophagograms at referral centers for study and treatment of esophageal diseases while providing representations of several frequent diseases.
Keywords: Esophagus; diseases of the esophagus; esophageal neoplasms; esophagogram
El estudio de las enfermedades esofágicas requiere de múltiples exámenes diagnósticos, ya que ninguno, por sí solo, provee total información sobre la funcionalidad y la anatomía del tracto digestivo superior. Para los cirujanos generales y gastrointestinales, el esofagograma constituye una herramienta esencial que, además de sugerir un diagnóstico, ofrece una idea de la anatomía del órgano y nos permite esbozar un mapa de fácil evaluación (sin la necesidad de un radiólogo), para establecer o definir un plan quirúrgico. El objetivo del presente artículo es mostrar al lector la utilidad del esofagograma en centros de referencia en el estudio y el tratamiento de las enfermedades esofágicas, así como su representación en algunas enfermedades frecuentes.
Palabras claves: Esófago; enfermedades del esófago; neoplasias esofágicas; esofagograma
Introduction
The study of diseases of the esophagus requires multiple diagnostic aids that provide, information about esophageal functionality and/or anatomy depending on the disease. An esophagogram is a dynamic radiological study of the upper digestive tract that uses contrast medium and air for double contrast and allows diagnosis of structural and functional esophageal abnormalities. Although esophagrams have been falling out of use, this study shows that for general and gastrointestinal surgeons the study remains an essential tool for diagnosis and for planning of surgical treatment.
The objective of this article is to show the usefulness of esophagograms and their radiological representation for study and treatment of esophageal diseases in referral centers. Simultaneously, this article presents images and descriptions of the most frequently found conditions and diseases.
Esophagograms
Esophageal diseases can be caused by functional and structural alterations, and their study can be complex since no examination offers complete information and evaluation of the organ. The esophagogram, also known as the barium swallow, is a simple and dynamic study that allows partial evaluation of the anatomy and functioning of the esophagus. 1,2 The technique consists of taking multiple sequential images after a patient swallows contrast medium (generally, 100 to 250 mL). The images are taken every 1, 2 and 5 minutes after the contrast is taken. 1,2 Interpretation requires clinical correlation with findings of physical examination and other studies such as endoscopy, pH measurements, conventional manometry and high resolution manometry. 1,2
The column of contrast medium, esophageal emptying and the integrity of anatomical structures, especially the esophageal walls and the gastroesophageal junction, should be evaluated (Figure 1). 1,2,3,4

Figure 1 Normal esophagogram. Important structures in the images are the aortic impression, right diaphragm, left diaphragm, gastroesophageal junction and stomach. Esophageal wall of smooth mucosa without irregularities.
Three different anatomical portions are evaluated according to their location 1,2,3,4:
The cervical esophagus extends from the pharynx to the sixth cervical vertebra and the lower border of cricoid cartilage.
The thoracic esophagus extends from the sixth cervical vertebra to the esophageal hiatus.
The abdominal esophagus extends from the esophageal hiatus to the gastroesophageal junction (Figure 1).
A video fluoroscopic swallowing exam (VFSE) evaluates the ability to swallow different substances. It focuses on the oropharynx and upper esophagus and can be modified by using different contrast medium textures and viscosities. Modification allows a more exhaustive evaluation of swallowing and swallowing disorders which is important for planning compatible diets and eliminating the risk of aspiration. 2
For patients with dysphagia for solids or for whom stenosis is suspected, solid foods impregnated with barium can help determine the size of the esophagus and/or the stenosis. 2
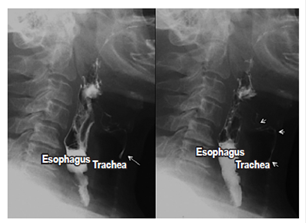
Aspiration
Aspiration is the passage of food (contrast medium) from the digestive tract to the respiratory tract. Aspiration can occur in asymptomatic patients and may be due to neuromuscular diseases or to upper digestive tract disorders. Predisposing factors include alterations in the state of consciousness, swallowing disorders and neurological deficiencies. 2,5 Aspiration is an important morbidity and mortality event in patients of advanced ages and may be asymptomatic in up to 55% of patients. The esophagogram, even with the arrival of new technologies, continues to be the study of choice for its diagnosis (Figure 2). 2,5
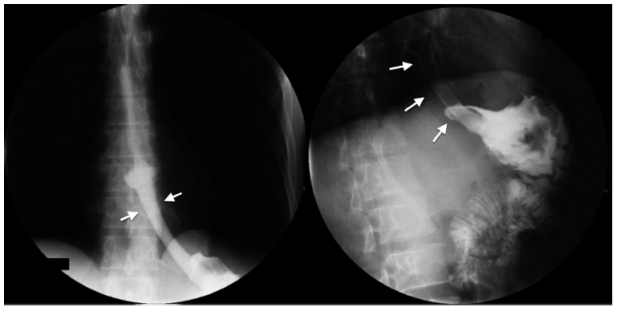
Gastroesophageal Reflux
Gastroesophageal reflux is a condition that affects normal individuals but becomes pathological when symptoms or complications develop 6,7. Its multifactorial physiopathology produces an imbalance between aggressor and protective factors (barrier failure and protection mechanisms). Although the diagnosis is made with 24-hour pH measurement, an esophagogram can suggest the presence of reflux with changes in position (supine) and Valsalva maneuvers plus it allows identification of any associated hiatal hernias (Figure 3). 6,7
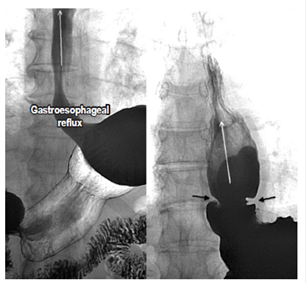
Figure 3 Gastroesophageal reflux. In the images, reflux of the contrast medium from the stomach to the esophagus is observed in the supine decubitus position and the Valsalva maneuver is performed (white arrows). In the image on the right, reflux (white arrows) associated with an esophageal ring (black arrows) is observed.
The sensitivity and specificity of the esophagogram for diagnosis varies according to the phase in which it was evaluated and the complications that arise. In the initial standing phase, its sensitivity is low, but it increases with changes in position and Valsalva maneuvers. In patients with moderate to severe esophagitis, sensitivity varies from 71% to 85% with a low detection rate of peptic stenosis (43%) and a positive predictive value of only 25% for Barrett’s esophagus, although its negative predictive value is 99%. (8,9,10
Hiatal Hernia
Hiatal hernias are protrusions of the stomach through the esophageal hiatus into the thorax. They affect 10% to 50% of the population, but early diagnosis and treatment can prevent development of more complex diseases. 11,12 In the final evaluation of the esophagogram, hiatal hernias should be identified and defined by sizes greater than 2 cm and location between the gastroesophageal junction and the diaphragmatic hiatus (If it is less than 2 cm, the herniation is physiological.) 11,12 Ninety-five percent of primary hernias are type I (slipped). Types II, III and IV are paraesophageal hernias. More than 90% of this group are type III while the least common are type II. Laparoscopic repair is the standard treatment. An esophagogram is useful for establishing the size of the hernia since it requires wide esophageal dissection, adequate closure of the hiatus, possibly using mesh, and an anti-reflux mechanism (Figure 4). 11,12

Figure 4 Hiatal hernia. A. A Type I sliding hiatal hernia is found. The “glide” of the gastroesophageal junction above the diaphragmatic level is demarcated by a black line. B. Type II paraesophageal hernia with displacement of the fundus and part of the gastric corpus (black arrow) but with the gastroesophageal junction in its normal position. C. Type III mixed hiatal hernia with displacement of the gastroesophageal junction and gastric fundus to the thorax (white arrow). Type IV hiatal hernia contains organs other than the stomach which is difficult to assess in this study.
Gastric volvulus
Gastric volvulus is an abnormal rotation of more than 180º of the stomach on itself. Acute gastric volvulus is a surgical emergency which requires decompression and gastric return. Radiological study with contrast medium is impossible due to the high risk of aspiration. 12 When gastric volvulus is chronic, the usual symptoms are regurgitation, heartburn, chest pain and dysphagia. An esophagogram, as part of the study of these symptoms, allows evaluation of the anatomy to determine the presence of a hernia, its size and its axis of rotation. 11,12
Gastric volvuli are classified into three types as can be seen in (Figure 5). 9
Mesenteroaxial (rotation on the axis of the mesentery).
Organoaxial (rotation on its own axis).
Mixed
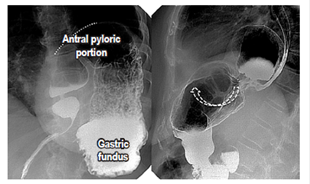
Figure 5 Gastric volvulus. The first image on the right shows a mesenteroaxial gastric volvulus in which the antrum moves towards the top (dotted line) and the fundus is in the bottom position. The second image on the left shows an organoaxial gastric volvulus with rotation and displacement of the gastric parts (white dotted arrow).
Esophageal Motility Disorders
Esophageal motor disorders include a wide variety of rare conditions of unknown etiology. The esophagogram has great sensitivity for diagnosis of some functional motility disorders but definitive diagnosis depends on findings of classical manometry or high resolution manometry. 13,14 Achalasia is a chronic and progressive disease characterized by failure of relaxation of the lower esophageal sphincter, absence of peristalsis and increased intraluminal esophageal pressure (Figure 6). 14,15
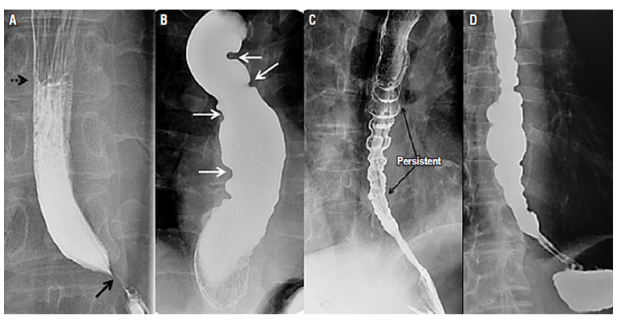
Figure 6 Esophageal motility disorders. A. The classic image of achalasia shows an air-fluid level in the middle esophageal third (punctuated arrow), distal esophageal narrowing that forms the sign of “bird’s beak” (black arrow), esophageal dilation and absence of peristalsis indicated by straight or smooth esophageal borders. B. Terminal stage of achalasia in the sigmoid esophagus is shown. Multiple curves do not allow adequate passage of the barium through the esophagus. C. Esophagogram characteristic of diffuse esophageal spasming is shown multiple areas of uncoordinated esophageal contraction. D. Nutcracker esophagus is shown.
Despite this, approximately 20% to 30% of patients with this diagnosis and with typical radiological findings have no dysfunction of the lower esophageal sphincter 10,14. The diffuse esophageal spasm occurs with uncoordinated contractions and retrosternal pain. Nutcracker esophagus has a normal propagation wave, but with greater contraction force and increased duration of contraction (Figure 6). 14,15,16 In patients with diffuse esophageal spasms, peristaltic contractions occur in less than 15% of cases due to their intermittent presentation. 10,14
Esophageal Diverticula
Diverticula are infrequent alterations of the integrity of the esophageal wall whose clinical presentation is marked by dysphagia and regurgitation. Diverticula are classified according to their anatomical locations in the upper, middle or lower esophagus. Barium studies are the most effective method for evaluation of this disease since they provide definitive diagnosis in more than 95% of cases. 18,19,20) Zenker’s diverticulum, the most common diverticulum of the upper esophagus, is associated with disorders of motility and swallowing, but there is no consensus on the exact mechanism of formation (Figure 7). 18,19

Figure 7 Esophageal diverticula. A. Zenker’s diverticulum with a diverticular sac shown by the dotted line located in the posterior part of the upper third of the esophagus which becomes opaque as a result of the contrast medium. B. Diverticulum of the middle esophagus with a wide-based diverticular sac located in the middle third of the esophagus, and an air-fluid level (white arrow) due to partial opaqueness due to the contrast medium. C. An epiphrenic diverticulum with a diverticular sac located in the distal esophagus. Hydro-aerial levels are found by partial filling with the contrast medium.
Diverticula of the middle esophagus are classified according to their etiology. Traction diverticula are associated with inflammatory processes or scarring from tuberculosis while pulsion diverticula are associated with motor disorders. Epiphrenic diverticula are proximal to the diaphragm, are associated with esophageal motility disorders, and some require resection (Figure 7). 19,20
Cardiovascular Dysphagia
Cardiovascular dysphagia includes multiple cardiovascular diseases that cause esophageal compression and secondary dysphagia. These can be divided into congenital, acquired and iatrogenic conditions. Congenital conditions include double aortic arches, right aortic arches, cervical aortic arches, Kommerell diverticula, aberrant subclavian arteries, pulmonary artery slings, and ligament arteriosus. Acquired conditions include aortic dissection, scoliosis and left atrial growth, and iatrogenic conditions include aortic-esophageal fistulas and postoperative dysphagia. 21,22
Growth of the left atrium secondary to congenital or acquired diseases and associated with mitral stenosis can cause esophageal compression with secondary dysphagia. This type of dysphagia requires differential diagnosis. When the growth of the atrium is secondary to rheumatic mitral valve disease and paralysis of the left recurrent laryngeal nerve, it is known as Ortner’s syndrome or cardiovocal dysphagia (Figure 8). 21,22,23

Figure 8 Cardiovascular dysphagia. Lateral oblique (left) and anteroposterior (right) projections of esophagogram in which left atrial growth is identified by the curved line that imprints and displaces the esophagus to the left with the air-fluid level shown by the dotted arrow caused by slow transit.
Benign Esophageal Tumors
Esophagograms are very useful for detection, location and measurement of benign and malignant stenosing lesions and have a sensitivity of 95% for detection of narrowing of the esophageal lumen. 13 Duplication cysts are infrequent congenital alterations of digestive tract development that are considered the third most frequent benign tumor of the esophagus after polyps and leiomyoma. In adults, they are found incidentally. Their most frequent location is in the right posteroinferior mediastinum. They are usually treated usually surgical, even in the absence of symptoms (Figure 9). 24,25
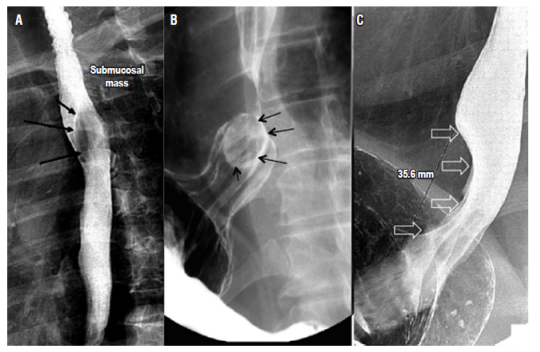
Figure 9 Benign tumors of the esophagus. A. An esophageal duplication cyst and a lesion causing extrinsic compression of the posterior wall of the middle third of the esophagus is shown by the black arrows. B. Esophageal fibrovascular polyp indicated by a rounded intraluminal lesion in the distal third of the esophagus. C. A leiomyoma indicated by compression and thinning of the esophageal lumen due to a fusiform lesion in the distal third of the esophagus.
Fibrovascular polyps are subepithelial and intraluminal tumors which grow slowly and are generally located in the proximal esophagus. They appear with long pedicles which grow distally, and the polyp may be distal to its implantation site. Endoscopic or surgical resection represents a therapeutic option in patients who have symptoms (Figure 9). 26,27
Leiomyomas are the most common benign tumors of the esophagus. They are usually located in the wall of the lower third of the esophagus. These tumors present with dysphagia and chest pain and are generally non-obstructive motile masses that rarely cause esophageal dilation. Surgery is reserved for symptomatic patients (Figure 9). 27
Malignant Esophageal Tumors
Esophageal cancer is an increasingly common pathology which has discouraging survival rates. Tumor location indicates histological type with squamous cell carcinoma generally found in the middle and upper esophagus, and adenocarcinomas mostly found in the lower esophagus. An esophagogram can locate the tumor and help generate a surgical plan, but it can also provide an idea of tumor stage. Those longer than 5 cm and stenosing tumors generally correspond to stages T3 and T4 (Figure 10). 28,29 The sensitivity of the study is greater than 95% for diagnosis of esophageal cancer which is similar to the sensitivity of digestive endoscopy of 95% to 100%. 10
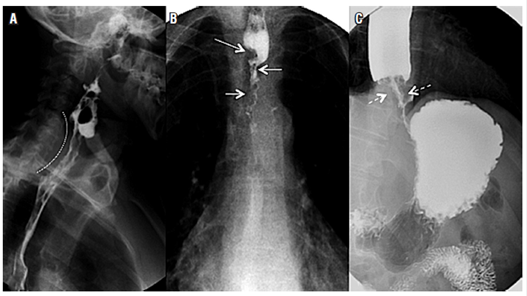
Figure 10 Malignant tumors of the esophagus. A. A posterior view of a malignant tumor in the cervical esophagus is indicated by the dotted line. Slow transit of the barium and irregularity in the mucosal surface can be seen. B. A malignant tumor in the thoracic esophagus with filiform passage of the contrast medium (white arrows) due to the thinning of the tumor which has a concentric growth pattern. C. A malignant tumor of the distal esophagus with evidence of concentric growth of the tumor (white punctuated arrows), filiform passage and slow transit of the barium, with proximal esophageal distention.
Evaluation of Surgical Procedures
Surgical procedures such as esophagectomies are performed for many reasons but have considerable morbidity and mortality. Early detection of complications allows quick action by the surgeon to prevent further complications. 30,31 An esophagogram is a very useful study for evaluating success of a surgical procedure as well as problems that can result from surgery. Stenosis of the anastomoses and anastomotic leaks are clear examples. Proper treatment derives from appropriate performance and interpretation. Although some studies report low sensitivity (36%), specificity in for anastomotic leaks approaches 100% (Figure 11). 30,31

Figure 11 Evaluation of surgical procedures. Latero-lateral intrathoracic esophagogastric anastomosis (left). Adequate passage of the contrast medium is shown by the curved arrow. Postoperative stenosis (right) with an area of narrowing at the site of the anastomosis (white arrows) and thinning of the esophageal lumen are also observed in a patient with a history of esophagectomy.
This study can also provide additional information on aspiration and on adequate emptying of any duct used for reconstruction of the stomach or colon (Figures 1 and 11). 30,31
The wrap can be observed in patients who have undergone antireflux surgery. Totally or partially surrounding the gastroesophageal junction, with a length of 2 to 3 cm, it should allow adequate passage of the contrast medium. Recurrent hiatal hernia can also be evaluated and correlated with the presence of symptoms. We are careful to evaluate the location of the wrap with respect to the gastroesophageal junction and the diaphragm in these patients and to evaluate the possibility of reflux of the contrast medium using the maneuvers described (Figure 12). 8,9
Identification of Stent and Evaluation of their Functionality
Endoscopic stents are used to maintain permeability in cases of malignant or benign obstruction and to control anastomotic leaks. They are less invasive procedures and have a low rate of complications, short hospital stays and low costs. 32 The esophagogram is a useful tool to assess the best location for the stent and its functionality (Figure 13 and 14). 32

Figure 13 Stent in the middle esophagus due to stenosing cancer. In the two images (left and right), the white arrows mark the extension of the stent and the passage of the contrast medium.
Conclusions
In conclusion, despite falling into disuse as the result of continuous emergence of new technologies, we conclude that esophagograms are simple, easy to understand, and provide information about anatomy as well as indirect information about esophageal functioning which is useful for developing a therapeutic plan.
Acknowledgements
We extend our thanks to the Department of Gastrointestinal Surgery and Digestive Endoscopy at the National Institute of Cancer and the Universidad Militar Nueva Granada.
REFERENCES
1. Neyaz Z, Gupta M, Ghoshal UC. How to perform and interpret timed barium esophagogram. J Neurogastroenterol Motil. 2013;19(2):251-6. Doi: https://doi.org/10.5056/jnm.2013.19.2.251 [ Links ]
2. Furlow B. Barium swallow. Radiol Technol. 2004;76(1):49-58. [ Links ]
3. Borraez BA, Gasparaitis A, Patti MG. Esophageal diseases: radiologic images. En: Esophageal diseases. Springer International Publishing Switzerland; 2014. pp. 11-39. [ Links ]
4. Borraez BA, Patti MG. Radiologic evaluation of esophageal diseases. En: Atlas of esophageal surgery. Springer International Publishing Switzerland; 2015. pp. 9-21. [ Links ]
5. Fuentes Santos C, Steen B. Aspiration of barium contrast. Case Rep Pulmonol. 2014;2014:1-3. Doi: https://doi.org/10.1155/2014/215832 [ Links ]
6. Baker ME, Einstein DM. Barium esophagram: does it have a role in gastroesophageal reflux disease? Gastroenterol Clin N Am. 2014;43:47-68. Doi: https://doi.org/10.1016/j.gtc.2013.11.008 [ Links ]
7. Allaix ME, Fisichella PM, Noth I, et al. Idiopathic pulmonary fibrosis and gastroesophageal reflux. implications for treatment. J Gastrointest Surg. 2014;18(1):100-4. Doi: https://doi.org/10.1007/s11605-013-2333-z [ Links ]
8. Baker ME, Einstein DM. Barium esophagram does it have a role in gastroesophageal reflux disease? Gastroenterol Clin N Am. 2014;43:47-68. Doi: https://doi.org/10.1016/j.gtc.2013.11.008 [ Links ]
9. Katzka DA. The role of barium esophagography in an endoscopy world. Gastrointest Endoscopy Clin N Am. 2014;24:563-80. Doi: https://doi.org/10.1016/j.giec.2014.06.004 [ Links ]
10. Levine MS, Rubesin SE, Laufer I. Barium esophagography: a study for all seasons. Clin Gastroenterol Hepatol. 2008;6(1):11-25. Doi: https://doi.org/10.1016/j.cgh.2007.10.029 [ Links ]
11. Dean C, Etienne D, Carpentier B, et al. Hiatal hernias. Surg Radiol Anat. 2012;34(4):291-9. Doi: https://doi.org/10.1007/s00276-011-0904-9 [ Links ]
12. Arévalo C, Luna RD, Luna-Jaspe C, et al. Hernia hiatal recidivante: la visión del cirujano. Revisión de la literatura. Rev Col Gastroenterol. 2015;30(4):447-55. [ Links ]
13. Scharitzer M, Pokieser P. What is the role of radiological testing of lower esophageal sphincter function? Ann N Y Acad Sci. 2016;6:1-11. [ Links ]
14. Maurer AH. Gastrointestinal motility, part 1: esophageal transit and gastric emptying. J Nucl Med Technol. 2016;44(1):1-11. Doi: https://doi.org/10.2967/jnumed.113.134551 / https://doi.org/10.2967/jnumed.112.114314 [ Links ]
15. Krill JT, Naik RD, Vaezi MF. Clinical management of achalasia: current state of the art. Clin Exp Gastroenterol. 2016;9:71-82. [ Links ]
16. Carucci LR, Turner MA. Dysphagia revisited: common and unusual causes. Radiographics. 2015;35(1):105-22. Doi: https://doi.org/10.1148/rg.351130150 [ Links ]
17. Aziz Q, Fass R, Gyawali CP, et al. Functional esophageal disorders. Gastroenterology. 2016;150:1368-79. Doi: https://doi.org/10.1053/j.gastro.2016.02.012 [ Links ]
18. Tao TY, Menias CO, Herman TE, et al. Easier to swallow: pictorial review of structural findings of the pharynx at barium pharyngography. Radiographics. 2013;33(7):189-208. Doi: https://doi.org/10.1148/rg.337125153 [ Links ]
19. Bagheri R, Maddah G, Mashhadi MR, et al. Esophageal diverticula: analysis of 25 cases. Asian Cardiovasc Thorac Ann. 2014;22(5):583-7. Doi: https://doi.org/10.1177/0218492313515251 [ Links ]
20. Allaix ME, Borraez Segura BA, Herbella FA, et al. Is resection of an esophageal epiphrenic diverticulum always necessary in the setting of achalasia? World J Surg. 2015;39(1):203-7. Doi: https://doi.org/10.1007/s00268-014-2770-1 [ Links ]
21. Yuan SM. Cardiovascular dysphagia: anatomical and clinical implications. Folia Morphol (Warsz). 2014;73(2):113-21. Doi: https://doi.org/10.5603/FM.2014.0026 [ Links ]
22. Al-Quthami A, Albloushi A, Alquthami AH. Images in vascular medicine. Dysphagia aortica with left atrial compression. Vasc Med. 2015;20(3):266-7. Doi: https://doi.org/10.1177/1358863X14568445 [ Links ]
23. Heng JS, Elghamaz A. Atrial enlargement associated with non-valvular atrial fibrillation: an unusual cause of dysphagia and weight loss. BMJ Case Rep. 2015. Doi: https://doi.org/10.1136/bcr-2014-209213 [ Links ]
24. Huang J, Yan ZN. Dysphagia due to esophageal duplication Cyst. Clin Gastroenterol Hepatol. 2016. [ Links ]
25. Al-Riyami S, Al-Sawafi Y. True intramural esophageal duplication cyst. Oman Med J. 2015;30(6):469-72. Doi: https://doi.org/10.5001/omj.2015.91 [ Links ]
26. Blacha MM, Sloots CE, Van Munster IP, et al. Dysphagia caused by a fibrovascular polyp: a case report. Cases J. 2008;19(1):334. Doi: https://doi.org/10.1186/1757-1626-1-334 [ Links ]
27. Ha C, Regan J, Cetindag IB, et al. Benign esophageal tumors. Surg Clin North Am. 2015;95(3):491-14. Doi: https://doi.org/10.1016/j.suc.2015.02.005 [ Links ]
28. Van Dam J, Rice TW, Catalano MF, et al. High-grade malignant stricture is predictive of esophageal tumor stage. Risks of endosonographic evaluation. Cancer. 1993;71(10):2910-7. Doi: https://doi.org/10.1002/1097-0142(19930515)71:10<2910::AID-CNCR2820711005>3.0.CO;2-L [ Links ]
29. Alsop BR, Sharma P. Esophageal cancer. Gastroenterol Clin North Am. 2016;45(3): 993-412. Doi: https://doi.org/10.1016/j.gtc.2016.04.001 [ Links ]
30. Upponi S, Ganeshan A, D’Costa H, et al. Radiological detection of post-esophagectomy anastomotic leak: a comparison between multidetector CT and fluoroscopy. Br J Radiol. 2008;81(967):545-8. Doi: https://doi.org/10.1259/bjr/30515892 [ Links ]
31. Roh S, Iannettoni MD, Keech JC, et al. Role of barium swallow in diagnosing clinically significant anastomotic leak following esophagectomy. Korean J Thorac Cardiovasc Surg. 2016;49(2):99-106. Doi: https://doi.org/10.5090/kjtcs.2016.49.2.99 [ Links ]
32. Kang HW, Kim SG. Upper gastrointestinal stent insertion in malignant and benign disorders. Clin Endosc. 2015;48(3):187-9. Doi: https://doi.org/10.5946/ce.2015.48.3.187 [ Links ]
Received: November 09, 2016; Accepted: July 28, 2017











 texto em
texto em