Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.1 Bogotá ene./mar. 2018
https://doi.org/10.22516/25007440.234
Case report
A Case Report of Cavernous Hemangioma as a Cause of Occult Gastrointestinal Bleeding
1 Especialista en gastroenterología y endoscopia digestiva, Clínica Farallones. Cali, Colombia
2 Especialista en patología, Clínica Farallones. Cali, Colombia
3 Residente de medicina interna, Universidad Libre. Cali, Colombia
4 Médico general, Clínica Farallones. Cali, Colombia
This is a descriptive study based on the case report of a patient suspected of occult gastrointestinal bleeding who was evaluated by the gastroenterology service in Clínica Nuestra in Cali. Previous studies had not shown cause of bleeding. Video endoscopy (Mirocam) found a lesion in the small intestine. Enteroscopy at performed at Clínica Farallones in Cali with an Olympus 180 Q enteroscope confirmed the finding. Surgery further confirmed the diagnosis. Data and photographs were obtained from the database of endoscopy services and the pathology photos were obtained from the pathologist’s registry. A literature review based on a Pubmed search of the existing literature on clinical histories and reports of similar cases is included.
Keywords: Cavernous hemangioma; occult gastrointestinal hemorrhage; endoscopic capsule
Se realizó un estudio descriptivo tipo reporte de caso de un paciente valorado por el servicio de gastroenterología en la Clínica Nuestra en la ciudad de Cali, por sospecha de sangrado digestivo oculto cuyos estudios previos no habían mostrado causa de sangrado. Se realizó videocápsula endoscópica (MiroCam®) con un hallazgo positivo de lesión en el intestino delgado. Se llevó a enteroscopia en Clínica Farallones de la Ciudad de Cali con enteroscopio Olympus 180 Q que confirmó el hallazgo. Ulteriormente, se llevó a cirugía, en la que se confirmó el diagnóstico. Los datos y las fotografías se obtuvieron en bases de datos de los servicios de endoscopia y las fotos de patología se obtuvieron del registro del médico patólogo. Finalmente, se realizó una búsqueda en PubMed sobre literatura existente de historia clínica y reportes de casos similares.
Palabras clave: Hemangioma cavernoso; hemorragia gastrointestinal oculta; cápsula endoscópica
Introduction
Gastrointestinal hemangiomas are benign primary tumors. Rare in all age groups, they represent 5% of all gastrointestinal tumors. 1 Classified as capillary, cavernous or mixed hemangiomas, cavernous hemangiomas occur most frequently. 2 They can appear as isolated phenomena or as part of systemic vascular disorders. 2
Among the possible forms of presentation are anemia, gastrointestinal bleeding (5% of digestive bleeding originates in the small intestine), intramural hematomas, perforation and intestinal obstruction. The latter is rare unless it is large and occludes the intestinal lumen. 3
Diagnosis of this lesion is difficult and generally requires several diagnostic tests including ones that are invasive. 4 Only 25% of these cases are diagnosed preoperatively. Traditionally, diagnosis has been based on angiography, nuclear gammagraphy with marked red blood cells, magnetic resonance imaging and enteroscopy. The latter, despite its high level of sensitivity, has the disadvantages that it generally only manages to explore about 80 to 120 cm from the angle of Treitz angle and that it is an invasive test that is annoying for the patient and has possible complications such as post-endoscopy abdominal pain, perforations and pancreatitis. 5
An endoscopic video capsule is the gold standard for identifying lesions of the small intestine. 6 It is significantly better for diagnosing intestinal vascular lesions than are all of the other techniques mentioned above. 7 With this you can obtain a low risk preoperative diagnosis without tests that cause bleeding. Other invasive tests are not effective in up to 75% of cases and repeated performance leads to greater costs. It should be noted that the benefit of the endoscopic capsule is related to the size of the lesion and to whether there is active bleeding at the time of exploration.
Surgical resection is the treatment of choice. Intestinal intussusception and perforations caused by cavernous hemangioma are extremely rare, 8 and postoperative recurrence is very rare. 9 In cases of non-resectable or diffuse hemangiomas, various treatments have been used with limited success. These include low-dose radiation therapy, cryotherapy and arterial embolization. 10
Case presentation
This patient is 67-year-old man who was admitted to the emergency department due to abdominal pain and rectal bleeding associated with constitutional symptoms of fatigue, asthenia and adynamia. Paraclinical tests included a complete blood count which showed low volume anemia. On the third day of hospitalization, a 1 g/dL decrease of hemoglobin was observed (Table 1), so two units of red blood cells were transfused. 2 A total colonoscopy followed by upper digestive endoscopy found no lesions that could explain the bleeding.
Table 1 Laboratory tests
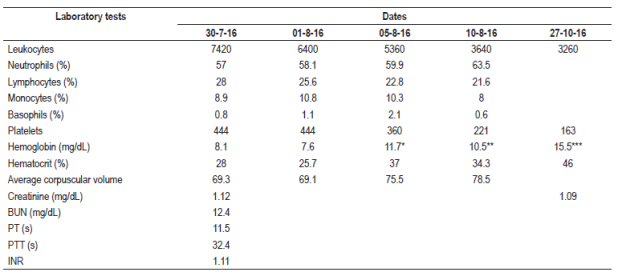
* Hemoglobin posttransfusion of blood products.
** Post-surgical hemoglobin.
*** Last control of hemoglobin.
BUN: blood urea nitrogen; INR: normalized international index; PT: prothrombin time; PTT: Partial thromboplastin time.
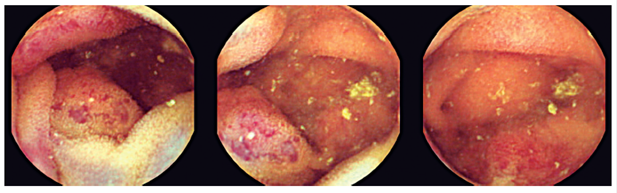
Taking into account that upper digestive endoscopy and total colonoscopy found no site of any bleeding, an endoscopic video capsule examination was performed. It found two violaceous lesions in the intestinal mucosa of the proximal jejunum which had no stigmas of bleeding. The initial diagnostic impression by endoscopic video capsule was either neuroendocrine tumors or Kaposi’s sarcoma (Figure 1).
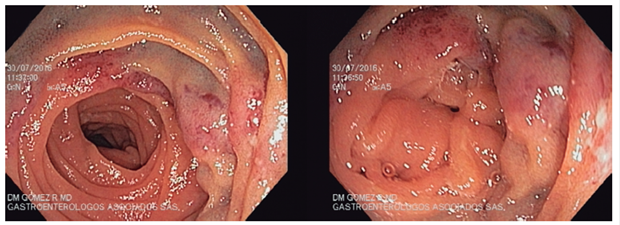
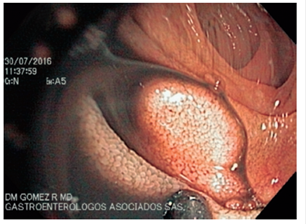
Subsequently, antegrade balloon enteroscopy was used to explore the middle jejunum. A discrete elevated, circular, hypervascularized lesion measuring approximately two cm between the proximal and middle jejunum hindered progression of the enteroscope. It was marked with Chinese ink with the help of an endoscopic needle above and below the lesion (Figures 2 and 3).
A laparoscopic proximal jejunal resection found a gastrointestinal tumor without other synchronous lesions.
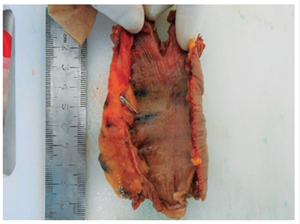
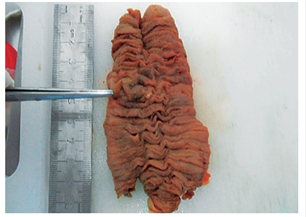
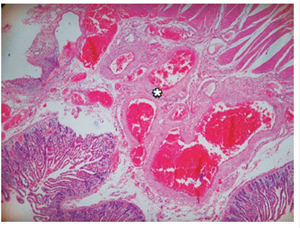
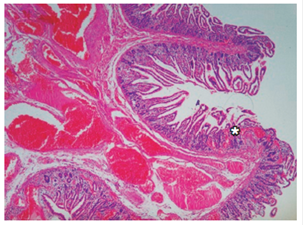
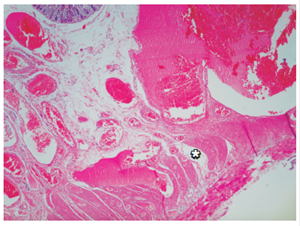
The macroscopic pathology description (Figures 4,5 and 6) revealed a segment of the small intestine that measured 11.5 cm long and was up to 3.5 cm in diameter and whose corresponding mesentery was without orientation. The mucosa was everted, and both ends were open. The serosa was smooth and marked with Chinese ink in the middle third. The mucosa showed a lesion in the form of a plaque with flattened violaceous folds. It measured 2.4 x 2.2 cm and contained cut microcysts filled with blood. The lesion was located 4 cm from the nearest edge and 5.2 cm from the opposite edge. The folds of rest of the intestinal mucosa appeared to be normal, and no other lesions were found. The serosa ink markings coincided with the submucosal lesion. The mesentery showed areas of congestion, but no lymph nodes were found. The microscopic slides of the wall of the small intestine (Figures 7,8,9 and 10) showed atypia with a proliferative lesion formed by large cavernous vascular channels with thin fibromuscular walls covered by the endothelium and filled with blood. This lesion was located primarily in the submucosa but extended focally to the lamina propria and to the internal muscle. The diagnosis was compatible with cavernous hemangioma.
Currently, the patient is stable and has had no new episodes of bleeding or anemia (Table 1). He continues to have follow/up examinations in the gastroenterology department.
Discussion
Gastrointestinal hemangiomas are unusual benign tumors whose first sign is usually bleeding. Although they are uncommon causes of gastrointestinal bleeding, s small bowel hemangioma can often lead to acute hemorrhaging or chronic anemia, and clinical manifestations of melena are observed in 65% of cases. They occur most frequently in the jejunum (46%), although they can compromise the entire gastrointestinal tract and manifest as intramural or intraluminal masses. In the colon, they are most common in the rectosigmoid section and may have the atypical appearance of a rigid annular lesion that mimics a carcinoma. They are equally common among men and women, and the average age of patients at presentation is 34.6 years. 1,11
The case described here compares well with clinical presentations in patients with a diagnosis of cavernous hemangioma found in current literature. The clinical picture was characterized by chronic anemia, weight loss, constitutional symptoms and digestive bleeding that led to initiation of the imaging protocol. 12 Upper digestive endoscopy and total colonoscopy failed to reveal any findings compatible with the origin of bleeding, indicating one important reason that this entity should be considered in cases of occult digestive bleeding.
The age of presentation of 67 years of the patient described here is unusual. The average age of presentation established in other reports is 34.6 years. This is another point to take into account when thinking about etiological alternatives in cases of occult digestive bleeding.
This description supports the use of an endoscopic video capsule as the gold standard for hidden digestive bleeding. The anatomic presentation site documented by endoscopic capsule is compatible with those described in the literature where 46% of the cases compromised the jejunum. The endoscopic capsule is clearly useful for preoperative diagnosis of hemangiomas in the small intestine.
Finally, this case shows how the endoscopic capsule has revolutionized diagnostic evaluation of small bowel lesions. Before this procedure became available, vascular lesions such as cavernous hemangioma required multiple investigations some of which were invasive and which resulted in uncertain diagnoses and associated morbidity and mortality.
Referencias
1. de Mascarenhas-Saraiva MN, da Silva Araújo Lopes LM. Small-bowel tumors diagnosed by wireless capsule endoscopy: report of five cases. Endoscopy. 2003;35(10):865-8. https://doi.org/10.1055/s-2003-42625. [ Links ]
2. Camilleri M, Chadwick VS, Hodgson HJ. Vascular anomalies of the gastrointestinal tract. Hepatogastroenterology. 1984;31(3):149-53. [ Links ]
3. Ell C, Remke S, May A, Helou L, Henrich R, Mayer G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy. 2002;34(9):685-9. https://doi.org/10.1055/s-2002-33446. [ Links ]
4. Kuo LW, Chuang HW, Chen YC. Small bowel cavernous hemangioma complicated with intussusception: report of an extremely rare case and review of literature. Indian J Surg. 2015;77(Suppl 1):123-4. https://doi.org/10.1007/s12262-014-1194-3. [ Links ]
5. Akamatsu T, Matsuda Y, Tsugane E, et al. A case of multiple cavernous hemangioma of the small intestine and clinical review of the Japanese literature. Gastroenterol Jpn. 1990;25(4):494-8. [ Links ]
6. Appleyard M, Fireman Z, Glukhovsky A, et al. A randomized trial comparing wireless capsule endoscopy with push enteroscopy for the detection of small-bowel lesions. Gastroenterology. 2000;119(6):1431-8. https://doi.org/10.1053/gast.2000.20844. [ Links ]
7. Pera M, Márquez L, Dedeu JM, et al. Solitary cavernous hemangioma of the small intestine as the cause of long-standing iron deficiency anemia. J Gastrointest Surg. 2012;16(12):2288-90. https://doi.org/10.1007/s11605-012-1991-6. [ Links ]
8. Pennazio M. Small-intestinal pathology on capsule endoscopy: spectrum of vascular lesions. Endoscopy. 2005 Sep;37(9):864-9. Erratum in: Endoscopy. 2005;37(10):1029. https://doi.org/10.1055/s-2005-870212. [ Links ]
9. Donhauser JL, Kelly EC. Intussusception in the adult. Am J Surg. 1950;79(5):673-7. https://doi.org/10.1016/0002-9610(50)90333-3. [ Links ]
10. Ruiz AR Jr, Ginsberg AL. Giant mesenteric hemangioma with small intestinal involvement: an unusual cause of recurrent gastrointestinal bleed and review of gastrointestinal hemangiomas. Dig Dis Sci. 1999;44(12):2545-51. https://doi.org/10.1023/A:1026659710815. [ Links ]
11. Allred HW Jr. Hemangiomas of the colon, rectum, and anus. Mayo Clin Proc. 1974;49(10):739-41. [ Links ]
12. Levy AD, Abbott RM, Rohrmann CA Jr, Frazier AA, Kende A. Gastrointestinal hemangiomas: imaging findings with pathologic correlation in pediatric and adult patients. AJR Am J Roentgenol. 2001;177(5):1073-81. https://doi.org/10.2214/ajr.177.5.1771073. [ Links ]
Received: May 18, 2017; Accepted: January 22, 2018











 texto en
texto en