Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.1 Bogotá ene./mar. 2018
https://doi.org/10.22516/25007440.230
Review articles
Probiotics in Acute, Antibiotic-associated and Nosocomial Diarrhea: Evidence in Pediatrics
1Médico, asistente de investigación, Universidad de los Andes. Bogotá D. C., Colombia. PediAFe, grupo de investigación
2Médico gastroenterólogo, nutriólogo pediatra, epidemiólogo clínico, Hospital Universitario Fundación Santa Fe de Bogotá. Bogotá D. C., Colombia. Universidad de los Andes. PediAFe, grupo de investigación
Introduction:
Probiotics are live microorganisms which, when administered in adequate amounts, provide beneficial action in humans. There are numerous studies about their use to treat diarrhea in pediatrics, so it is necessary to evaluate the evidence.
Methods:
We reviewed metaanalyses and systematic reviews in the last ten years about the use of probiotics to treat acute diarrhea, diarrhea associated with antibiotics and Clostridium difficile and nosocomial diarrhea.
Results:
Metaanalyses show that treatment of acute diarrhea with probiotics decreases duration by one day (95% CI: 15.9 to 33.6 hours) and reduces a risk of prolongation in the following four to seven days. They provide strong recommendations with moderate evidence for Lactobacillus rhamnosus GG and Saccharomyces boulardii. For diarrhea associated with antibiotics and Clostridium difficile, meta-analyses show risk reduction of between 50% and 60%, with strong recommendations for Lactobacillus rhamnosus GG and Saccharomyces boulardii with an NNT of 10 (95% CI: 7 to 12). For nosocomial diarrhea, moderate evidence was found for the use of Lactobacillus rhamnosus GG, mainly in reducing the risk of symptomatic gastroenteritis due to rotavirus. Currently, sufficient evidence does not exist to give recommendation for strains S. thermophiles and B. bifidum.
Conclusion:
For reducing the duration and reducing the risk of prolongation of acute diarrhea, evidence exists only for Lactobacillus rhamnosus GG and Saccharomyces boulardii. In addition, they reduce the risk of diarrhea associated with antibiotics by 50% to 60%. There is moderate evidence that Lactobacillus rhamnosus GG reduces the risk of nosocomial diarrhea.
Keywords: Probiotics; pediatrics; diarrhea; antibiotics; hospital infections
Introducción:
los probióticos son microorganismos vivos que, administrados en cantidades adecuadas, proveen una acción benéfica en el ser humano. Existen numerosos estudios acerca de su uso en enfermedad diarreica en pediatría, por lo que se hace necesario evaluar la evidencia.
Métodos:
se realizó una revisión de la literatura incluyendo solo metaanálisis y revisiones sistemáticas en los últimos 10 años acerca del uso de probióticos en diarrea aguda, diarrea asociada a antibióticos y Clostridium difficile, y diarrea nosocomial.
Resultados:
en diarrea aguda, los metaanálisis muestran disminución de la duración en un día (intervalo de confianza [IC] 95%; 15,9 a 33,6 horas) y disminución del riesgo de prolongación en los siguientes 4 y 7 días, con recomendaciones fuertes y evidencia moderada para Lactobacillus rhamnosus GG y Saccharomyces boulardii. En diarrea asociada a antibióticos y a C. difficile, los metaanálisis mostraron reducción del riesgo entre el 50% y 60%, con recomendación fuerte para L. rhamnosus GG y S. boulardii con un número necesario a tratar (NNT) de 10 (IC 95%; 7-12). En diarrea nosocomial, se encontró evidencia moderada con el uso de L. rhamnosus GG, principalmente en reducción del riesgo de gastroenteritis sintomática por rotavirus. Sin evidencia suficiente para dar recomendación para las cepas Streptococcus thermophilus y Bifidobacterium bifidum.
Conclusión:
solo existe evidencia con los probióticos L. rhamnosus GG y S. boulardii en reducción de la duración y disminución del riesgo de prolongación de diarrea aguda, así como reducción del riesgo entre 50% y 60% de diarrea asociada a antibióticos. Existe evidencia moderada con L. rhamnosus GG, en la reducción de riesgo de diarrea nosocomial.
Palabras clave: Probióticos; pediatría; diarrea; antibióticos; infección hospitalaria
Introduction
In 2014, the International Scientific Association for Probiotics and Prebiotics (ISAPP) ratified and established the definition previously proposed by the World Health Organization (WHO) of probiotics as “…live microorganisms which when administered in adequate amounts confer a health benefit on the host.” 1
Probiotics’ multiple physiological actions in the human body include restoration of the gut microbiota by occupying physiological niches to prevent the colonization of opportunistic pathogens, 2 improvement of the bioavailability of vitamins such as vitamin K, B12 and pyridoxine, and synthesis of other micronutrients such as linoleic acid. 3 They aid intestinal transit to facilitate absorption and reduce gas production and have an immunomodulatory effect through action on the lymphoid tissue associated with mucous membranes and play a role in production of immunoglobulin A (IgA) and local activation of macrophages. 2
The market for, and investments in, probiotics have been growing rapidly in recent years throughout the world. In 2015, the probiotic market was valued at US$ 33.19 billion, and it is projected that by 2020 investment will reach US$ 46.55 billion with an annual growth rate of 7%. 4
Not all probiotic products are the same, and their use must depend on quality, safety, tolerability, price and efficacy. Moreover, their use must take into account the economic limitations of Colombia’s health care system. 5 Currently, these microorganisms have been introduced into the market as nutritional supplements which have lower standards for approval than do registered medicines so they have lesser guarantees of quality, efficacy and safety. 6 This has led to the sale and promotion of multiple products containing probiotics many of which do not have acceptable evidence for use.
There are few studies that talk about the quality of probiotics. One study has evaluated sixteen products containing bifidobacteria to determine the true presence of the bacteria registered in the package using molecular techniques. The study found that only one product contained the bifidobacteria described on the label. 7 Other studies have found that the number of colonies reported cannot be isolated after cultivation. 8
In recent years, there have been numerous studies about the use of probiotics to treat diarrhea in children, so it is necessary to evaluate the available evidence to help clinical practice achieve efficacy and quality.
Methods
A review of evidence in the current literature about probiotic treatment of diarrhea in pediatrics was conducted using the following MeSH terms: probiotics, diarrhea or gastroenteritis, antibiotic-associated diarrhea and healthcare-associated diarrhea. A search for metaanalyses, systematic reviews and the most important clinical practice guidelines for children under 18 between 2007 and 2017 was also performed. Guidelines found include those of the European Society for Pediatric Gastroenterology Hepatology and Nutrition (ESPGHAN), Latin American Society of Gastroenterology, Hepatology and Pediatric Nutrition (LASPGHAN) and North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). Studies were classified into three categories: acute diarrhea, diarrhea associated with antibiotics and Clostridium difficile, and nosocomial diarrhea.
Acute diarrhea
The basis of treatment of acute diarrhea is early rehydration and early return to feeding plus zinc supplementation (due to the high prevalence of zinc deficiency in our country) as recommended by the Colombian guidelines. 9
In 2010, a Cochrane review analyzed 63 randomized or quasi-randomized studies that compared probiotics and placebos and which included 8,014 patients. Of these, 56 studies included 6,489 children. The results show that probiotics reduced the mean duration of diarrhea by 24.7 hours (95% confidence interval [CI]: 15.9 to 33.6 hours), and decreased the risk of diarrhea lasting for more than 4 days to 59%, (relative risk [RR]: 0.41, 95% CI: 0.32 to 0.53). 10 The organisms most frequently studied were Lactobacillus rhamnosus GG (13 studies), Saccharomyces boulardii (10 studies) and enterococcus LAB (lactic acid bacteria) (5 studies). No significant differences were found in the outcomes mentioned or in the doses used. 10
In 2013, a systematic review Applegate et al. evaluated the effect of probiotics in children under five years of age who had acute diarrhea. Infants and children taking antibiotics were excluded. We found eight studies that showed probiotics reduced the duration of diarrhea by 14% (95% CI: 3.8% to 24.2%) and reduced the frequency of diarrhea on the second day by 13.1% (CI 95 %: 0.8% to 25.3%). 11 No significant difference was found in hospital stays (RR: 0.81, 95% CI: 0.42 to1.57). Analyses of probiotic strains found that L. rhamnosus GG was the most consistent and reduced the duration of diarrhea by 16.0% (95% CI: -53.9 to 22.0%) with evidence of moderate quality. 11
Since the effect of probiotics depends on the species and strain used, probiotics have been studied individually. In 2007, a metaanalysis that evaluated S. boulardii treatment of acute diarrhea in children from two months to 12 years of age was published. It covered five studies with 619 participants. The results showed a reduction in the duration of diarrhea by 1.1 days (95% CI: -1.3 to -0.8 days), a reduction in the risk of diarrhea persisting to days three, six and seven of 29% (RR 0.71, 95% CI: 0.56 to 0.90), 51% (RR 0.49, 95% CI: 0.24 to 0.99) and 75% (RR: 0.25; 95% CI: 0.08 to 0.83), respectively. 12 One study reported a decrease in hospital stays of one day (95% CI: 1.4 to 0.62). 13
In 2013, a metaanalysis that evaluated L. rhamnosus GG treatment of acute gastroenteritis in children was published. It included 2,963 total participants, and eleven of the studies it covered, including 2,444 children, showed a reduction in the duration of diarrhea of 1.05 days (CI 95%: -1.7 to -0.4). A daily dose of 1010 colony forming units (CFU) of L. rhamnosus GG or more was more effective and decreased duration of diarrhea by 1.11 days (95% CI: -1.91 to -0.31), slightly more than did a daily dose of less than 1010 CFU which reduced duration by only of 0.9 days (95% CI: -2.5 to 0.69) 14. In addition, the risk of developing diarrhea for more than seven days was reduced by 73% (RR: 0.27, 95% CI: 0.09 to 0.78). Three of the studies including 201 patients also found that the use of L. rhamnosus GG effectively treated diarrhea caused by rotavirus. Duration of diarrhea fell by 2.05 days (95% CI: -2.39 to -1,71) with respect to one with invasive origin which did not show statistically significant improvement: 0.05 days (95% CI: 0.64 to 0.74). 14
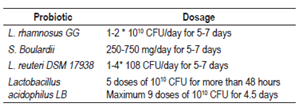
ESPGHAN established in 2014 that the use of probiotics should be considered for management of infectious diarrhea on the basis of findings in multiple metaanalyses. It established a strong recommendation for the use of L. rhamnosus GG and S. boulardii, but the GRADE quality of evidence level was low due to limitations in the consistency of the evidence and to high level of heterogeneity of the metaanalyses. 15 Lactobacillus reuteri has a weak recommendation for usage and a very low level of evidence. 15 The recommended doses are shown in Table 1.
In 2015, a Latin American consensus of pediatric gastroenterology reviewed the evidence of about 74 articles with recommendations for the use of probiotics in children. It established a 1A recommendation for the use of L. reuteri and a 1B recommendation for the use of L. rhamnosus GG and S. boulardii for treatment of infectious diarrhea. It did not specify recommended dosages. 16
For its part, the American Academy of Pediatrics also supports the use of probiotics to treat acute infectious diarrhea in healthy children, specifically L. rhamnosus GG to reduce the duration of diarrhea. 17
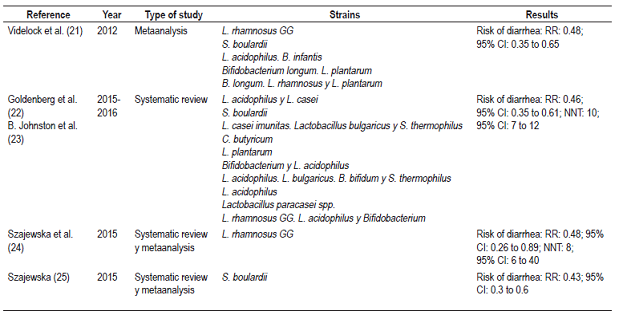
A worldwide review of clinical practice guidelines for the management of acute gastroenteritis in children has reported that nine of fifteen guidelines support the use of probiotics ant that ten of fifteen support the use of zinc sulfate. 18 Table 2 summarizes the findings of metaanalyses and systematic reviews regarding the use of probiotics to treat acute diarrhea.
Diarrhea associated with antibiotics and c. difficile
Diarrhea is one of the most common complications associated with the use of antibiotics in children. Antibiotics alter the biological balance of intestinal microbiota and can lead to the growth of pathogenic bacteria such as C. difficile bacilli. 19 It is estimated that its incidence is 11%. Children under two are the most commonly affected group with an incidence of up to 18%. β-lactam antibiotics are the most commonly associated antibiotics. 20
In 2012, Videlock and colleagues published a metaanalysis about the use of probiotics to treat diarrhea associated with antibiotics. It covered 10 pediatric studies and a population of 1,246 children. The results showed a 52% reduction of the risk of developing diarrhea associated with antibiotics when probiotics were used (RR: 0.48, 95% CI: 0.35 to 0.65) independent of the probiotic strain used and the type of antibiotic used. 21 Analysis of probiotic strains analysis included studies of adults. L. rhamnosus GG showed a risk reduction of 60% (RR: 0.40, 95% CI: 0.2 to 0.81) while S. boulardii reduced risk by 56% (RR: 0.46, 95% CI: 0.3 to 0.7). There was less heterogeneity with respect to L. rhamnosus GG. 21
In 2015, Goldenberg and colleagues published a Cochrane collaboration metaanalysis which was reviewed in 2016 in the Journal of the American Medical Association (JAMA). It analyzed 23 pediatric studies with a population of 3,938 participants for whom probiotics were used alone or in combination. The results found that the incidence of diarrhea associated with antibiotics in the group taking probiotics was 8% (163/1,992) while it was 19% (364/1,906) in the control group which did not receive probiotics. Overall risk reduction was 54% (RR: 0.46, 95% CI: 0.35 to 0.61) with a number needed to treat (NNT) of 10 patients to prevent an event (95% CI : 7 to 12). 22,23 GRADE analysis of evidence showed a moderate evidence quality, and no serious adverse events occurred. The probiotics with the best evidence were L. rhamnosus GG (four studies, n = 711) and S. boulardii (four studies, n = 1611) at doses of 5 to 40 CFU/day. 22,24
In 2015, a metaanalysis of five studies with 455 patients investigated the effectiveness of L. rhamnosus GG for prevention of diarrhea associated with antibiotics in adults and children. It found a reduction of risk by 52% but only in the pediatric population (RR: 0.48, 95% CI : 0.26 to 0.89). The GRADE quality of evidence was moderate, with an NNT to prevent an event of 8 patients (NNT: 8, 95% CI: 6 to 40). 25
A metaanalysis that evaluated studies of S. boulardii in six pediatric populations covering a total of 1,653 patients found that the risk of diarrhea associated with antibiotics in children receiving placebos was 20.9% while it was only 8.8% in children who received the probiotic: the reduction of risk was 57% (RR: 0.43, 95% CI: 0.3 to 0.6). 25 That metaanalysis also showed that in two studies with 579 patients, S. boulardii reduced the incidence of diarrhea associated with C. difficile by 75%, (RR: 0.25, 95% CI: 0.08 to 0.73). 23
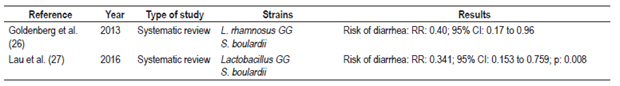
A 2013 systematic review by the Cochrane Collaboration of C. difficile infections found that administration of probiotics to pediatric patients reduced the risk of C. difficile infections by 60% (RR: 0.40, 95% CI: 0.17 to 0.96). The review covered three studies which included a total of 300 treated patients and 305 controls. The L. rhamnosus GG and S. boulardii strains were used in these studies. 26.
A 2016 metaanalysis that included four pediatric studies covering 938 patients found a statistically significant 66% reduction in the risk of C. difficile infection (RR: 0.341, 95% CI 0.153 to 0.759, p = 0.008). 27 Strains of L. rhamnosus GG and S. boulardii showed the best risk reductions of 6.7% and 58.5% respectively. The study of S. boulardii also included information about adult patients. 27
Based on these studies, ESPGHAN reviewed the data from more than 21 randomized clinical trials in 2016. The studies covered the 3255 patients included in these metaanalyses and found that the use of probiotics reduced the risk of diarrhea associated with antibiotics by 52% (RR: 0.48, 95% CI: 0.37 to 0.61) with an incidence of 21.2% compared to an incidence of 9.1% in patients who did not receive probiotics. 28
ESPGHAN reaffirmed that the probiotics with the best evidence are L. rhamnosus GG and S. boulardii, but concluded that dosage has not been clearly established. Nevertheless, it suggested that the greatest effect in children has been achieved with high doses of L. rhamnosus GG (1-2 x 1010 CFU). It strongly recommended its use for the prevention of diarrhea associated with antibiotics and graded the quality of the evidence as moderate. 28 It also concluded that there is no established dosage for S. boulardii but said that it should not be less than 250 mg nor more than 500 mg in children. Its recommendation was strong, and the quality of evidence was moderate. 28 In addition, on the basis of two studies with 579 patients which showed a 75% reduction in risk of C. difficile infections using S. boulardii, it recommended this probiotic but with low quality of evidence (RR: 0.25, 95% CI: 0.08 to 0.73). 29,30 Finally, it mentioned that B. clausii has no effect on the risk of diarrhea associated with antibiotics, nor does it have an effect when used in combinations of probiotics. 28 It recommended that the probiotic be administered simultaneously with the antibiotic and continued for the duration of antibiotic treatment.
For its part, the Latin American Consensus issued recommendation 1B for L. rhamnosus GG and S. boulardii for use in diarrhea associated with antibiotics. 16 Tables 3 and 4 summarize the findings of metaanalyses and systematic reviews of the use of probiotics to treat diarrhea associated with antibiotics and C. difficile.
Table 3 Metaanalyses and systematic reviews regarding use of probiotics to treat diarrhea associated with antibiotics

Nosocomial diarrhea
Nosocomial infections occur after the first 48 hours of hospital stay. In children, the most common infection associated with health care is rotavirus gastroenteritis. 31 A metaanalysis from 2012 showed that the incidence of rotavirus-associated diarrhea is 2.9 per 100 hospitalizations and that its epidemiological peak can reach as high as 8 per 100 hospitalizations. 32 In this field, the use of probiotics seems to be effective in prevention.
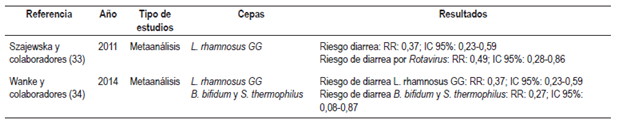
A metaanalysis of three studies that evaluated the effect of L. rhamnosus GG on diarrhea associated with health care was published in 2011. It found that taking this probiotic reduced the risk of diarrhea by 63% (RR: 0.37, 95% CI: 0.23 to 0.59) and symptomatic gastroenteritis due to rotavirus by 51% (RR 0.49, 95% CI: 0.28 to 0.86). However, no differences were found in the length of hospital stays. 33
A 2014 metaanalysis that collected data from six randomized clinical trials, including the three previously mentioned studies of the use of L. rhamnosus GG, covered 1,343 patients and confirmed the previously described reduction of the risk of diarrhea by 63 % (RR: 0.37, 95% CI: 0.23 to 0.59). In addition, one of the studies included showed that the combination of B. bifidum and S. thermophilus reduced the risk of diarrhea associated with health care by 78% (n = 55; RR: 0.27; 95%: 0.08 to 0.87) as well as reducing the risk of symptomatic gastroenteritis due to rotavirus (n = 55, RR: 0.27, 95% CI: 0.08 to 0.87). 34 In contrast, two other studies found that L. reuteri DSM 17938 and Lactobacillus delbrueckii H2B20 were not effective for reducing the incidence of nosocomial diarrhea. 34
A new study published in 2016 evaluated L. reuteri DSM 17938 in a population of 148 children. It found no difference in the risk of diarrhea associated with health care (RR: 1.19, 95% CI: 0.43 to 3.27). 35
Based on these studies, the Latin American Consensus issued a 1B recommendation for treatment with S. thermophilus, B. bifidum and L. rhamnosus GG for prevention of nosocomial diarrhea. 16 However, in June 2017, ESPGHAN’s working group on probiotics for treatment of nosocomial diarrhea published its recommendations, also based in part on a review of the two previously mentioned metaanalyses, and issued a strong recommendation of the use of L. rhamnosus GG with moderate evidence in favor 36. Due to the high quality evidence showing due to lack of efficacy of L. reuteri DSM 17938 for preventing nosocomial diarrhea, ESPGHAN recommends against its use. ESPGHAN did not issue recommendations for or against S. thermophilus, B. bifidum, L. delbrueckii H2B20 and Bifidobacterium animalis subsp. lactis (BB-12®) because there was insufficient evidence since only studies with two or more randomized clinical trials of probiotics were analyzed. 36
Table 5 summarizes the findings of metaanalyses and systematic reviews about the use of probiotics to treat nosocomial diarrhea.
Safety
Currently, there are no systematic reviews that analyze adverse effects and safety of probiotic administration, but evidence to date has demonstrated no serious adverse effects. 37 Nevertheless, cases of fungemia and bacteremia secondary to the administration of probiotics have been described in patients with risk factors such as immunosuppression, hospitalization in an intensive care unit (ICU) with a central catheter, and severe or cardiac structural disease. In these cases, the use of probiotics is not recommended. 38,39
Conclusion
Evidence shows that administration of probiotic strains L. rhamnosus GG and S. boulardii reduce duration of acute diarrhea by one day and also reduce the risk of prolongation of diarrhea to four and seven days. Administration of these probiotics is strongly recommended, but the quality of evidence remains low due to the heterogeneity of the studies. There is evidence that L. rhamnosus GG and S. boulardii reduce risk of diarrhea associated with antibiotics and c. difficile by 50% to 60% with an NNT of 10, moderate quality evidence, and a strong recommendation for use. Finally, there is evidence in favor of L. rhamnosus GG for reducing the risk of nosocomial diarrhea, especially symptomatic gastroenteritis due to rotavirus. There is insufficient evidence about S. thermophilus and B. bifidum. The use of Lactobacillus GG and S. boulardii should be considered in combination with standard treatment for management of diarrhea in children, remembering that its use should be individualized in each patient, weighing its costs and benefits.
REFERENCES
1. Hill C, Guarner F, Reid G, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506-14. https://doi.org/10.1038/nrgastro.2014.66. [ Links ]
2. Vandenplas Y, Huys G, Daube G. Probiotics: an update. J Pediatr (Rio J). 2015;91(1):6-21. https://doi.org/10.1016/j.jped.2014.08.005. [ Links ]
3. Weber TK, Polanco I. Gastrointestinal microbiota and some children diseases: a review. Gastroenterol Res Pract. 2012;2012:676585. [ Links ]
4. MarketsandMarkets.com. Probiotics market by application (functional food & beverages (dairy, non-dairy beverages, baked goods, meat, cereal), dietary supplements, animal feed), source (bacteria, yeast), form (dry, liquid), end user (human, animal), and region - forecast to 2022. Marketsandmarkets.com. [internet] 2017 [acceso el 25 de abril de 2017]. Disponible en: Disponible en: http://www.marketsandmarkets.com/Market-Reports/probiotic-market-advanced-technologies-and-global-market-69.html . [ Links ]
5. Grover S, Rashmi HM, Srivastava AK, et al. Probiotics for human health -new innovations and emerging trends. Gut Pathog. 2012;4(1):15. https://doi.org/10.1186/1757-4749-4-15. [ Links ]
6. Passariello A, Agricole P, Malfertheiner P. A critical appraisal of probiotics (as drugs or food supplements) in gastrointestinal diseases. Curr Med Res Opin. 2014;30(6):1055-64. https://doi.org/10.1185/03007995.2014.898138. [ Links ]
7. Lewis ZT, Shani G, Masarweh CF, et al. Validating bifidobacterial species and subspecies identity in commercial probiotic products. Pediatr Res. 2016;79(3):445-52. https://doi.org/10.1038/pr.2015.244. [ Links ]
8. Goldstein EJ, Citron DM, Claros MC, et al. Bacterial counts from five over-the-counter probiotics: are you getting what you paid for? Anaerobe. 2014;25:1-4. https://doi.org/10.1016/j.anaerobe.2013.10.005. [ Links ]
9. Ministerio de Salud y Protección Social, Colciencias, Instituto de Evaluación Tecnológica en Salud. Guía de referencia rápida para prevención, diagnóstico y tratamiento de la enfermedad diarreica aguda en niños menores de 5 años. Bogotá D. C.: MinSalud; 2013. [ Links ]
10. Allen SJ, Martinez EG, Gregorio GV, et al. Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst Rev. 2010;(11):CD003048. https://doi.org/10.1002/14651858.CD003048.pub3. [ Links ]
11. Applegate JA, Fischer Walker CL, Ambikapathi R, et al. Systematic review of probiotics for the treatment of community-acquired acute diarrhea in children. BMC Public Health. 2013;13 Suppl 3:S16. [ Links ]
12. Szajewska H, Skórka A, Dylag M. Meta-analysis: Saccharomyces boulardii for treating acute diarrhoea in children. Aliment Pharmacol Ther. 2007;25(3):257-64. https://doi.org/10.1111/j.1365-2036.2006.03202.x. [ Links ]
13. Kurugöl Z, Koturoğlu G. Effects of Saccharomyces boulardii in children with acute diarrhoea. Acta Paediatr. 2005;94(1):44-7. https://doi.org/10.1080/08035250410022521 - https://doi.org/10.1111/j.1651-2227.2005.tb01786.x. [ Links ]
14. Szajewska H, Skórka A, Ruszczyński M, et al. Meta-analysis: Lactobacillus GG for treating acute gastroenteritis in children--updated analysis of randomised controlled trials. Aliment Pharmacol Ther. 2013;38(5):467-76. https://doi.org/10.1111/apt.12403. [ Links ]
15. Szajewska H, Guarino A, Hojsak I, et al. Use of probiotics for management of acute gastroenteritis: a position paper by the ESPGHAN Working Group for Probiotics and Prebiotics. J Pediatr Gastroenterol Nutr. 2014;58(4):531-9. https://doi.org/10.1097/MPG.0000000000000320. [ Links ]
16. Cruchet S, Furnes R, Maruy A, et al. The use of probiotics in pediatric gastroenterology: a review of the literature and recommendations by Latin-American experts. Paediatr Drugs. 2015;17(3):199-216. https://doi.org/10.1007/s40272-015-0124-6. [ Links ]
17. Thomas DW, Greer FR; American Academy of Pediatrics Committee on Nutrition; et al. Probiotics and prebiotics in pediatrics. Pediatrics. 2010;126(6):1217-31. https://doi.org/10.1542/peds.2010-2548. [ Links ]
18. Lo Vecchio A, Dias JA, Berkley JA, et al. Comparison of recommendations in clinical practice guidelines for acute gastroenteritis in children. J Pediatr Gastroenterol Nutr. 2016;63(2):226-35. https://doi.org/10.1097/MPG.0000000000001133. [ Links ]
19. Guarino A, Guandalini S, Lo Vecchio A. Probiotics for prevention and treatment of diarrhea. J Clin Gastroenterol. 2015;49 Suppl 1:S37-45. https://doi.org/10.1097/MCG.0000000000000349. [ Links ]
20. Turck D, Bernet JP, Marx J, et al. Incidence and risk factors of oral antibiotic-associated diarrhea in an outpatient pediatric population. J Pediatr Gastroenterol Nutr. 2003;37(1):22-6. https://doi.org/10.1097/00005176-200307000-00004. [ Links ]
21. Videlock EJ, Cremonini F. Meta-analysis: probiotics in antibiotic-associated diarrhoea. Aliment Pharmacol Ther. 2012;35(12):1355-69. https://doi.org/10.1111/j.1365-2036.2012.05104.x. [ Links ]
22. Goldenberg JZ, Lytvyn L, Steurich J, et al. Probiotics for the prevention of pediatric antibiotic-associated diarrhea. Cochrane Database Syst Rev. 2015;(12):CD004827. https://doi.org/10.1002/14651858.CD004827.pub4. [ Links ]
23. Szajewska H, Kołodziej M. Systematic review with meta-analysis: Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea. Aliment Pharmacol Ther. 2015;42(7):793-801. https://doi.org/10.1111/apt.13344. [ Links ]
24. Johnston BC, Goldenberg JZ, Parkin PC. Probiotics and the prevention of antibiotic-associated diarrhea in infants and children. JAMA. 2016;316(14):1484-5. https://doi.org/10.1001/jama.2016.11838. [ Links ]
25. Szajewska H, Kołodziej M. Systematic review with meta-analysis: Lactobacillus rhamnosus GG in the prevention of antibiotic-associated diarrhoea in children and adults. Aliment Pharmacol Ther. 2015;42(10):1149-57. https://doi.org/10.1111/apt.13404. [ Links ]
26. Goldenberg JZ, Ma SS, Saxton JD, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. 2013;(5):CD006095. https://doi.org/10.1002/14651858.CD006095.pub3. [ Links ]
27. Lau CS, Chamberlain RS. Probiotics are effective at preventing Clostridium difficile-associated diarrhea: a systematic review and meta-analysis. Int J Gen Med. 2016;9:27-37. [ Links ]
28. Szajewska H, Canani RB, Guarino A, et al. Probiotics for the prevention of antibiotic-associated diarrhea in children. J Pediatr Gastroenterol Nutr. 2016;62(3):495-506. https://doi.org/10.1097/MPG.0000000000001081. [ Links ]
29. Kotowska M, Albrecht P, Szajewska H. Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea in children: a randomized double-blind placebo-controlled trial. Aliment Pharmacol Ther. 2005;21(5):583-90. https://doi.org/10.1111/j.1365-2036.2005.02356.x. [ Links ]
30. Shan LS, Hou P, Wang ZJ, et al. Prevention and treatment of diarrhoea with Saccharomyces boulardii in children with acute lower respiratory tract infections. Benef Microbes. 2013;4(4):329-34. https://doi.org/10.3920/BM2013.0008. [ Links ]
31. World Health Organization. Report on the burden of endemic health care-associated infection worldwide. Géneova: WHO; 2011. [ Links ]
32. Bruijning-Verhagen P, Quach C, Bonten M. Nosocomial rotavirus infections: a meta-analysis. Pediatrics. 2012;129(4):e1011-9. https://doi.org/10.1542/peds.2011-2779. [ Links ]
33. Szajewska H, Wanke M, Patro B. Meta-analysis: the effects of Lactobacillus rhamnosus GG supplementation for the prevention of healthcare-associated diarrhoea in children. Aliment Pharmacol Ther. 2011;34(9):1079-87. https://doi.org/10.1111/j.1365-2036.2011.04837.x. [ Links ]
34. Wanke M, Szajewska H. Probiotics for preventing healthcare-associated diarrhea in children: A meta-analysis of randomized controlled trials. Pediatr Pol. 2014;89(1):8-16. https://doi.org/10.1016/j.pepo.2013.12.003. [ Links ]
35. Urbańska M, Gieruszczak-Białek D, Szymański H, et al. Effectiveness of Lactobacillus reuteri DSM 17938 for the prevention of nosocomial diarrhea in children: a randomized, double-blind, placebo-controlled trial. Pediatr Infect Dis J. 2016;35(2):142-5. https://doi.org/10.1097/INF.0000000000000948. [ Links ]
36. Hojsak I, Szajewska H, Canani RB, et al. Probiotics for the prevention of nosocomial diarrhea in children. J Pediatr Gastroenterol Nutr. 2018;66(1):3-9. https://doi.org/10.1097/MPG.0000000000001637. [ Links ]
37. Hempel S, Newberry S, Ruelaz A, et al. Safety of probiotics used to reduce risk and prevent or treat disease. Evid Rep Technol Assess (Full Rep). 2011;(200):1-645. [ Links ]
38. Doron S, Snydman DR. Risk and safety of probiotics. Clin Infect Dis. 2015;60 Suppl 2:S129-34. https://doi.org/10.1093/cid/civ085. [ Links ]
39. Whelan K, Myers CE. Safety of probiotics in patients receiving nutritional support: a systematic review of case reports, randomized controlled trials, and nonrandomized trials. Am J Clin Nutr. 2010;91(3):687-703. https://doi.org/10.3945/ajcn.2009.28759. [ Links ]
Received: May 23, 2017; Accepted: January 22, 2018











 texto en
texto en