Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.1 Bogotá Jan./Mar. 2018
https://doi.org/10.22516/25007440.235
Case report
Case Report of Rescue Therapy for Bile Duct Perforation using Fully Covered Self-Expanding Metal Stent after Failure of Conservative Management
1Gastroenterólogo de la Universidad Autónoma de Bucaramanga (UNAB) y Fundación Oftalmológica de Santander (FOSCAL). Floridablanca, Santander, Colombia. Correo: germantofi@hotmail.com
2Cirujano gastrointestinal, departamento de cirugía gastrointestinal de la FOSCAL. Floridablanca, Santander, Colombia. Correo: Jairoemendoza.saavedra@hotmail.com
3Médico internista, departamento de medicina interna de la FOSCAL. Floridablanca, Santander, Colombia. Correo: carlos.velandia@gmail.com
4Médico general de la FOSCAL. Floridablanca, Santander, Colombia.
Complications occur in 5% to 10% of patients who undergo endoscopic retrograde cholangiopancreatography (ERCP), but less than 1% suffer perforations. The use of fully covered self-expanding metal stents (SEMS) to close uncomplicated perforations has become a safe optional strategy for initial management of these patients, as well as for rescue therapy when conservative management has failed.
We present the case of a 73-year-old patient with residual choledocholithiasis who underwent therapeutic ERCP with sphincterotomy and stone removal. Twelve hours after the intervention, the patient returned to the emergency department where a biliary tract type II perforation secondary to sphincterotomy was confirmed. Subsequent conservative management included suspension of oral feeding, administration of proton pump inhibitors and antibiotics, surgical evaluation and medical observation. Failure of non-surgical management led to consideration of placement of a fully covered SEMS as rescue therapy. The patient’s postoperative evolution was with satisfactory, and she was discharged eight days after stent placement.
Keywords: Biliary tract; intestinal perforation; endoscopic retrograde cholangiopancreatography; postoperative
Las complicaciones de la colangiopancreatografía retrógrada endoscópica (CPRE) ocurren entre el 5% y 10% de los pacientes, de los cuales menos del 1% sufre perforaciones. El uso de stents metálicos autoexpandibles totalmente cubiertos para el cierre de perforaciones no complicadas se ha convertido en una estrategia opcional y segura para el manejo inicial de estos pacientes, así como una terapia de rescate para quienes el manejo conservativo ha fallado.
Presentamos el caso de una paciente de 73 años con coledocolitiasis residual que fue sometida a una CPRE terapéutica con esfinterotomía y remoción de los cálculos. 12 horas después de la intervención, consultó al servicio de urgencias donde se confirmó una perforación de la vía biliar tipo II secundaria a esfinterotomía. Ulteriormente, se ofreció un manejo conservador con retiro de la ingesta oral, terapia con inhibidor de la bomba de protones, antibióticos, evaluación quirúrgica y observación médica. Sin embargo, ante la falla del manejo no quirúrgico, se consideró la colocación del stent metálico autoexpandible totalmente cubierto como terapia de rescate con evolución satisfactoria en el postoperatorio y salida 8 días después de la colocación del stent.
Palabras clave: Vía biliar; perforación intestinal; colangiopancreatografía retrógrada endoscópica, postoperatorio
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP), introduced in 1968, has become a commonly used procedure for diagnosis and management of diseases of the pancreatic and common bile ducts. 1 Initially, interventions were restricted to the use of small-diameter plastic stents, due to the small diameters of these ducts, but since 1982, the development of a larger duodenoscope biopsy channels and new endoscopic techniques have made interventions with larger stents possible. 2 This has resulted in decreasing numbers of associated complications such as post-ERCP bleeding. 3,4
ERCP complication rates reported in the literature vary widely: pancreatitis is most frequent (5% -10%), followed by hemorrhaging (1% -2%) and infections (1% -2%). 5 Most only require conservative management and medical observation and have morbidity rates of 5% to 10% and mortality rates from 0.1% to 1%. 6,7 Nevertheless, although the incidence of post-ERCP perforations is only 0.5% to 0.6%, 5 the mortality rate in these cases is 7% to 14%. It depends upon several factors including early detection and rapid management. 6,8
During endoscopy, instruments can cause perforations at any point including the esophagus, stomach, and duodenum. For ERCP, these regions include the biliary tract and the area around the ampulla of Vater associated with sphincterotomy. 9 Risk factors for post-ERCP perforation are related to procedures such as sphincterotomy, intramural injections, dilatation of stenosis, manipulation of the guidewire, prolonged procedures and difficulties during the examination. 10 They can also be related to patient characteristics such as anatomy distorted by surgery (e.g., Billroth II) which confers a significant risk of perforation especially at the site of the anastomosis or the efferent stump. 9
According to Stapfer et al., post-ERCP duodenal perforations are classified according to the degree of severity, anatomical location, perforation mechanism and implications for management into four types (Table 1). 11 A 2015systematic review by Vezakis et al. has analyzed 18 studies published between 2000 and 2014. They included 142,847 patients and found an incidence of duodenal perforations of 0.39%. According to the Stapfer classification, type I perforations accounted for 25%, type II accounted for 46%, and type III accounted for 22%. The overall mortality rate was 7.8%. 12 Management of each type of post-ERCP duodenal perforations can be summarized into two categories: conservative (types II, III and IV) and surgical (types I and II). 11 The choice of therapeutic approach for type II perforations depends on clinical history, physical examination and findings from computed tomography (CT) or magnetic resonance imaging. 7,10,11 After a careful selection of patients, non-surgical treatment has been successful in 90% of cases. 13. Debates continue about how to decide which nonsurgical management method is best for a particular patient and what to do when initial treatment fails (especially for type II perforations due to their high mortality rates). 12 According to another systematic review by Cirocchi et al. that covered 303 patients, the most frequent type of perforation according to the Stapfer classification was type II. It accounted for 54% of cases of which 84.2% only required conservative management. 14
Table 1 Classification of post-ERCP duodenal perforations 11
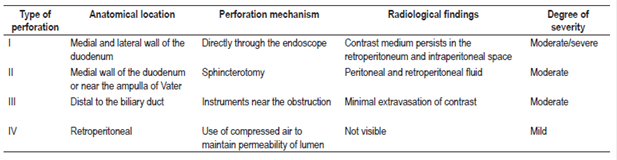
Modified from: Stapfer M et al. Ann Surg. 2000; 232 (2): 191-8.
The systematic review conducted by Vezakis et al. also analyzed 11 studies about diagnosis and treatment of post-ERCP perforations. The overall mortality rate was 9.4%. Twenty one percent of patients required surgical management, the mortality rate for this group of patients was 38%. 12
Based on clinical series, experts recommend conservative management using a nasal-duodenal or nasogastric drainage tube, intravenous fluids, antibiotics, and - in some cases - somatostatin analogues. Nevertheless, there are not yet any certain recommendations regarding aggressive treatment through stent placement given concerns about the final result and the potential need for repeat intervention (which is an individual decision for each patient). 13
Clinical case
The patient was a 73-year-old woman who had had laparoscopic cholecystectomy due to cholelithiasis. Because of clinical symptoms of obstruction of the bile duct due to residual choledocholithiasis with secondary dilatation of the extrahepatic bile duct she underwent therapeutic ERCP with sphincterotomy of the major papilla and extraction of several gallstones without bleeding during the procedure. Twelve hours later she was admitted to the emergency department because of severe pain in the right upper quadrant that radiated to the right shoulder and was associated with four episodes of vomiting without signs of bleeding. Physical examination showed a heart rate of 75 beats per minute (bpm) with moderate pain on palpation of the right upper quadrant but without peritoneal irritation. Laboratory tests showed a leukocyte count of 11,830/mm3 and a granulocyte percentage of 91%. Based on these findings, conservative management consisting of a proton pump inhibitor and intravenous antibiotics. An abdominal CT scan showed aerobilia and free fluid in the peritoneum that extended from the lower edge of the liver to the space anterior to the right kidney (Figure 1).
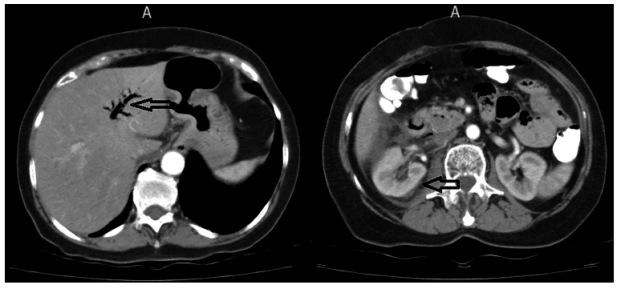
Figure 1 Contrast CT scan of abdomen showing aerobilia in the left panel. In the right panel there was evidence of free fluid in the peritoneum, liver and right anterior perirenal space (black arrows).
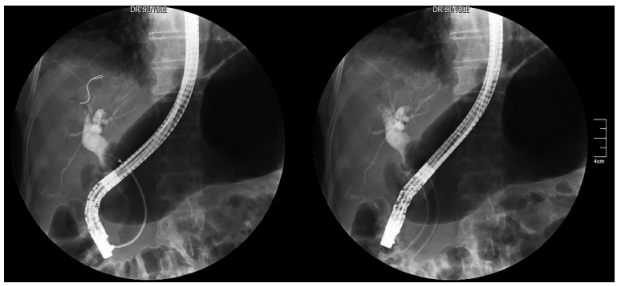
A doctor from the gastrointestinal surgery department suspected post-ERCP type II duodenal perforation and decided to continue conservative management. Forty-eight hours later, the patient developed tachycardia, persistent localized abdominal pain and had a white blood cell count of 14,110/mm3 with a neutrophil percentage of 89%, without peritoneal irritation. For these reasons, the gastrointestinal surgeon decided to perform an ERCP which confirmed type II perforation. This led to the decision to place a fully covered self-expanding metal stent (FCSEMS) to close the perforation due to failure of conventional medical therapy (Figure 2). After the intervention, the clinical evolution of the patient was satisfactory with absence of abdominal pain, normalization of the leukocyte count and an abdominal CT that showed no evidence of leakage of contrast material to the retroperitoneum 24 hours after the procedure.
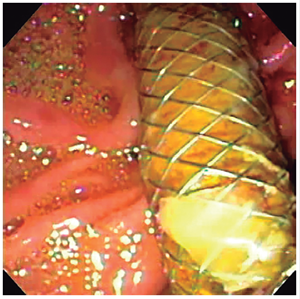
Eight days after FCSEMS placement and completion of the antibiotic treatment, the patient was discharged in adequate clinical condition. Eight weeks after the procedure, the stent was removed on an outpatient basis without complications (Figure 3).
Conclusions
This report describes an uncomplicated post-ERCP type II perforation which required placement of a FCSEMS in the bile duct as salvage therapy after conservative management had failed. There is still no consensus in the management guidelines regarding these complications because retroperitoneal perforations related to endoscopy are rare and because there is great variability in clinical consequences. 15
Maintaining conservative treatment is the mainstay in most cases, even when there is ample presence of retroperitoneal air in asymptomatic patients. 10,13 If internal or external perforation of the bile duct is confirmed, pancreatic drainage may be indicated. 16 Contraindications to a non-surgical approach are abdominal pain with signs of peritoneal irritation, fever, clinical signs of toxicity, greater filtration of contrast medium, fluid collections and unresolved problems. These should be resolved with surgery at the same time that drainage of the lesion is repaired. This is especially true for patients who are older adults. 10,13
On one hand, the advent of new endoscopic techniques including minimally invasive interventions with FCSEMS and endoclips have been reported to have had successful results for patients with type I perforations. 17,18. On the other hand, Howard et al. have reported an innovative and aggressive approach for type II perforations: immediate endoscopic drainage derived from the bile duct, pancreatic duct or duodenum (whichever is proximal to the lesion) using a biliary stent or a nasal-biliary tube with continuous drainage of bile fluid using a nasogastric or nasal-duodenal tube. 16,19 This has decreased the need for interventions from 60% to 10%. 19 Nevertheless, inadequate biliary drainage can cause infiltration of bile fluid which can drain to the site of the perforation and increase morbidity. 11
A need for new, safe and effective interventions for managing post-ERCP perforation complications led to the use of FCSEMS in 2011. 15 While FCSEMS are currently used to treat other benign and neoplastic clinical conditions of the bile duct, 20,21 their use in type II perforations is still not widely understood and discussed because there are only a few case reports albeit with excellent results. 15,18,20 A concern about FCSEMS’ safety is based on reports of complications including duodenal migration, bile duct ulcers, de novo choledocholithiasis, stenosis, and even periampullary adenomas. 21,22 Evidence suggests that FCSEMS placement for 30 days or less is effective in resolving complex bile leaks and post-sphincterotomy bleeding. The duration of the stent placement varies according to the patient’s clinical condition, but the strategy of temporary stenting is associated with lower risks of early and late complications. 20
Although complications secondary to ERCP are rare, they are a marker for high risk of mortality. 22 They require early diagnoses and precise, safe and effective multidisciplinary treatment. This case shows the need for a well-guided assessment of the initial approach for patients with non-surgical post-ERCP type II perforations. It furthermore shows that patients for who do not meet surgical criteria but for whom conservative treatment has failed failure, can be successfully treated with the innovative and minimally invasive strategy of using FCSEMS for safe closure of lesions. This case demonstrates that successful outcomes are possible for specific patients with subsequent FCSEMS removal.
Consent. Written informed consent of the patient was obtained for the publication of this case report and the images that accompany it. A copy of the written consent is available for review by the editor of this journal.
Conflict of interests. The authors declare that they have no conflicts of political, personal, religious, ideological, academic, intellectual, commercial or any other interest.
Acknowledgments
We thank the Department of Radiology that provided radiology services on behalf of FOSCAL.
REFERENCES
1. McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968;167(5):752-6. https://doi.org/10.1097/00000658-196805000-00013 [ Links ]
2. Huibregtse K, Tytgat GN. Palliative treatment of obstructive jaundice by transpapillary introduction of large bore bile duct endoprosthesis. Gut. 1982;23(5):371-5. https://doi.org/10.1136/gut.23.5.371 [ Links ]
3. Ferreira LE, Baron TH. Post-sphincterotomy bleeding: who, what, when, and how. Am J Gastroenterol. 2007;102(12):2850-8. https://doi.org/10.1111/j.1572-0241.2007.01563.x [ Links ]
4. Valats JC, Funakoshi N, Bauret P, et al. Covered self-expandable biliary stents for the treatment of bleeding after ERCP. Gastrointest Endosc. 2013;78(1):183-7. https://doi.org/10.1016/j.gie.2013.02.035 [ Links ]
5. Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48(1):1-10. https://doi.org/10.1016/S0016-5107(98)70121-X [ Links ]
6. Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335(13):909-18. DOI: 10.1056/NEJM199609263351301. [ Links ]
7. Enns R, Eloubeidi MA, Mergener K, et al. ERCP-related perforations: risk factors and management. Endoscopy. 2002;34(4):293-8. https://doi.org/10.1055/s-2002-23650 [ Links ]
8. Fatima J, Baron TH, Topazian MD, et al. Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management. Arch Surg. 2007;142(5):448-54. https://doi.org/10.1001/archsurg.142.5.448 [ Links ]
9. Guda NM, Reddy DN, Kumar A. Complications of ERCP. Indian J Gastroenterol. 2014;33(1):1-9. https://doi.org/10.1007/s12664-013-0383-5 [ Links ]
10. Lee TH, Han JH, Park SH. Endoscopic treatments of endoscopic retrograde cholangiopancreatography-related duodenal perforations. Clin Endosc. 2013;46(5):522-8. https://doi.org/10.5946/ce.2013.46.5.522 [ Links ]
11. Stapfer M, Selby RR, Stain SC, et al. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000;232(2):191-8. https://doi.org/10.1097/00000658-200008000-00007 [ Links ]
12. Vezakis A, Fragulidis G, Polydorou A. Endoscopic retrograde cholangiopancreatography-related perforations: Diagnosis and management. World J Gastrointest Endosc. 2015;7(14):1135-41. https://doi.org/10.4253/wjge.v7.i14.1135 [ Links ]
13. Paspatis GA, Dumonceau JM, Barthet M, et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2014;46(8):693-711. https://doi.org/10.1055/s-0034-1377531 [ Links ]
14. Cirocchi R, Kelly MD, Griffiths EA, et al. A systematic review of the management and outcome of ERCP related duodenal perforations using a standardized classification system. Surgeon. 2017;15(6):379-87. https://doi.org/10.1016/j.surge.2017.05.004 [ Links ]
15. Vezakis A, Fragulidis G, Nastos C, et al. Closure of a persistent sphincterotomy-related duodenal perforation by placement of a covered self-expandable metallic biliary stent. World J Gastroenterol. 2011;17(40):4539-41. https://doi.org/10.3748/wjg.v17.i40.4539 [ Links ]
16. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37(3):383-93. https://doi.org/10.1016/S0016-5107(91)70740-2 [ Links ]
17. Small AJ, Petersen BT, Baron TH. Closure of a duodenal stent-induced perforation by endoscopic stent removal and covered self-expandable metal stent placement (with video). Gastrointest Endosc. 2007;66(5):1063-5. https://doi.org/10.1016/j.gie.2007.03.1082 [ Links ]
18. Baron TH, Wong Kee Song LM, Zielinski MD, et al. A comprehensive approach to the management of acute endoscopic perforations (with videos). Gastrointest Endosc. 2012;76(4):838-59. https://doi.org/10.1016/j.gie.2012.04.476 [ Links ]
19. Thomas J. Howard. Letters To The Editor. Ann Surg. 2001;234(1):132-3. [ Links ]
20. Canena J, Liberato M, Horta D, et al. Short-term stenting using fully covered self-expandable metal stents for treatment of refractory biliary leaks, postsphincterotomy bleeding, and perforations. Surg Endosc. 2013;27(1):313-24. https://doi.org/10.1007/s00464-012-2368-3 [ Links ]
21. Kahaleh M, Behm B, Clarke BW, et al. Temporary placement of covered self-expandable metal stents in benign biliary strictures: a new paradigm? (with video). Gastrointest Endosc. 2008;67(3):446-54. https://doi.org/10.1016/j.gie.2007.06.057 [ Links ]
22. Sandha GS, Bourke MJ, Haber GB, et al. Endoscopic therapy for bile leak based on a new classification: results in 207 patients. Gastrointest Endosc. 2004;60(4):567-74. https://doi.org/10.1016/S0016-5107(04)01892-9 [ Links ]
Received: July 04, 2017; Accepted: January 22, 2018











 text in
text in