Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.32 no.4 Bogotá Oct./Dec. 2017
https://doi.org/10.22516/25007440.181
Review articles
How to Perform High Resolution Esophageal Manometry and How to Interpret It Using Chicago 3.0
1Hospital Universitario San Ignacio, servicio de gastroenterología. Pontificia Universidad Javeriana, Bogotá D. C., Colombia.
2Complejo Hospitalario Dr. Arnulfo Arias Madrid, servicio de gastroenterología. Caja de Seguro Social, Ciudad de Panamá, Panamá
The introduction of high resolution esophageal manometry has led to the revelation of previously unidentified patterns of esophageal function. Similarly, this diagnostic method has revealed topographic patterns of esophageal pressure which has led to the development of new tools for analysis and classification of esophageal motility disorders. Currently, the Chicago 3.0 classification has become a tool for analysis of the various esophageal motility disorders. In Colombia, the use of this study is spreading and growing. This article reviews of how to perform and interpret high resolution esophageal manometry and shows how to classify esophageal motility disorders according to the latest update of Chicago 3.0.
Keywords: Esophageal motility disorders; high resolution esophageal manometry; achalasia; Chicago 3.0.
Con la introducción de la manometría esofágica de alta resolución se revelaron patrones no identificados previamente de la función esofágica. De igual forma, este método diagnóstico adiciona patrones de presión topográfica de la presión esofágica, lo que lleva al desarrollo de nuevas herramientas para el análisis y clasificación de desórdenes motores esofágicos. En la actualidad, la clasificación de Chicago 3.0 es la herramienta de análisis de los diferentes trastornos motores esofágicos. En Colombia, cada día se ve el crecimiento en la realización de este estudio. El artículo propone hacer una revisión de cómo realizar e interpretar una manometría esofágica de alta resolución y clasificar los diferentes trastornos de la motilidad esofágica según la última actualización de la clasificación de Chicago 3.0.
Palabras clave: Desórdenes de motilidad esofágica; manometría esofágica de alta resolución; acalasia; Chicago 3.0
Introduction
Evaluation of esophageal and gastrointestinal motor function with manometric techniques became possible in the 1970s when Wyle Jerry Dodds and Ron Arndorfer developed the first manometry system. In the 1990s, Ray Clouse and his colleagues gave birth to high resolution manometry (HRM) by decreasing the space between sensors located along the conventional manometry pressure catheter from 5 cm to 1 cm, increasing the number of sensors and increasing the length of the sensed segment from the pharynx to the stomach, so that motor function of the upper esophageal sphincter (UES) and the lower esophageal sphincter (LES) could both be observed during every swallow. This offers a complete temporospatial description of esophageal motor function 1,2.
The first attempts to classify esophageal motility disorders using conventional manometry criteria were made by Spechler and Castell in 2001 based on a review data published in the literature up to that point. However, they recognized that the clinical significance of any observed manometric findings could be limited because many of the reported abnormalities were poorly correlated with symptoms and because management did not lead to improvement of symptoms 3.
The development of high resolution catheters and software that produces color coded tracings with pressure segments has revolutionized diagnostic evaluation of esophageal motor disorders and provide results which offer great advantages over those obtained from conventional manometry 4,5. This quickly led to the introduction of esophageal HRM and esophageal pressure topography (EPT) into the clinical research scenario and clinical practice. The increased use of HRM allowed an objective evaluation of EPT measures that were integrated into a new classification scheme of esophageal motor disorders known as the Chicago classification. After its first publication in 2009, it has been updated intermittently in an attempt to represent clinically relevant phenotypes 3,6. Its last update in 2014 is the Chicago 3.0 classification. Since then, several studies have been published that demonstrate that this new scheme results in an increased proportion of HRMs that are classified as normal because of decreasing diagnoses of minor esophageal motility disorders while the proportion of major motility disorders and obstructive disorders has remained unchanged 7,8.
Indications
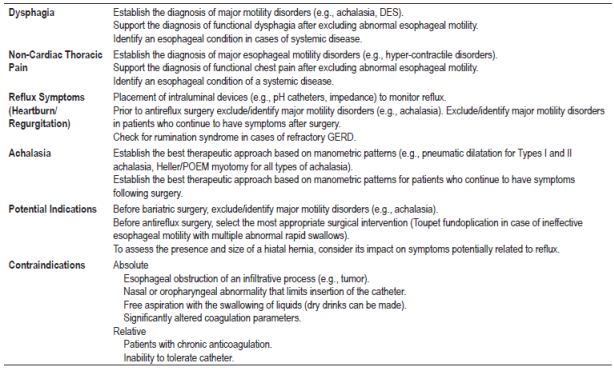
Esophageal manometry is the definitive test for evaluating esophageal motility. It is indicated for diagnostic evaluation of patients with non-obstructive dysphagia when endoscopic and radiological studies have not clarified the etiology of dysphagia, for evaluation of patients before anti-reflux surgery, for evaluation of non-cardiac chest pain, and for evaluation of symptoms after antireflux surgery (Table 1). The challenge for gastroenterologists and fellows in gastroenterology is to become sufficiently familiar with HRM to use it appropriately in clinical practice to achieve optimal management of patients with primary or secondary motility disorders 4,9,10.
The motility laboratory
Appropriate diagnosis of an esophageal motility disorder depends to a large extent on obtaining a high quality HRM study. This is of great importance because the surgical, medical or endoscopic management that is offered to the patient depends on the outcome. A high quality esophageal manometry laboratory requires the appropriate equipment and a dedicated staff in order to perform HRM studies 9.
Currently, equipment is available from several commercial companies including Sandhill Scientific Inc., (Highland Ranch, Colorado in the United States) and Medtronic from Given Imaging (Los Angeles, California in the United States) 11. Medtronic equipment was used in all the studies used for the development of the Chicago classification 9. The HRM catheter is solid state (considered to be an economical infusion system which requires less maintenance) and has an external diameter of 4.2 mm. It has 36 circumferential sensors separated by 1 cm intervals 4,11. This allows evaluation of intraluminal pressure throughout the entire length of the esophagus including the sphincters 1. Adequate maintenance of the equipment by trained personnel and scheduling of timely replacement of catheters are both very important.
Esophageal manometry studies can be performed by medical personnel, nurses or technicians trained in the area, but to perform high quality studies whoever performs the manometry must have the appropriate level of training and experience. Staff should have the ability to assess whether the study is appropriate, have sufficient knowledge to determine the appropriate position of the catheter in relation to the diaphragm, and be able to recognize common artifacts and equipment malfunctions 9.
How to perform a high quality study
Since esophageal HRM was introduced into clinical practice, technical and methodological changes have been developed which has required standardization and establishment of reference values and analytical criteria among laboratories 12. A high quality HRM study requires control of certain issues related to the patient and requires technical execution of the procedure, as described below.
Ideally, the patient should be instructed to refrain from eating solids for six hours prior to the procedure, and to refrain from ingesting any liquids for two hours prior to the procedure. In the case of suspicion of achalasia or a previous diagnosis, fasting time should be at least 12 hours. This decreases the risk of vomiting and aspiration during the introduction of the manometry catheter. Medications that can influence esophageal motility should be carefully evaluated and discontinued at least 3 days before the test if possible. These medications include calcium channel blockers, nitrates, prokinetics, loperamide, β-blockers, opioids, and anticholinergic agents 1,4,10.
Because this is a minimally invasive procedure, the patient must be given a detailed explanation about the technique used in the procedure and possible discomfort that may be experienced. Once the patient has approved the procedure, it is suggested that she or he sign an informed consent statement 1,9.
Prior to esophageal intubation, the manometry catheter should be calibrated. The calibration method varies according to the type of probe to be used and the manufacturer’s specifications 1.
The HRM catheter is placed transnasally. It is positioned by observing the appearance of a high pressure zone at the distal end of the LES and is adjusted so that at least 2 to 3 cm of the distal end of the catheter is below the level of the diaphragm. However, this is not always possible when there is a large hiatal hernia and in some patients with achalasia 1,9. One way to verify the correct placement of the catheter and to make sure that it has passed through the esophagogastric junction (EGJ) is to ask the patient to take deep breaths which makes it easier to identify the distal pressure zone and the pressure inversion point (PIP).
Once the catheter has been correctly positioned, basal pressures and the evaluation of contractile pattern and force of swallowing are recorded. A standard international protocol has been proposed for recording this information (Table 2).
Table 2 Standard protocol for high-resolution esophageal manometry and adjunct tests
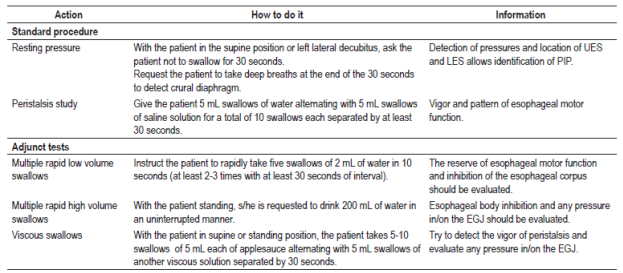
Adapted from: Savarino E, et al. Dig Liver Dis. 2016; 48 (10): 1124-35
Some authors have suggested that increasing the esophageal workload during manometry could increase the sensitivity of the investigation. The use of multiple rapid swallows is the simplest provocative maneuver (Table 2). After the last swallow of the series, the so-called peristaltic reserve, a robust esophageal contraction, is expected. An abnormal response consists of incomplete inhibition when fragments of contraction are seen during the expected period of inhibition or suboptimal contraction in which the sequence following multiple rapid swallows fails to demonstrate any increase of smooth muscle contractions. Multiple low volume rapid swallowing evaluates peristaltic reserve while swallowing large volumes can be used to identify increased resistance to flow 4,13.
Interpretation of hrm based on Chicago 3.0 criteria
HRM shows the resting pressure of the sphincters and esophageal motor activity triggered by swallowing 1. Although most analyses done with the software provided with the equipment are helpful, final interpretation needs to be developed by a competent and experienced clinician. The basic Gastroenterology Core Curriculum in the United States suggests two levels of training for interpretation of HRM: a basic level required for all gastroenterologists and intensive clinical training for those who provide HRM studies to patients 9. This level is required due to the high prevalence and health care burden of esophageal motor disorders 14. Despite this recommendation, most gastroenterology training programs do not provide formal training in gastrointestinal motility diagnosis.
Previous studies have found that diagnostic agreement for esophageal HRM between training personnel and doctors in practice is suboptimal. An inadequate diagnosis adversely impacts patient outcomes and health care costs. The GI core curriculum recommends completing 50 manometry studies to achieve competency, but a recent study of gastroenterologists in training found that less than 50% of training personnel had achieved expert competency after evaluating 50 HRM studies. This suggests that using a minimum volume of cases to assess competency for evaluating esophageal HRM is inadequate and that it would be more appropriate to establish cut-off points for evaluating HRM analysis competency for different levels 14,15.
HRM allows differentiation of basal pressure of the LES from the crural diaphragm contraction. Under normal conditions, these two pressure zones must coincide, and separation indicates the presence of a hiatal hernia. Similarly, the point where pressure changes during inspiration from negative pressure generated by intrathoracic pressure to positive pressure generated by intragastric pressure (the PIP) can be identified. This point indicates the division that the diaphragm creates between the thorax and the abdomen 1. Objective measures of esophageal function are immediately available after performing HRM and can be used to classify individual swallows and generate a diagnosis of esophageal motility 4. Therefore, stepwise interpretation of an HRM analysis is convenient, as discussed below.
Baseline pressure and function of the esophagogastric junction
The study begins with evaluation of the resting pressures of the UES and the LES (which are identified as two areas with increased pressure easily evidenced by a change in the color of the EPT), the morphology of the EGJ and whether or not a hiatal hernia exists 1. To achieve this, it is essential to correctly place the reference parameters within the analytical software (Figures 1 and 2). Two components make up the EGJ: the LES and the crural diaphragm. The morphology of the EGJ is classified into three types according to the level of separation that exists between the location of the LES and the PIP (which indicates the location of the crural diaphragm) (Figure 3):
Figure 1 HRM software reference points. The correct positioning of the reference points in the software is necessary to achieve a correct analysis of basal pressures and assessment of swallows. 1: upper edge of the LES 2: lower edge of the LES. The orange points followed by the dotted lines delimit the e-Sleeve for analysis of residual pressure in the EGJ during swallowing so it should cover the entire EGJ
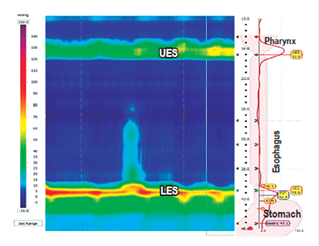
Figure 2 Evidence of pressure zones generated by the upper esophageal sphincter (UES) and the lower esophageal sphincter (LES)
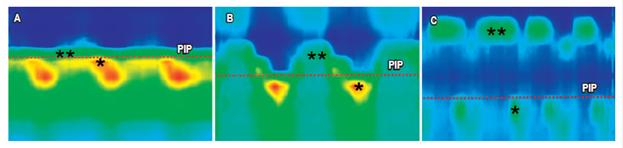
Figure 3 The morphology of the EGJ is classified into three types according to the degree of separation between the LES and the PIP. This indicates the point at which pressure through the EGJ during inspiration is reversed from intra-aortic negative to positive intragastric and which represents the location of the crural diaphragm. A. Type I: the LES and the crural diaphragm coincide. B. Type II: separation of less than 2 cm between the crural diaphragm and the LES. C. Type III:is separation of more than 2 cm between the crural diaphragm and the LES. * crural diaphragm; ** LES; PIP: red dotted line.
Type I: the LES and the crural diaphragm coincide
Type II: small spatial separation of less than two cm between the crural diaphragm and the LES
Type III: large spatial separation of more than two cm between the crural diaphragm and the LES 2.
At this point, whether or not relaxation of the EGJ is normal during swallowing must be determined. Integrated relaxation pressure (IRP) measures EGJ relaxation 9. The equipment measures IRP at ten seconds from the start of swallowing which is when relaxation of the UES begins. The IRP is the lowest average pressure in the EGJ during 4 of those 10 seconds. It can be continuous or discontinuous during a swallow (Figure 4) 1.
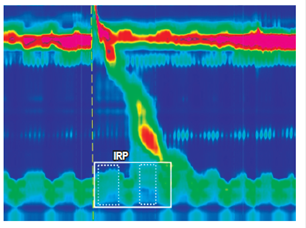
Figure 4 The IRP is the lowest continuous or discontinuous average pressure across the EGJ for 4 seconds (dotted squares) within the window of 10 seconds (continuous frame) during one swallow.
According to the new Chicago classification, it should be expressed as the median (rather than the mean) of the 10 swallows expressed in mm of Hg. The upper limit of normal for catheters of the Sierra design (Given Imaging) is 15 mm of Hg (Table 3) 9. A higher value means increased resistance to bolus transit in the EGJ which is considered pathological. Any pathological process, whether mechanical or functional, that prevents passage through the EGJ may increase IRP. Some of these alterations may be achalasia and conditions that behave like outflow obstructions such as neoplasms, benign stenoses, and fundoplication 1. We have tried to establish normal values of IRP after fundoplication in asymptomatic patients and found that one study determined that IRP may be higher than normal in those with Nissen-type fundoplication, but is similar to normal values in subjects with Toupet type fundoplication 16.
EPT measurement for assessment of individual swallows
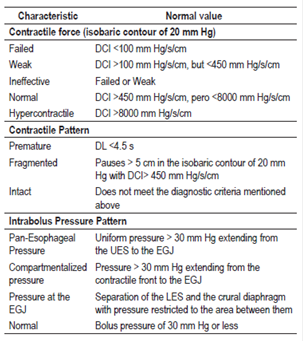
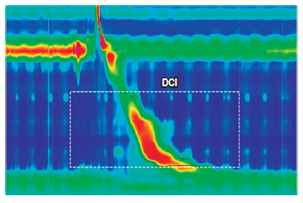
The main HRM measurements of esophageal peristalsis used in the Chicago 3.0 classification (Figure 5) are the distal contractile integral (DCI) and distal latency (DL) (Table 3).
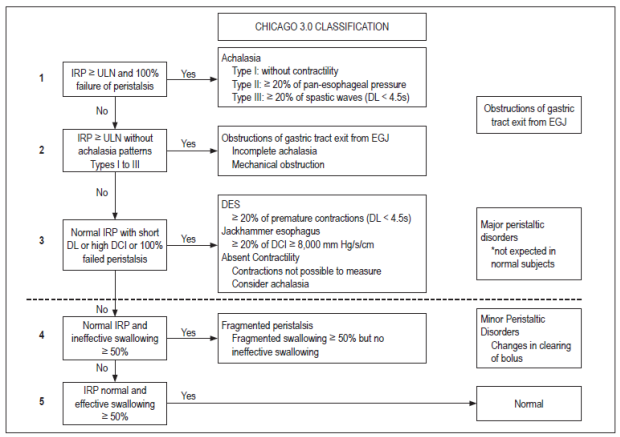
Figure 5 Algorithm for interpretation of esophageal HRM using Chicago 3.0 classification. Taken from: Kahrilas PJ, et al. Neurogastroenterol Motil. 2015; 27 (2): 160-74. ULN: upper limit of normal.
The DCI is a measure of the contractile (peristaltic) force of esophageal contraction and represents the amplitude x duration x length (mm Hg/s/cm) of the esophageal contraction in the isobaric contour of 20 mm Hg through pressures from proximal to distal 4. DCI is the determinant of hypercontractile swallowing (DCI> 8000 mm Hg/s/cm), weak swallowing (DCI <450 mm Hg/s/cm), and failed peristalsis (DCI <100 mm Hg/s/cm) 9.
DL is the time interval in seconds between the relaxation of the UES and the inflection point along the isobaric contour of 30 mm Hg where the velocity of propagation slows. This point is known as the contractile deceleration point (CDP), and it demarcates the tubular esophagus from the phrenic ampulla. DL is an indirect measure of swallowing inhibition and, therefore, of normal peristalsis. A measurement of less than 4.5 seconds defines a premature contraction (Figures 6 and 7)9.
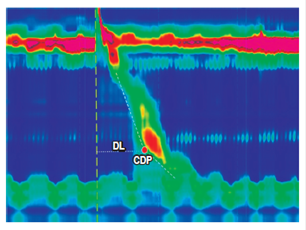
Figure 6 DL is the time interval in seconds between relaxation of the UES and the CDP (red dot). The CDP is the point along the isobaric contour of 30 mm Hg at which the speed of propagation slows down. It demarcates the tubular esophagus from the phrenic ampulla.
Peristaltic pauses
Peristaltic pauses are spatial gaps in peristaltic contraction defined by examining the integrity of the isobaric contour of 20 mm Hg from the UES to the EGJ. Peristaltic pauses are considered significant if they are more than 5 cm long 9.
Pressure patterns
Finally, abnormal pressure patterns are determined. Pressure develops when swallowed liquid is trapped between two contractile segments of the esophagus. It can be identified with a vertical isobaric pressure band. Abnormally high intrabolus pressure is a sign of altered mechanics of bolus transit and may be secondary to obstruction of the flow or to alterations in the distensibility of the esophageal wall. Pressure of more than 30 mm Hg that extends from the UES to the EGJ is called pan-esophageal pressure and is the defining characteristic of Type II achalasia. Compartmentalized pressure occurs between a peristaltic contraction and the EGJ, and indicates an obstruction to outflow.
Despite the development of consistent HRM technique and a standardized protocol, it has been demonstrated that technically imperfect studies are common in one third-level referral hospital and can occur in up to 21% of cases. Technically imperfect studies are considered to be those that are unable to cross the EGJ and/or those that have less than 7 evaluable swallows, sensor malfunctions, altered thermal compensation, and miscellaneous artifacts (vascular or cardiac). However, despite their technical limitations, these studies can still be interpreted, especially in the context of complementary endoscopic and radiographic data 11.
After analyzing ten swallows, the Chicago 3.0 classification can be used to determine the manometric diagnosis of the patient.
In the hierarchical scheme of the Chicago classification (Figure 5), identification of obstruction of outflow from the EGJ (defined by IRP> 15 mm Hg for catheters of Sierra design) is paramount. The presence or absence of this is the initial decision point in the diagnostic algorithm. If obstruction of outflow from the EGJ is accompanied by 100% of unsuccessful swallows or 20% of premature contractions, criteria for the diagnosis of achalasia are met.
Achalasia is further classified according to the pattern of contractility that accompanies obstruction of outflow:
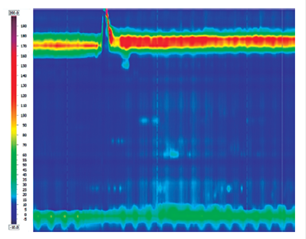
Figure 8 Type I achalasia (classical) is associated with the presence of IRP over 15 mm Hg) and 100% of failed swallows.
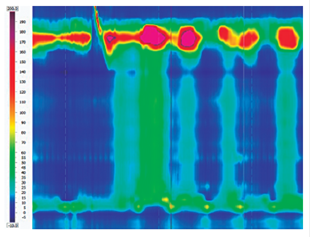
Figure 9 Type II achalasia is associated with IRP over 15 mm Hg and pan-esophageal pressure of more than 30 mm Hg that extends from the UES to the EGJ.
Increased IRP associated with a contractile pattern that does not meet the criteria for any type of achalasia defines an obstruction of outflow from the EGJ. This is a heterogeneous diagnosis with different differential diagnoses that include early or evolving achalasia, mechanical obstruction, hiatal hernia and pressure artifacts. Consequently, additional tests such as a barium esophagogram or endoscopic ultrasound should be considered before any therapeutic intervention is made 6,9.
If the median IRP is normal, the percentage of premature, hypercontractile and failed swallows can be used to identify major peristaltic disorders which generate patterns that are not observed in asymptomatic subjects. DES is defined by premature swallows, hypercontractile esophagus is defined by hypercontractile swallows (Figure 10), and failed contractility is designated if 100% of swallows fail 6,9.
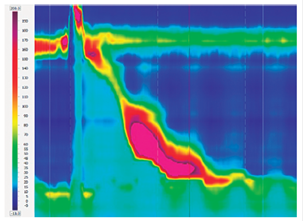
Figure 10 Hypercontractile esophagus (Jackhammer esophagus) is defined by hypercontractile swallows (DCI> 8000 mm Hg/s/cm).
A minor disturbance of peristalsis is established if the median IRP is normal, a major peristaltic disorder is excluded and if more than 50% of swallows are weak or unsuccessful (ineffective esophageal motility) or if more than 50% of swallows have large peristaltic pauses (fragmented peristalsis). Both minor disorders can be seen in patients with dysphagia or reflux symptoms. However, they can also be seen in asymptomatic controls, so their clinical relevance remains unclear.
Finally, if the previously described motility disorders are ruled out and 50% of swallows are normal, a diagnosis of normal esophageal motility is made 6,9.
Referencias
1. Hani A, Leguízamo AM, Carvajal JJ, et al. Cómo realizar e interpretar una manometría esofágica de alta resolución. Rev Col Gastroenterol. 2015;30(1):74-83. [ Links ]
2. Conklin JL. Evaluation of esophageal motor function with high-resolution manometry. J Neurogastroenterol Motil. 2013;19(3):281-94. https://doi.org/10.5056/jnm.2013.19.3.281 [ Links ]
3. Carlson DA, Pandolfino JE. High-resolution manometry and esophageal pressure topography: filling the gaps of convention manometry. Gastroenterol Clin North Am. 2013;42(1):1-15. https://doi.org/10.1016/j.gtc.2012.11.001 [ Links ]
4. Savarino E, de Bortoli N, Bellini M, et al. Practice guidelines on the use of esophageal manometry -A GISMAD-SIGE-AIGO medical position statement. Dig Liver Dis. 2016;48(10):1124-35. https://doi.org/10.1016/j.dld.2016.06.021 [ Links ]
5. Çelebi A. High-resolution manometry versus conventional manometry in diagnosis of patients with nonobstructive dysphagia. Turk J Gastroenterol. 2016;27(6):566-7. https://doi.org/10.5152/tjg.2016.0007 [ Links ]
6. Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160-74. https://doi.org/10.1111/nmo.12477 [ Links ]
7. Patel A, Cassell B, Sainani N, et al. Comparison of motor diagnoses by Chicago Classification versions 2.0 and 3.0 on esophageal high-resolution manometry. Neurogastroenterol Motil. 2017;29(7):1-8. [ Links ]
8. Monrroy H, Cisternas D, Bilder C, et al. The Chicago Classification 3.0 results in more normal findings and fewer hypotensive findings with no difference in other diagnoses. Am J Gastroenterol. 2017;112(4):606-12. [ Links ]
9. Carlson DA, Kahrilas PJ. How to effectively use high-resolution esophageal manometry. Gastroenterology. 2016;151(5):789-92. https://doi.org/10.1053/j.gastro.2016.09.024 [ Links ]
10. Gyawali CP, Patel A. Esophageal motor function: technical aspects of manometry. Gastrointest Endosc Clin N Am. 2014;24(4):527-43. https://doi.org/10.1016/j.giec.2014.06.003 [ Links ]
11. Roman S, Kahrilas PJ, Boris L, et al. High-resolution manometry studies are frequently imperfect but usually still interpretable. Clin Gastroenterol Hepatol. 2011;9(12):1050-5. https://doi.org/10.1016/j.cgh.2011.08.007 [ Links ]
12. Ruiz de León San Juan A, Ciriza de Los Ríos C, Pérez de la Serna Bueno J, et al. Practical aspects of high resolution esophageal manometry. Rev Esp Enferm Dig. 2017;109(2):91-105. [ Links ]
13. Elvevi A, Mauro A, Pugliese D, et al. Usefulness of low- and high-volume multiple rapid swallowing during high-resolution manometry. Dig Liver Dis. 2015;47(2):103-7. https://doi.org/10.1016/j.dld.2014.10.007 [ Links ]
14. Yadlapati R, Keswani RN, Dunbar KB, et al. Benchmarks for the interpretation of esophageal high-resolution manometry. Neurogastroenterol Motil. 2017;29(4):1-7. [ Links ]
15. Yadlapati R, Keswani RN, Ciolino JD, et al. A system to assess the competency for interpretation of esophageal manometry identifies variation in learning curves. Clin Gastroenterol Hepatol. 2017;15(11):1708-14. [ Links ]
16. Weijenborg PW, Savarino E, Kessing BF, et al. Normal values of esophageal motility after antireflux surgery; a study using high-resolution manometry. Neurogastroenterol Motil. 2015;27(7):929-35. [ Links ]
Received: June 15, 2017; Accepted: October 06, 2017











 text in
text in