Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.32 no.4 Bogotá oct./dic. 2017
https://doi.org/10.22516/25007440.185
Case report
A Case Report of Fibro-Stenotic Crohn’s Disease in the Middle Ileum as the Initial Manifestation
1Gastroenterólogo, servicio de gastroenterología y hepatología. Hospital Universitario Fundación Santa Fe de Bogotá, Bogotá D. C., Colombia
2Cirujano de colon y recto, Departamento de Cirugía. Hospital Universitario Fundación Santa Fe de Bogotá, Bogotá D. C., Colombia
3Patóloga, Hospital Universitario Fundación Santa Fe de Bogotá. Profesora de la Universidad de los Andes, Bogotá D. C., Colombia
4Residente de tercer año, especialización en Medicina Interna. Hospital Universitario Fundación Santa Fe de Bogotá, Bogotá D. C., Colombia
Crohn’s disease (CD) is an inflammatory bowel disease that can affect the entire gastrointestinal tract. The small intestine is affected in about 50% of patients among whom the terminal ileum is the area most commonly affected.
Intestinal stenosis is a common complication in CD and approximately 30% to 50% of patients present stenosis or penetrating lesions at the time of diagnosis. Because conventional endoscopic techniques do not allow evaluation of small bowel lesions, techniques such as enteroscopy and endoscopic video-capsule were developed. Each has advantages and indications.
We present the case of a patient with CD with localized fibrostenosis in the middle ileum which is not a frequent site for this type of lesion.
Keywords: Crohn’s disease; fibrostenosis; small intestine; endoscopic video-capsule; enteroscopy
La enfermedad de Crohn (EC) es una enfermedad inflamatoria intestinal que puede afectar todo el tracto gastrointestinal; el intestino delgado es el segmento afectado en cerca del 50% de los pacientes, en los cuales el íleon terminal es el área más comúnmente comprometida por la enfermedad.
Las estenosis intestinales son una complicación frecuente en la EC y aproximadamente 30% a 50% de los pacientes presentan estenosis o lesiones penetrantes al momento del diagnóstico. Las técnicas endoscópicas convencionales no permiten evaluar las lesiones del intestino delgado; es por esto que se desarrollaron técnicas como la enteroscopia y la videocápsula endoscópica, teniendo cada una de ellas sus ventajas e indicaciones.
Se presenta un caso de un paciente con EC con fibroestenosis localizada en el íleon medio. No es una localización frecuente para este tipo de lesiones.
Palabras clave: Enfermedad de Crohn; fibroestenosis; intestino delgado; videocápsula endoscópica; enteroscopia
Crohn’s disease (CD) is a chronic inflammatory bowel disease that causes symptoms such as abdominal pain, diarrhea, and bloody stools. It can affect any part of the gastrointestinal tract but compromises the small intestine in 40% to 60% of cases 1. In the small intestine, the terminal ileum is the most commonly affected area. Proximal localization is rare, but it has been reported in up to 10% of patients 2.
We present the case of a 65-year-old man with no previous relevant medical history who was examined after suffering generalized abdominal pain and distension associated with vomiting. His vomit had the appearance of coffee grounds. Bowel obstruction was documented through plain abdominal radiography and confirmed by a CT scan which showed nonspecific structural changes in distal ileal loops with no signs of loop serious damage (Figure 1). Complementary paraclinical tests showed hypochromic microcytic anemia, so the patient was questioned again and reported isolated previous episodes of melena and endoscopy and total colonoscopy which had found no evidence of pathological lesions.
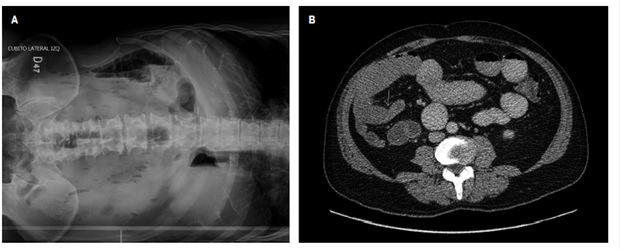
Figure 1 A. Plain abdominal x-ray; and B. Sagittal section of abdominal CT scan with contrast. Both images show intestinal obstruction and nonspecific structural changes in the distal ileal loops without signs of serious damage to loops.
Because of suspected small bowel bleeding, an endoscopic videocapsule was used to examine the small intestine. It showed stenosis and localized ulceration in the middle ileum without active bleeding (Figure 2). Based on these findings, retrograde double-balloon enteroscopy was scheduled. A unenterable concentric stenosis with a diameter of approximately 8 mm with ulceration in the lower part of the ileocecal valve was seen at 190 cm. The border was free, without bleeding, but covered with fibrin (Figure 3). During enteroscopy, biopsies of the stenosis were taken and a submucosal wheal was made with abundant saline solution. This point was then marked 3 cm distal from the site of the stenosis with Chinese ink to facilitate future location.
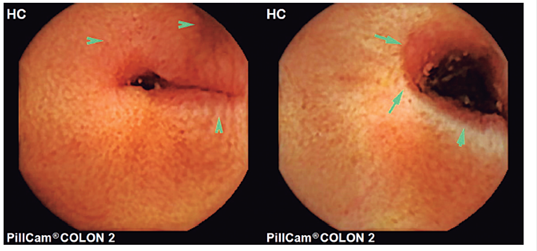
Figure 2 Videocapsule showing the presence of stenosis and ulcer located in the middle ileum without active bleeding.
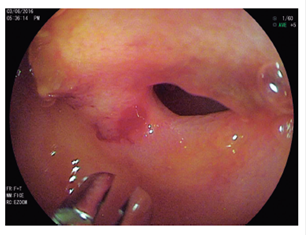
Figure 3 Retrograde enteroscopy shows concentric stenosis at 190 cm upstream of the ileocecal valve with ulceration of the free border but without evidence of active bleeding.
The pathology report showed that the lesion was compatible with CD. The case was discussed in the medical board with the participation of the gastroenterology service and a colon and rectal surgeon. It was decided to perform elective surgical resection of the stenotic segment since fibrostenosis with a high risk of obstruction but without evidence of other lesions in the rest of the small intestine had been documented.
Laparoscopic surgery showed the presence of ileum stenosis of approximately 1 cm with fatty infiltration on the serosa and the adjacent tattoo. The pathology report from the surgical specimen described alteration of the architecture of the small bowel wall with focal loss of the villi with ulceration, shortening and villous enlargement; slightly distorted crypts with decreased goblet cells: fibrosis of the lamina propria with increased lymphoplasmacytic infiltration; metaplasia of the submucosal glands and hypertrophy of nerve fibers. These findings are compatible with chronic inflammatory bowel disease of the CD type in the active phase (Figure 4).
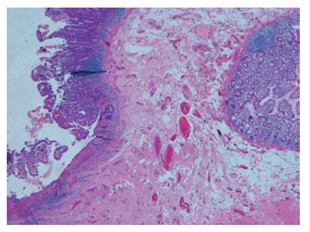
Figure 4 Hematoxylin and eosin 4X. Bowel wall sample showing altered architecture. To the left, there is ulceration with lymphoplasmacytic infiltrate and lymphoid accumulation and an area of submucosal fibrosis. On the right there are irregular glands, with pseudo-pyloric metaplasia.
During outpatient follow-up, the patient had no new episodes of abdominal pain or symptoms suggestive of intestinal obstruction. He continues to take iron orally for iron deficiency anemia and to return for annual follow-up endoscopic studies. One year after the procedure, everything was within normal limits.
The incidence of CD has increased in the last 50 years, but its clinical behavior remains very heterogeneous. Diagnosis must take into account clinical, endoscopic, histopathological and imaging findings making endoscopy essential for taking biopsy samples to confirm diagnosis of this disease histologically 1,3.
Intestinal stenosis is a frequent complication of CD: it has been described in up to 40% of patients with localized disease in the ileum 4, and in approximately 30% to 50% of patients who have stenosis or penetrating injuries at the time of treatment 5. The clinical relevance of these stenoses is due to the fact that up to 60% of cases require surgery within the first 20 years after diagnosis 6.
Since CD is a transmural disease, it affects all layers of the intestine. It often leads to protein deposits in the extracellular matrix that alter the architecture of the intestinal segments involved 5. Stenosis is the result of chronic inflammation that leads to tissue remodeling, hypertension of the mesenchymal cells, hyperplasia and fibrosis of the segments affected by inflammatory bowel disease. This is a consequence of a process of scarring after the initial injury and the inflammatory response that occurs in genetically susceptible patients 1,7. Stenoses with a purely inflammatory component benefit from treatment with anti-inflammatories that reduce edema. Endoscopic dilation and surgery are indicated as complementary treatment, if fibrotic component predominates in lesions because it does not respond to medical treatment 3.
Conventional endoscopic techniques do not allow evaluation of small bowel lesions secondary to CD that are located distal to the duodenum or proximal to the terminal ileum. For this reason techniques such as enteroscopy and endoscopic videocapsule have been developed. The main advantage of the capsule is that it performs a complete evaluation of the small intestine with a high diagnostic yield. Nevertheless, it is incapable of taking samples and, due to the risk of impaction, should only be used in cases where stenosis is suspected. The advantages of enteroscopy are that biopsy samples can be taken and therapeutic procedures can be performed 8.
Endoscopic studies, which only allow evaluation when there is endoluminal involvement due to disease, can be complemented with imaging studies that allow evaluation of the bowel wall and adjacent tissues. Intestinal ultrasound focuses on detection of intestinal wall thickening, increased vascularization through Doppler, and stenosis and extramural lesions. CT enterography allows detection of stenosis with or without proximal dilation, as well as signs of penetrating diseases such as fistulas or extraluminal abscesses. Magnetic resonance enterography has the advantages of being radiation-free and having different acquisition protocols which allow quantitative and qualitative evaluation of the activity and severity of disease. The method chosen depends on availability and experience in carrying out these studies 4.
For appropriately selected patients, endoscopic balloon dilation can be used to treat cases of short, uncomplicated stenoses, ileal-colonic or colonic anastomoses, but the risk of perforation during the procedure must be taken into account 5. Extensive intestinal resections should be avoided due to possible diarrhea and malabsorption, complications related to small intestine. For this reason, more conservative techniques have been developed that limit resection to the stenosis followed by a longitudinal closure. A laparoscopic approach is preferable for reducing the frequency of adhesions and incisional hernias with good clinical recovery 9,10.
Referencias
1. Kim M, Jang HJ. The role of small bowel endoscopy in small bowel Crohn’s disease: when and how? Intest Res. 2016;14(3):211-7. https://doi.org/10.5217/ir.2016.14.3.211 [ Links ]
2. Van Assche G, Dignass A, Panes J, et al. The second European evidence-based Consensus on the diagnosis and management of Crohn’s disease: Definitions and diagnosis. J Crohns Colitis. 2010;4(1):7-27. [ Links ]
3. Siegmund B. Medical Therapy of fibrostenotic Crohn’s disease. Viszeralmedizin. 2015;31(4):259-64. [ Links ]
4. Bettenworth D, Nowacki TM, Cordes F, et al. Assessment of stricturing Crohn’s disease: Current clinical practice and future avenues. World J Gastroenterol. 2016;22(3):1008-16. [ Links ]
5. Rieder F, Latella G, Magro F, et al. European Crohn’s and colitis organisation topical review on prediction, diagnosis and management of fibrostenosing Crohn’s disease. J Crohns Colitis. 2016;10(8):873-85. [ Links ]
6. Peyrin-Biroulet L, Harmsen WS, Tremaine WJ, et al. Surgery in a population-based cohort of Crohn’s disease from Olmsted County, Minnesota (1970-2004). Am J Gastroenterol. 2012;107(11):1693-701. [ Links ]
7. Li C, Kuemmerle JF. Mechanisms that mediate the development of fibrosis in patients with Crohn’s disease. Inflamm Bowel Dis. 2014;20(7):1250-8. [ Links ]
8. Park SJ, Kim WH. A look into the small bowel in Crohn’s disease. Clin Endosc. 2012;45(3):263-8. [ Links ]
9. Thienpont C, Van Assche G. Endoscopic and medical management of fibrostenotic Crohn’s disease. Dig Dis. 2014;32 Suppl 1:35-8. https://doi.org/10.1159/000367824 [ Links ]
10. Nasr JY, Lloyd J, Yadav D. An unusual cause of fibrostenotic terminal ileal disease. Gastroenterology. 2011;141(3):e5-6. [ Links ]
Received: April 06, 2017; Accepted: October 06, 2017











 texto en
texto en 


