Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.2 Bogotá Apr./June 2018
https://doi.org/10.22516/25007440.257
Case report
A case of refractory anastomotic esophageal stenosis managed with a radial incision and endoscopic cutting
1Especialista en Gastroenterología, jefe de la especialidad de Gastroenterología Clínico-Quirúrgica de la Universidad de Caldas, jefe y coordinador de Unión de Cirujanos de Manizales. Manizales, Colombia
2Especialista en Gastroenterología Clínico-Quirúrgica, Universidad de Caldas. Manizales, Colombia
3Residente fellow de segundo año de Gastroenterología Clínico-Quirúrgica, Universidad de Caldas. Manizales, Colombia
Esophageal stenoses very rarely occur after an esophagojejunal anastomosis, but when they do they can compromise patients’ quality of life and nutritional status and may require endoscopic management with balloon dilation or with plugs which entail risks. Nevertheless, there is a group of patients who do not improve after dilation, whose stenoses persist, and who therefore continue to be symptomatic. For a patient with a stenosis that is refractory to dilation, a radial incision and endoscopic cutting with an electric scalpel can be performed with good results. We present the case of a patient with a postoperative stenosis at the esophagojejunal anastomosis who was refractory to initial dilation, who required a radial incision cut with an endoscopic electric scalpel whose improvement led to a better quality of life.
Keywords: Endoscopy; dilatation; stenosis; radial incision
Una causa poco frecuente de estenosis esofágica es la que se presenta después de una anastomosis esofagoyeyunal, la cual puede llevar a comprometer la calidad de vida del paciente y su estado nutricional, que requiere un manejo endoscópico inicial con balón de dilatación o con bujías (con el riesgo que ellas generan); pero hay un grupo de pacientes quienes, a pesar de la dilatación, no encuentran mejoría, por lo que persisten con la estenosis y, por tanto, con su sintomatología. En este último tipo de pacientes con estenosis refractarias al manejo con dilatación se realiza la técnica de incisión radiada y corte endoscópico con electrobisturí de punta, con buenos resultados. Se presenta el caso de un paciente con una estenosis postoperatoria a nivel de la anastomosis esofagoyeyunal, a quien se le dio un manejo inicial con dilatación refractaria y requirió una incisión radiada y corte endoscópico con electrobisturí de punta, y obtuvo mejores resultados en su calidad de vida.
Palabras clave: Endoscopia; dilatación; estenosis; incisión radiada
Introduction
Eighty percent of benign esophageal strictures occur after gastroesophageal reflux. The remaining 20% have causes such as postoperative stenosis, Schatzki’s ring, burns due to caustics and radiation. When an anastomosis is surgically created using either manual or mechanical sutures, there is an inherent risk fibrosis and stenosis at the site of the anastomosis which must be managed with pneumatic balloon dilation. This technique achieves satisfactory results in a good percentage of patients but has recurrence rates that sometimes require multiple dilation sessions. For patients with postsurgical stenoses that are refractory to dilation and whose stenotic segment is short (<1 cm), management with a radial endoscopic incision and resection has good results.
Clinical case
The patient was a 49-year-old man who had had a total gastrectomy with Roux-en-Y reconstruction three years earlier. Two months following surgery, he presented dysphagia. A postoperative stenosis was found and initially treated with outpatient esophageal dilation which partially relieved his symptoms. Nevertheless, some dysphagia continued for solids (grade 2). Relief lasted less than 3 months.
Esophageal balloon dilation was again performed in December 2013 and in November 2014. This was followed by a very short interval of relief until February 2015. At that point, the patient’s symptoms led to hospitalization. He was evaluated in the Gastroenterology service of the Union of Surgeons located in La Clínica la Presentación in Manizales, Colombia. He was found to be in adequate general condition with grade three dysphagia but without significant alteration of nutritional status despite nutritional risk of dysphagia. An initial endoscopy (Figure 1) found an important area of stenosis.
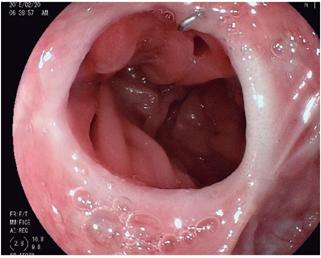
Figure 1 Initial image of postoperative stenosis. The staples and area of circumferential fibrosis can be seen.
Laboratory tests were normal, and recurrence of a tumor was ruled out by tomography. Failure of initial management with dilations and alternatives were discussed, and treatment with a radial incision and endoscopic resection of the area of the stenosis was decided upon. The procedure was performed under sedation with propofol, with prior informed consent and under the supervision of an anesthesiologist. A distal esophageal stenosis that prevented passage of a standard Fujinon 10.3 mm endoscope was endoscopically observed in the area of the esophagojejunal anastomosis (Figure 1). Radial incisions were made towards 9 o’clock and 3 o’clock. The procedure was performed with an electrocautery endoscopic tip through the working channel of the endoscope (Figure 2).
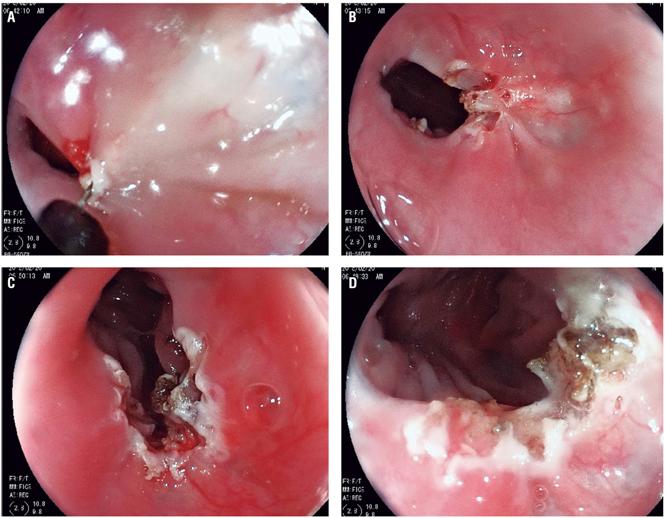
Figure 2 Endoscopic procedure. Radial incisions were made on the fibrotic segment with an electrocautery tip.
Next, the fibrotic segment was cut between the incised sites of the ring leaving the resected segment free. There was no evidence of significant bleeding or evidence of perforation, so the procedure was concluded. No steroid injection was used because an adequate diameter of approximately 12 mm had been reached. Its gross area was less than 75% of the esophageal lumen which decreased the risk of fibrosis and restenosis. In addition, one gram of sucralfate in suspension was administered orally every 8 hours as a mucosal protector.
The patient remained in the hospital for two days of additional monitoring until complete oral tolerance of a solid diet had been achieved. Fifteen days after the procedure, a follow-up examination by the treating doctor found persistent relief of symptoms. During a subsequent follow-up 30 days after the procedure, the patient reported no additional changes. He continued to tolerate a solid diet without problems. At his 60 day follow-up examination, endoscopy found continued permeability with easy and adequate passage of the endoscopy equipment and without evidence of restenosis (Figure 3).
Discussion
The first-line therapeutic option for management of esophagojejunal stenoses continues to be balloon dilation. However, stenoses that do not respond to repeated dilation and are considered to be refractory to initial management severely affect patient’s quality of life and expose them to risks from multiple sessions of pneumatic dilation. For these reasons, it is necessary to study safe and successful alternatives. This case report shows the potential of radial incision and endoscopic cutting of stenoses. This procedure allowed our patient to recover rapidly and reincorporate into his normal life without dietary limitations that affect his quality of life.
Current evidence suggests that this procedure be used principally for patients who are refractory to management by dilation and whose anastomotic stenoses are short segments measuring less than 10 mm. The procedure is also indicated for patients with Schatzki rings who develop stenosis of the esophageal lumen. The procedure has a good safety profile and achieves acceptable levels of long-term permeability. 1
On the other hand, the injection of steroids into the stenotic area has been described as additional therapy for reducing the incidence of restenosis in patients undergoing esophageal dilation and in those subjected to dissection of endoscopic submucosa. 2,3 Nevertheless, there are still no studies that demonstrate efficacy, dosage, frequency and technique.
The use of other measures such as self-expanding metal stents or plastic stents for refractory stenosis has also been demonstrated to be effective, but these methods entail complications related to overgrowth of tissue inside the stent, migration and pain. Lee et al. have demonstrated the effectiveness of stenting in 87.5% of their patients, with restenosis occurring in only 12.5%. Of these, 66% responded to pneumatic balloon dilatation as the second line of treatment. The main risk factor for restenosis was stenotic segments longer than 10 mm. Nevertheless, the study design and limited number of patients does not allow extrapolation of these results. 4 Another study with a better methodological design has attempted to randomly assign patients for primary treatment into a group treated with electrocautery and a group treated by dilation with Savary’s plugs. Comparison of the groups was unable to establish differences, but the study has opened the door to use of this technique as initial treatment of stenoses. 5,6
Another important point is definition of refractory stenoses following anastomosis. Kochman, at the University of Pennsylvania in 2005, defined them as those that fail to return to a diameter of 14 mm after five dilation sessions over a two-week interval. Most studies define stenoses as refractory after 3 dilation sessions are followed by persistent dysphagia symptoms of at least grade 2 according to Atkinson’s classification (Classification originally designed for malignant disease). 5 In addition, these studies consider an adequate diameter to be larger than10 mm, since it correlates well with relief of dysphagia. 7
In our case report, the stenosis occurred postoperatively. Nevertheless, since the stenosis was only 5 mm the RIC procedure could be used for this stenosis despite its different etiology. The use of radial incision 8,9 and endoscopic cutting with an electrocautery tip 10 is an appropriate alternative for management of refractory esophageal anastomotic stenoses. Its long-term safety and efficacy are still being evaluated, but reports to date, including the case of our patient, suggest that it be added to the repertoire of standard techniques. 9
Referencias
1. Jayanta S, Narendra D, Saroj KS, et al. Endoscopic incisional therapy for benign esophageal strictures: Technique and results. World J Gastrointest Endosc. 2015;7(19):1318-26. doi: 10.4253/wjge.v7.i19.1318. [ Links ]
2. Hanaoka N, Ishihara R, Takeuchi Y, et al. Intralesional steroid injection to prevent stricture after endoscopic submucosal dissection for esophageal cancer: a controlled prospective study. Endoscopy. 2012;44(11):1007-11. doi: 10.1055/s-0032-1310107. [ Links ]
3. Hashimoto S, Kobayashi M, Takeuchi M, et al. The efficacy of endoscopic triamcinolone injection for the prevention of esophageal stricture after endoscopic submucosal dissection. Gastrointest Endosc. 2011;74(6):1389-93. doi: 10.1016/j.gie.2011.07.070. [ Links ]
4. Lee TH, Lee SH, Park JY, et al. Primary incisional therapy with a modified method for patients with benign anastomotic esophageal stricture. Gastrointest Endosc. 2009;69(6):1029-33. doi: 10.1016/j.gie.2008.07.018. [ Links ]
5. Hordijk ML, Siersema PD, Tilanus HW, et al. Electrocautery therapy for refractory anastomotic strictures of the esophagus. Gastrointest Endosc. 2006;63(1):157-63. doi: 10.1016/j.gie.2005.06.016. [ Links ]
6. Hordijk ML, van Hooft JE, Hansen BE, et al. A randomized comparison of electrocautery incision with Savary bougienage for relief of anastomotic gastroesophageal strictures. Gastrointest Endosc. 2009;70(5):849-55. doi: 10.1016/j.gie.2009.02.023. [ Links ]
7. Kochhar R, Makharia GK. Usefulness of intralesional triamcinolone in treatment of benign esophageal strictures. Gastrointest Endosc. 2002;56(6):829-34. doi: 10.1067/mge.2002.129871. [ Links ]
8. Asada Y, Muto M. New treatment for refractory stricture of the digestive tract: radial incision and cutting (RIC). Gastrointest Endosc. 2007;65(5):AB279. doi: 10.1016/j.gie.2007.03.985. [ Links ]
9. Muto M, Ezoe Y, Yano T, et al. Usefulness of endoscopic radial incision and cutting method for refractory esophagogastric anastomotic stricture. Gastrointest Endosc. 2012;75(5):965-72. doi: 10.1016/j.gie.2012.01.012. [ Links ]
10. Simmons DT, Baron TH. Electroincision of refractory esophagogastric anastomotic strictures. Dis Esophagus. 2006;19(5):410-4. doi: 10.1111/j.1442-2050.2006.00605.x. [ Links ]
Received: August 14, 2017; Accepted: April 13, 2018











 text in
text in 



