Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.1 Bogotá Jan./Mar. 2018
https://doi.org/10.22516/25007440.232
Case report
Endosonography with Fine Needle Aspiration Biopsy of the Left Adrenal Gland for Diagnosis of Paracoccidioidomycosis: Contribution of a New Case to the Literature
1Gastroenterólogo clínico quirúrgico, endosonografista de GASTROCAL, Fundación Oftalmológica de Santander (FOSCAL). Floridablanca, Santander, Colombia.
2Internista gastroenterólogo de GASTROCAL, FOSCAL. Floridablanca, Santander, Colombia.
3Cirujano gastrointestinal de FOSCAL. Floridablanca, Santander, Colombia
4, FOSCAL. Floridablanca, Santander, Colombia
5Internista endocrinólogo de FOSCAL. Floridablanca, Santander. Profesor asociado de la Universidad Autónoma de Bucaramanga (UNAB). Bucaramanga, Colombia
6Internista endocrinólogo de FOSCAL, FOSUNAB. Floridablanca, Santander, Colombia
Endosonography, born more than 30 years ago, is one diagnostic modality for benign and malignant pathologies of the gastrointestinal tract. In recent years, transgastric (left) or transduodenal (right) fine needle biopsies of the adrenal glands guided by endosonography has been demonstrated to be safer and more efficacious than percutaneous approaches guided by CT or ultrasound. Differential diagnoses of adrenal insufficiency with evidence of masses in adrenal glands must consider paracoccidioidomycosis despite the fact that it is exclusively present in Latin America where its etiological agent is found. We present a case of paracoccidioidomycosis with adrenal insufficiency and bilateral adrenal thickening whose diagnosis was achieved by transgastric biopsy of the left adrenal gland guided by endosonography.
Keywords: Endosonography; paracoccidioidomycosis; adrenal insufficiency
La endosonografía nació hace más de 30 años como parte de las modalidades diagnósticas de patologías benignas y malignas del tracto gastrointestinal. En los últimos años se ha demostrado la eficacia y seguridad superior de la biopsia con aguja fina de las glándulas suprarrenales por vía transgástrica (izquierda) o tranduodenal (derecha) guiadas por endosonografía, en comparación con los abordajes percutáneos guiados por tomografía axial computarizada (TAC) o ecografía. Uno de los diagnósticos diferenciales de insuficiencia suprarrenal con evidencia de masas en glándulas suprarrenales es la paracoccidioidomicosis, a pesar de ser una entidad de presentación exclusiva de las áreas geográficas de Latinoamérica, donde se encuentra su agente etiológico. Se presenta un caso de paciente con paracoccidioidomicosis con insuficiencia suprarrenal y engrosamiento adrenal bilateral, cuyo diagnóstico se logró mediante biopsia transgástrica de glándula suprarrenal izquierda guiada por endosonografía.
Palabras clave: Endosonografía; paracoccidioidomicosis; insuficiencia suprarrenal
Introduction
Endoscopic ultrasonography (EUS) or endosonography was born 30 years ago and has become one modality for diagnosing benign and malignant pathologies of the gastrointestinal tract. Currently, it is widely used for this purpose and has also been used with therapeutic intent for more than a decade. It offers several options including biliary-digestive tract derivations and combined approaches for the bile duct with rendez-vous technique. Most options are for the upper gastrointestinal tract. 1 EUS equipment makes it possible to take biopsy samples through transesophageal, transgastric, transduodenal or transrectal punctures. This allows for deeper and better studies. The possibility of obtaining tissue by means of fine needle aspiration (FNA) biopsies also allows differential diagnosis of multiple tumors and inflammatory pathologies. It often helps clarify a specific etiology and establish appropriate treatment. In recent years, the efficacy and safety of endoscopic ultrasound guided transgastric and transduodenal biopsies of the adrenal glands has been demonstrated to be superior to percutaneous approaches guided by computerized axial tomography (CT) or ultrasound.
Currently, it is known that adrenal masses are found incidentally in up to 5% of all patients who undergo a CT scan of the abdomen. Often, additional studies are required to clarify the final diagnosis. 2 Reports in the literature on EUS guided adrenal gland biopsies demonstrate the presence of metastatic malignant tumor lesions of lungs, breasts, the stomach, kidneys, skin and the lymphatic system as well as benign and infectious lesions (predominantly tuberculosis and histoplasmosis). It only became possible to diagnose paracoccidioidomycosis by biopsy of the left adrenal gland guided by EUS in recent years. 3,4 Since this is a new area, we decided to report this case of diagnosis of paracoccidioidomycosis through biopsy of the left adrenal gland guided by EUS.
Clinical case
The patient was a 56 year old man who came to the emergency department because of acute symptoms of generalized weakness, asthenia, adynamia and diaphoresis. Upon admission to the emergency department, severe hypotension and dehydration grade I were observed. A physical examination also showed hepatomegaly and skin lesions on the backs of his hands, and his face was hyperpigmented with regular edges. The patient is a farmer from Molagavita, a rural area in the Department of Santander in Colombia who currently resides in the urban area of Girón, Santander. His only pathological background consists of compensated diabetes. He had had symptoms of asthenia, adynamia for 8 months prior to his visit to the emergency department and had lost approximately 15 kg of weight: The severe acute episode began one month prior to coming to the hospital. He required hospitalization for correction of symptomatic hyponatremia.
Intravenous (IV) hydration was started immediately. At 8 A.M., the patient’s paraclinical study showed serum cortisol of 0.0 μg/dL, hyponatremia with serum sodium value of 125 mmol/L and severe hyperkalemia with serum potassium of 7 mmol/L (without electrocardiographic alterations). Other tests reported hyperphosphatemia of 5.9 mg/dL, uric acid at 8.57 mg/dL, and elevated serum creatinine values at 1.36 mg/dL. The data indicated that the patient was in adrenal crisis with deterioration of renal functioning and hyperphosphatemia with hyperuricemia. Hydrocortisone was started immediately while constant support of fluids and electrolytes was maintained. Hypotension, hyponatremia and hyperkalemia improved. A contrast-enhanced CT scan showed marked thickening of both suprarenal glands, especially the left, with homogeneous enhancement of the contrast medium but with a seemingly focal lesion on the left adrenal gland that measured 21 mm. Lymph nodes of the bilateral inguinal chains were also slightly enlarged (Figure 1).
The treating group requested an EUS to explore the possibility of taking a transgastric biopsy of the left adrenal lesion. Pancreatobiliary EUS performed with linear Pentax equipment and a Hitachi processor identified an enlarged left adrenal gland with a heterogeneous mass in the esophagogastric junction. It was predominantly hypoechoic without any apparent dominant lesion and measured 25 mm in diameter at its greatest dimension.

Figure 1 CT scan of the abdomen showing a diffuse increase in both adrenal glands, especially the left (white arrow).
An EUS guided biopsy was performed on the left adrenal mass using puncture needle number 22 G. Seven passes were made and then the stylet was removed in such a way that the appropriate material was obtained for study.
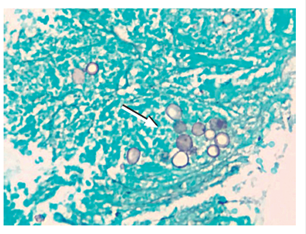
There were no complications related to the procedure (Figure 2). The histopathology report showed necrosis and inflammation. Grocott-Gomori’s (or Gömöri) methenamine silver stain showed aggregations of yeast blastoconidia of varying sizes that were compatible with paracoccidioidomycosis. Ziehl-Neelsen staining was negative for acid-fast bacilli, and no malignancy was observed in the sample (Figures 3 and 4). The patient was treated with amphotericin B until scheme completion and was discharged following evident clinical improvement. Patient continued to have outpatient follow-ups and treatment with itraconazole and oral prednisone.
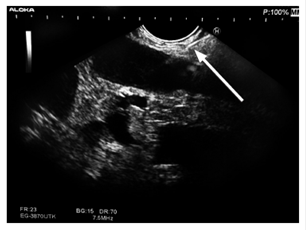
Figure 2 Heterogeneous, hypoechogenic EUS showing enlarged left adrenal gland with mass. EUS FNA of left adrenal gland (white arrow).
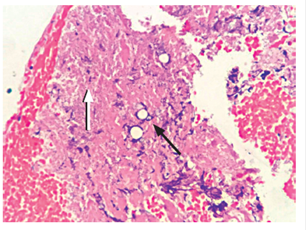
Figure 3 Hematoxylin-eosin staining shows necrotic tissue (white arrow) in the left adrenal gland and presence of yeast agglomerations (black arrow).
Discussion
Paracoccidioidomycosis is a systemic mycosis that is prevalent in Latin America and which is caused by Paracoccidioides brasiliensis, a dimorphic fungus. The lungs are most commonly affected, but the oral mucosa, mononuclear phagocyte system, skin, bones and adrenal glands can also be compromised. Two forms of clinical presentation are recognized: acute and subacute (juvenile type). The latter mainly affects children and is rapidly disseminated especially to the mononuclear phagocyte system. Chronic Paracoccidioidomycosis (adult type) accounts for more than 90% of all cases. It starts as a lung infection and then spreads to the regional lymph nodes. Depending on the immune response, it can be eliminated, remain dormant or become active. 5
The adrenal glands are affected in up to 40% of cases, but up to 10% of them have tissue damage that is so severe that the clinical manifestations of the disease appear as adrenal insufficiency. 3,5
A definitive diagnosis is made with microscopic identification of Langhans giant cells type and yeasts with multiple buds in an expanding ship’s wheel pattern with several smaller budding ship’s wheel in the periphery of a larger one. Periodic acid Schiff (PAS) and silver stains allow better visualization of this finding. 6
When paracoccidioidomycosis presents as adrenal failure and anatomical alteration of the adrenal glands, the diagnosis is achieved with a biopsy of those glands. 7
Historically, the biopsy methods of choice for adrenal glands were transabdominal ultrasound and CT with percutaneous puncture. However, these approaches fail to recover diagnostic samples up to 14% of the time and between 0.4% and 12% of the attempts are associated with adverse effects which include pneumothorax, bleeding, tumor dissemination in the puncture tract, adrenal abscesses and pancreatitis. 8
Currently, it is recognized that EUS achieves visualization of the left adrenal gland in up to 98% of studies and that left adrenal gland biopsies guided by EUS have a 100% technical success rate with very minimal numbers of mild complications such as minor bleeding. 9 Similarly, EUS guided fine needle puncture aspiration biopsies of adrenal glands are considered to provide better profiles than do percutaneous techniques, especially when it is taken into account that only the gastric wall is crossed to reach the site of sampling. It has even been shown by Puri et al. that when the percutaneous approach has failed to obtain adequate adrenal gland biopsy samples, the transgastric approach guided by EUS has been able to obtain adequate samples from which diagnoses have been achieved in all cases. 10
One important recommended is that the presence of a pheochromocytoma should be ruled out prior to and adrenal gland biopsy in order to prevent a hypertensive crisis from hemorrhaging at the biopsy site. 11
Conclusions
Paracoccidioidomycosis is a disease that is unique to a few Latin American countries where its causative pathogen is found. For this reason, case reports are limited to certain specific geographic areas. Similarly, the adrenal glands are not affected in all cases. Due to morphological alterations entailed in these glands, a differential diagnosis is required that can be achieved adequately with a biopsy. Over time, it has been shown that percutaneous biopsies of the adrenal glands carry a considerable risk profile of complications. Taken together with the excellent performance and safety of EUS-FNA, this explains why the technique has acquired such a fundamental role.
As the presentation of this case demonstrates, the possibility of differential diagnoses of adrenal gland lesions has been extended and should include possibility of paracoccidioidomycosis.
At present, there are no reports in the literature of paracoccidioidomycosis diagnosed in the adrenal gland by biopsy guided by EUS, so the case of this patient is of great importance for the scientific environment.
Referencias
1. Venkatachalapathy S, Nayar MK. Therapeutic endoscopic ultrasound. Frontline Gastroenterol. 2017;8(2):119-23. https://doi.org/10.1136/flgastro-2016-100774 [ Links ]
2. Bovio S, Cataldi A, Reimondo G, et al. Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J Endocrinol Invest. 2006;29(4):298-302. https://doi.org/10.1007/BF03344099 [ Links ]
3. Bodtger U, Vilmann P, Clementsen P, et al. Clinical impact of endoscopic ultrasound-fine needle aspiration of left adrenal masses in established or suspected lung cancer. J Thorac Oncol. 2009;4(12):1485-9. https://doi.org/10.1097/JTO.0b013e3181b9e848 [ Links ]
4. Colaiacovo R, Ganc RL, Leone AC, et al. Diagnosis of left adrenal paracoccidioidomycosis by endoscopic ultrasound fine needle aspiration. Endoscopy. 2011;43 Suppl 2 UCTN:E236-7. [ Links ]
5. Pereira CM, Silva SR, Camargo P, et al. Addison’s disease associated to paracocidioidomycosis. Braz J Oral Sci. 2004;3(9):475-8. [ Links ]
6. Farina M, Espinola C, Yamanaka W, et al. Paracocci-dioidomicosis en la glándula suprarenal. Reporte de un caso. Rev Chil Cir. 2007;59(4):299-301. https://doi.org/10.4067/S0718-40262007000400010 [ Links ]
7. Agudelo CA, Muñoz C, Ramírez A, et al. Identification of Paracoccidioides brasiliensis in adrenal glands biopsies of two patients with paracoccidioidomycosis and adrenal insufficiency. Rev Inst Med Trop Sao Paulo. 2009;51(1):45-8. https://doi.org/10.1590/S0036-46652009000100008. [ Links ]
8. DeWitt JM. Endoscopic ultrasound-guided fine-needle aspiration of right adrenal masses: report of 2 cases. J Ultrasound Med. 2008;27(2):261-7. https://doi.org/10.7863/jum.2008.27.2.261 [ Links ]
9. Patil R, Ona MA, Papafragkakis C, et al. Endoscopic ultrasound-guided fine-needle aspiration in the diagnosis of adrenal lesions. Ann Gastroenterol. 2016;29(3):307-11. https://doi.org/10.20524/aog.2016.0047 [ Links ]
10. Puri R, Thandassery RB, Choudhary NS, et al. Endoscopic ultrasound-guided fine-needle aspiration of the adrenal glands: analysis of 21 patients. Clin Endosc. 2015;48(2):165-70. https://doi.org/10.5946/ce.2015.48.2.165 [ Links ]
11. Casola G, Nicolet V, vanSonnenberg E, et al. Unsuspected pheochromocytoma: risk of blood-pressure alterations during percutaneous adrenal biopsy. Radiology. 1986;159(3):733-5. https://doi.org/10.1148/radiology.159.3.3517958 [ Links ]
Received: May 08, 2017; Accepted: January 22, 2018











 text in
text in