Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.32 no.4 Bogotá Oct./Dec. 2017
https://doi.org/10.22516/25007440.184
Case report
Subcardial Gastric Diverticula: A Rare Endoscopic Finding
1Médico internista, gastroenterólogo. Miembro internacional ACP, AGA, ASGE. Hospital Emiro Quintero Cañizares, Ocaña, Santander, Colombia. Correo: royerogastro@hotmail.com
Gastric diverticula are uncommon and are usually diagnosed incidentally by radiological or endoscopic methods. They are divided into congenital and acquired diverticula and are usually asymptomatic. Clinical expression ranges from nonspecific abdominal pain to more dramatic clinical conditions such as perforations and bleeding. We present a case of three gastric diverticula in a patient with a history of functional dyspepsia, cholecystectomy and Nissen fundoplication. Treatment was conservative.
Keywords: Diverticulum; stomach; Nissen fundoplication
Los divertículos gástricos (DG) son un hallazgo infrecuente. Suelen ser diagnosticados incidentalmente por métodos radiológicos o endoscópicos; se dividen en congénitos y adquiridos; y generalmente son asintomáticos, pero su expresión clínica va desde dolor abdominal inespecífico hasta cuadros clínicos más dramáticos como perforación y sangrado. Se presenta un caso de 3 DG en un paciente con antecedentes de colecistectomía y funduplicatura de Nissen con historia de dispepsia funcional. Su tratamiento fue conservador.
Palabras clave: Divertículo; estómago; funduplicatura de Nissen
Introduction
Gastric diverticula are dilations that protrude from the gastric wall 1. Their prevalence ranges from 0.04% to 2.6%, and they can be congenital or acquired 2,3,4. Most are asymptomatic, but they can manifest as dyspepsia, vomiting and abdominal pain or in forms as severe as bleeding or perforation 5,6. In patients with symptomatic or complicated gastric diverticula, laparoscopic resection is a surgical approach that has excellent results 7.
We report a case of diverticular disease in the gastric fundus in a patient with a history of Nissen fundoplication and cholecystectomy who has had long-standing dyspepsia. This is combination of a rare entity with a rare association. Our findings are presented together with a review of the medical literature.
Case description
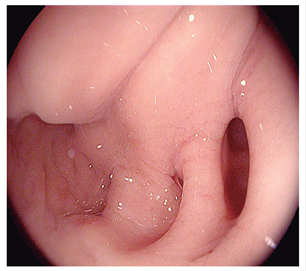
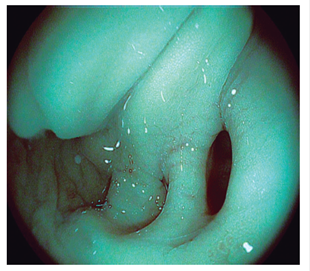
A 65-year-old male patient was examined after suffering from dyspepsia manifested by epigastric pain and postprandial difficulty for several years. He said he had never used nonsteroidal anti-inflammatory drugs (NSAIDs). His medical record showed that he had undergone Nissen fundoplication to treat gastroesophageal reflux and hiatal hernia twenty five years before the examination, had had a cholecystectomy to treat cholecystitis and vesicular lithiasis eight years prior to the examination, and had undergone upper digestive endoscopy five years prior to the examination which had found no evidence of diverticula. Physical examination found the following: weight: 78 kilos, height: 1.69 m, and body mass index (BMI): 27.36. There were no signs of any pathology. After patient provided informed consent, upper digestive endoscopy was performed (Figures 1,2 and 3) and found that the diameter of the esophageal lumen was slightly enlarged, there were folds around the posterior gastric cardia related to the Nissen fundoplication, and there were three small saccular orifices measuring between 0.5 cm and 1 cm without signs of recent bleeding. The rest of the endoscopy suggested superficial chronic gastritis. Biopsies taken according to Sidney’s protocol showed Stage I for both the Operative Link of Gastritis Assessment (OLGA) and Gastric Intestinal Metaplasia Assessment (OLGIM). The patient tested positive for helicobacter pylori in the antrum and negative in the corpus. The patient was treated with sequential therapy with amoxicillin, clarithromycin and tinidazole for 14 days to eradicate H. pylori and received treatment for symptoms of dyspepsia. Clinical monitoring of the patient continues.
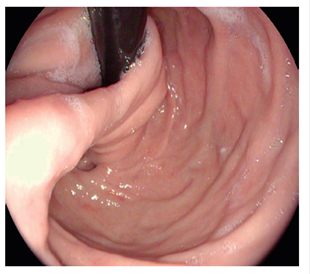
Figure 1 Retroversion view of subcardial folds in relation to fundoplication. A single diverticulum can be seen.
Discussion
Gastric diverticula are rare, although their discovery varies according to the diagnostic method. In a large series of 14,428 patients who underwent a thoracic and abdominal CT scans, 18 gastric diverticula were incidentally diagnosed for a prevalence of 0.12% 8. A recent review found a prevalence of 0.04% and in radiological studies with contrast and a prevalence of 0.1% -0.11% in endoscopic procedures 9. Meeroff et al. reported an incidence of 0.2% in autopsies 3.
Gastric diverticula can be congenital or acquired. Congenital diverticula involve all the layers of the gastric wall and are primarily located mainly in the posterior wall near the gastroesophageal junction. In this posterior location near the cardia, the gastric wall has been found to be less resistant due to the absence of longitudinal muscle fibers and the peritoneum. Consequently, prolonged increases in intra-abdominal or intragastric pressure can lead to the appearance of a diverticular sac 10. Acquired diverticula, or pseudo-diverticula, affect only the mucosa without compromising the muscular layer. They are subdivided into:
Diverticula generated by increased intraluminal pressure due to pregnancy, pyloric obstruction, severe vomiting, coughing, constipation or foreign bodies or to the erosive effects of gastric ulcers or carcinomas.
Diverticula produced by traction due to gastric adhesions resulting from inflammatory lesions of the spleen, gallbladder, pancreas, liver, peritoneum or stomach surgery. They are usually located near the gastric antrum 7,9,11,12.
Many diverticula are detected incidentally by computerized axial tomography (CAT). They are recognized as cystic lesions with a thin wall filled with air and fluid and located behind the stomach in the left paravertebral region between the spleen, the adrenal gland and the left crura of the diaphragm 8. If a diverticulum does not contain air, it can be misinterpreted, especially as a cystic lesion of the left adrenal gland 12,13. Differential diagnosis should also consider anatomical variations of normal structures or pathologies of adjacent organs such as accessory spleens, liver tumors, fluid-filled colon, tortuous splenic arteries or veins, exophytic renal masses in the upper kidney, pancreatic masses, increased adrenal fat and thickening of the left diaphragmatic crura 13. For these reasons, a combination of endoscopic, radiological, barium and endosonographic studies is recommended to corroborate the diagnosis of a gastric diverticulum 14.
A number of case reports have shown that gastric diverticula can manifest with abdominal symptoms such as vomiting and abdominal pain and can be associated with dyspepsia 16, peptic ulcers 11 and gastroesophageal reflux 5,15,17,18. They can also be complicated by bleeding and perforations 19,20.
Initial medical management for symptomatic diverticula includes the use of antacids, proton pump inhibitors and a soft diet 21. If diverticula continue to have severe symptoms despite pharmacological treatment, or are complicated because of large size (diameters greater than 4 cm), laparoscopic surgery indicated 22. This technique is currently well accepted and is minimally invasive and highly effective 23,24.
Conclusions
Gastric diverticula are a rare pathology and are usually asymptomatic. In the case described, and according to the medical literature reviewed, subcardial diverticular formations may be related to prior surgery. In addition, they can contribute to the upper digestive tract symptoms described. Although no radiological study was performed for this patient, it is important to note that when left adrenal masses are diagnosed in a CT scan, the diagnosis of gastric diverticula in the gastric fundus should be considered since it is the main differential diagnosis when these imaging findings are presented. In diverticula larger than 4 cm, laparoscopy has been indicated as definitive treatment because they have a high probability of being complicated by perforations or bleeding.
REFERENCES
1. Podda M, Atzeni J, Messina Campanella A, Saba A, Pisanu A. Syncope with surprise: an unexpected finding of huge gastric diverticulum. Case Rep Surg. 2016;2016:1941293. https://doi.org/10.1155/2016/1941293 [ Links ]
2. Palmer ED. Gastric diverticula. Int Abstr Surg. 1951;92(5):417-28. [ Links ]
3. Meeroff M, Gollán JR, Meeroff JC. Gastric diverticulum. Am J Gastroenterol. 1967;47(3):189-203. [ Links ]
4. Goldberg E, Raufman JP. Stomach and duodenum: anatomy and structural anomalies. En: Podolsky D, Camilleri M, Fitz JG; et al (editores). Yamada’s textbook of gastroenterology. 6.a edición. Oxford: Wiley-Blackwell; 2015. pp. 60-72. [ Links ]
5. Mohan P, Ananthavadivelu M, Venkataraman J. Gastric diverticulum. CMAJ. 2010;182(5):E226. https://doi.org/10.1503/cmaj.090832 [ Links ]
6. Hajini FF, Husain M, Bhat A, Bukhari SI. Gastric diverticulum a rare endoscopic finding. BMJ Case Rep. 2014 Apr 1;2014. pii: bcr2013202887. [ Links ]
7. Marano L, Reda G, Porfidia R, et al. Large symptomatic gastric diverticula: two case reports and a brief review of literature. World J Gastroenterol. 2013;19(36):6114-7. https://doi.org/10.3748/wjg.v19.i36.6114 [ Links ]
8. Schramm D, Bach AG, Zipprich A, et al. Imaging findings of gastric diverticula. ScientificWorldJournal. 2014;2014:923098. https://doi.org/10.1155/2014/923098 [ Links ]
9. Rashid F, Aber A, Iftikhar SY. A review on gastric diverticulum. World J Emerg Surg. 2012;7(1):1. https://doi.org/10.1186/1749-7922-7-1 [ Links ]
10. Puente J, Aguayo J, Parilla P, et al. Divertículos gástricos. En: Balibrea Cantero JL (editor). Tratado de cirugía (vol. II): patología quirúrgica. 1.ª edición. Madrid: Marban Libros; 2002. pp. 2095-101. [ Links ]
11. Tsitsias T, Finch JG. Gastric diverticulum of the prepyloric region: a rare presentation of gastric diverticulum. Case Rep Gastroenterol. 2012;6(1):150-4. https://doi.org/10.1159/000338067 [ Links ]
12. Zuluaga A, Ochoa J, Bustamante S, et al. Divertículos y pseudodivertículos del tracto digestivo superior: hallazgos por tomografía computarizada multidetector (TCMD): serie de casos. Rev Colomb Radiol. 2015;26(1):4139-44. [ Links ]
13. Feng YE, Zhang Z. Gastric diverticulum simulating a left adrenal mass: a case report and review of the literature. Oncol Lett. 2015;10(4):2477-2480. https://doi.org/10.3892/ol.2015.3559 [ Links ]
14. Simon M, Zuber-Jerger I, Schölmerich J. True gastric diverticulum. Dig Liver Dis. 2009;41(5):370. https://doi.org/10.1016/j.dld.2008.06.016 [ Links ]
15. Mahafza WS, Taib AA, Shahait AD, et al. Chronic gastritis in a gastric diverticulum misdiagnosed as a left adrenal mass. Indian J Surg. 2015;77(Suppl 1):150-2. https://doi.org/10.1007/s12262-015-1210-2 [ Links ]
16. Eitzen K, Eslick GD, Daneshjoo R. Dyspepsia and gastroesophageal reflux symptoms predominate in gastric diverticulum. J Dig Dis. 2012;13(6):335-6. https://doi.org/10.1111/j.1751-2980.2012.00595.x [ Links ]
17. Moy BT, Marchioni Beery RM, Birk JW. Gastric diverticulum: an unusual endoscopic finding. ACG Case Rep J. 2016;3(3):150-1. https://doi.org/10.1503/cmaj.090832 [ Links ]
18. Villazón DO, Hernández LA, Badin AV, et al. Divertículo gástrico: caso clínico y revisión de la literatura. Rev Mex Cir Endoscop. 2013;14(4):183-5. [ Links ]
19. Gibbons CP, Harvey L. An ulcerated gastric diverticulum--a rare cause of haematemesis and melaena. Postgrad Med J. 1984;60(708):693-5. https://doi.org/10.1136/pgmj.60.708.693 [ Links ]
20. Chen JH, Su WC, Chang CY, et al. Education and imaging. Gastrointestinal: bleeding gastric diverticulum. J Gastroenterol Hepatol. 2008;23(2):336. [ Links ]
21. Zelisko A, Rodriguez J, El-Hayek K, et al. Laparoscopic resection of symptomatic gastric diverticula. JSLS. 2014;18(1):120-4. https://doi.org/10.4293/108680813X13693422520648 [ Links ]
22. Muis MO, Leitao K, Havnen J, et al. Gastric diverticulum and halitosis-a case for surgery? Int J Surg Case Rep. 2014;5(7):431-3. https://doi.org/10.1016/j.ijscr.2014.04.029 [ Links ]
23. Tebala GD, Camperchioli I, Tognoni V, et al. Laparoscopic treatment of a gastric diverticulum. Eur Rev Med Pharmacol Sci. 2010;14(2):135-8. [ Links ]
24. DuBois B, Powell B, Voeller G. Gastric diverticulum: “a wayside house of ill fame” with a laparoscopic solution. JSLS. 2012;16(3):473-7. https://doi.org/10.4293/108680812X13462882736330 [ Links ]
Received: April 04, 2017; Accepted: October 06, 2017











 text in
text in