Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.2 Bogotá Apr./June 2018
https://doi.org/10.22516/25007440.259
Case report
A case of endoscopic management of an esophageal duplication cyst
1Médico cirujano general, Universidad Pontificia Bolivariana, gastroenterólogo clínico-quirúrgico, Universidad de Caldas. Manizales, Colombia.
2Médico cirujano general, Universidad Industrial de Santander, gastroenterólogo clínico-quirúrgico, Universidad de Caldas. Manizales, Colombia.
3Médico, cirujano general, gastroenterólogo clínico-quirúrgico, coordinador del programa de Gastroenterología Clínico-Quirúrgica, Universidad de Caldas. Manizales, Colombia.
4Médico, cirujano general, Universidad de Caldas, residente de Gastroenterología Clínico-Quirúrgica, Universidad de Caldas. Manizales, Colombia.
Esophageal duplication cysts are rare congenital anomalies. Most cases are asymptomatic and their diagnoses are often incidental findings. In the past, surgery was considered to be the treatment for these lesions because of the possibility of complications such as hemorrhaging and infections as well as the fear of malignant transformation. However, the extremely low rate of malignancy and the possibility of an inadequate outcomes of surgery have made it necessary to consider other alternatives that taking both risks and benefits of the surgical procedure into account. We report the case of a 56-year-old patient with an endosonographic diagnosis of an esophageal duplication cyst who underwent endoscopic marsupialization of the cyst followed by complete resolution of symptoms, without complications, and with immediate reintegration into daily life.
Endosonography (EUS) has been widely used as a tool for evaluation and diagnosis of duplication cysts. It is the diagnostic method of choice for investigating this pathology since it can distinguish between solid and cystic lesions. The question of whether or not to perform EUS guided fine needle aspiration (FNA) of a lesion suspected of being a duplication cyst is controversial since these lesions can be infected with significant consequences. Nevertheless, EUS-FNA is often required to make a definitive diagnosis that rules out ominous lesions.
Keywords: Cyst; duplication; esophagus; endoscopic management
Los quistes de duplicación esofágica son una anomalía congénita poco frecuente. La mayoría de los casos son asintomáticos y su diagnóstico frecuentemente es un hallazgo incidental. La posibilidad de que se desarrollen complicaciones (hemorragia, infección, entre otras) y el temor a la posibilidad de transformación maligna hacen que el tratamiento de estas lesiones haya sido considerado quirúrgico en el pasado. Sin embargo, la extremadamente baja tasa de malignización y la posibilidad de un desenlace inadecuado asociado con la cirugía hacen considerar otras alternativas, teniendo en cuenta la relación riesgo-beneficio del procedimiento quirúrgico. Se reporta el caso de una paciente de 56 años con diagnóstico endosonográfico de quiste de duplicación esofágica, que fue sometida a marsupialización endoscópica del quiste con una resolución completa de sus síntomas, sin complicaciones y con una reintegración inmediata a la vida diaria.
La endosonografía (EUS) ha sido ampliamente utilizada como una herramienta para la evaluación y el diagnóstico de los quistes de duplicación. Es el método diagnóstico de elección para investigar esta patología ya que puede distinguir entre lesiones sólidas y quísticas. La cuestión de si se debe realizar o no la aspiración con aspiración con aguja fina guiada por EUS (FNA) en una lesión sospechosa, en el caso de un quiste de duplicación, es controvertida ya que estas lesiones pueden infectarse con consecuencias significativas, aunque frecuentemente se requiere que la punción obtenga un diagnóstico definitivo que descarte lesiones ominosas.
Palabras clave: Quiste; duplicación; esófago; manejo endoscópico
Introduction
Esophageal duplication cysts are benign alterations of early embryonic development that develop in the third or fourth week of gestation. They occur relatively infrequently and have an estimated incidence of 1 per 8,000 live births. Two types have been described: those that are adjacent to the lumen but do not communicate with the esophageal lumen, and those that are tubular and communicate directly to the lumen. Both types of duplication are frequently reported as different entities.
These cysts have three distinguishing characteristics: they are contained in the esophageal wall, they are covered by two muscular layers, and they are lined by a squamous epithelium or a coating compatible with that found in the embryonic esophagus. 1
Up to one third of these cysts contain gastric, pancreatic or mucosal mucosa that contains Peyer’s plaques in heterotopic form. Approximately 80% do not communicate with the lumen of the esophagus. They most frequently occur on the right lateral side of the esophagus due to the dextrorotation of the stomach during embryogenesis. 2 Symptoms caused by these lesions are most frequently observed in childhood (80% of cases). Compression of the adjacent structures most commonly causes dysphagia (70%), epigastric pain (20%), retrosternal pain (10 %), 2 and respiratory symptoms such as coughing, stridor and wheezing. Hematemesis is rarer and occurs in patients with tubular communication.
Older patients are usually diagnosed incidentally during upper endoscopy or in radiological images. Onset of symptoms is infrequent after 2 years of age. 3
Although cases of malignant transformation have been described, the true prevalence of malignancy remains unknown. To date, there have only been two cases published. The McGregor report in 1976 was a post-mortem diagnosis due to infectious causes. In 2001, Sigh reported the case of an 18-year-old patient who responded adequately to a combination of chemotherapy and radiation therapy. 4,5
Endoscopically, duplication cysts may look like other subepithelial lesions of the esophagus with a luminal protuberance associated with normal overlying mucosa without irregularities. Tubular duplications sometimes look like diverticula of varying sizes.
Endosonographic findings show homogenous anechoic lesions with regular margins derived from the submucosa (third layer). The wall can consist of three to five layers. In some cases the image is more hypoechoic than anechoic due to the presence of echogenic material consisting of layers of debris or mucin.
The diagnosis is based on endoscopic and endosonographic characteristics, but in cases that are uncertain due to hypoechoic images of the content of the cyst, EUS (FNA) has been used to clarify the diagnosis and rule out malignancy. Nevertheless, this practice is not recommended for lesions that are clearly anechoic because of the presumptive risk of infection. 6,7 Expectant management of asymptomatic cysts is possible despite the potential for complications including malignancy. This potential has led some authors to recommend surgical resection. However, there are no prospective studies that evaluate the natural history of duplication cysts, so these recommendations lack statistical strength.
Only one case of surgical treatment and one case of endoscopic treatment of symptomatic cases have been described in the literature. The first case reported, by Will et al. in 2005, was a 25-year-old patient who underwent successful fenestration of the cyst to create communication with the esophageal lumen. 8 Complete resection of the luminal wall of a cyst in a symptomatic 75-year-old patient has also been described. Polypectomy loop resection was performed due to the pseudo-pedicled characteristic of the lesion. 9
In EUS, esophageal duplication cysts frequently appear to be homogeneous hypoechoic masses in the area of the esophagus. However, when there are doubts about malignancy, FNA can be used for diagnosis of esophageal duplication cysts and duplication cysts in general, although it is controversial. While fine needle FNA can show squamous cells or other cyst contents compatible with a duplication cyst that can aid in diagnosis, the risk of infecting the cyst is a major concern. Some studies have shown infection rates as high as 14%. EUS-FNA should be performed if there is a concern of more serious damage or if the nature of the lesion is in doubt.
Clinical case
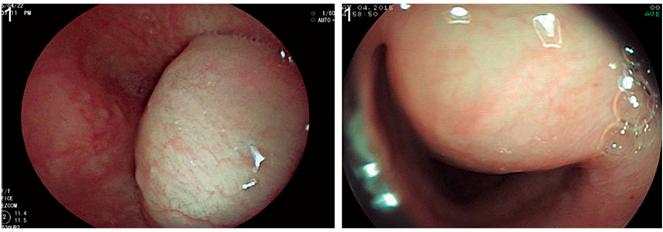
We present the case of a 56-year-old patient who had no relevant medical history. For two months prior to the procedure, the patient has suffered from dysphagia related to solids associated with a loss of 4 kg of weight. Upper digestive endoscopy found a 30 mm lesion with a subepithelial appearance and covered by a mucosa without alterations in the lower third of the esophagus in the right anterior wall (Figure 1).
Radial esophageal EUS then found a lesion dependent on the third esophageal layer, but with hypoechoic rather than anechoic characteristics. EUS-FNA with rapid cytological study was performed. Abundant mucosal material with epithelial cells and mucin but without evidence of malignant cytopathological changes was found (Figure 2).
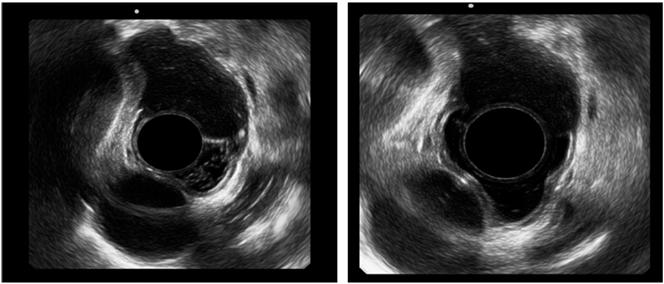
Figure 2 Radial endosonography. A subepithelial lesion of the third esophageal, hypoechoic layer is shown.
These findings supported a diagnosis of a duplication cyst without malignancy. Cyst marsupialization in a section of the luminal wall of the cyst was performed with an electrosurgical endoscopic tip with the patient under general anesthesia. A 20 mm cut was made at the zenith of the luminal lesion with dissection in steps until the submucosa was reached. Complete drainage of the lesion and complete endoscopic inspection was achieved. A blind cavity covered by pale epithelium without malignancy was found (Figure 3).

Figure 3 Incision of the lesion. Duplication cyst can be seen inside and at the end the hole that remains in the opening of the esophagus.
The patient progressed satisfactorily, and retrosternal pain was the only symptom following the procedure. It was treated successfully with common analgesics in the first 24 hours. An oral tolerance test showed no residual dysphagia.
A follow-up EUS on the fourth day after the procedure found complete collapse of the lesion (Figure 4 A) associated with total communication with the esophageal lumen and an absence of food residues (Figure 4 B).
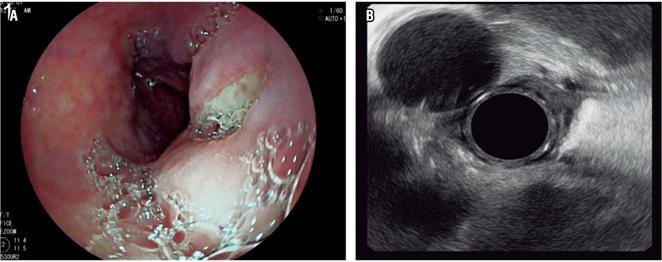
Figure 4 Follow-up EUS on the fourth day. A. Endoscopic view showing the external orifice to the esophageal lumen. B. EUS shows aorta at 11 o’clock in the viewer and the cyst already reduced following drainage.
Due to excellent post-procedure evolution and absence of residual symptoms, the patient was discharged with a mucosal protector (sucralfate) but without any requirement for analgesics. In a 10-day telephone follow-up, the patient stated that symptoms of dysphagia had completely disappeared.
Discussion
Esophageal duplication cysts are rare lesions associated with embryonic development of the bowel. Their infrequent occurrence has left the natural history of these lesions unknown. A systematic search for complications that surgical resection can entail combined the possibility of malignancy does not allow a strong recommendation for this treatment. However, the complications associated with open or minimally invasive surgery can be extrapolated. According to this method, the risk of complications ranges between 15% and 37.5%. The most likely are respiratory complications associated with thoracic surgery. In the case of an upper abdominal approach, the risk fluctuates between 16% and 17% which is a high rate of morbidity for management of a benign disease. 10
Similarly, studies of methodological design of endoscopic techniques are lacking, but the fact that endoscopy is less invasive and has little risk of respiratory alterations makes these techniques very attractive for management of duplication cysts. Endoscopic management of esophageal duplication cysts is still under development, and only two case reports have been published. 8,9 The 2005 case reported by Will et al. involved a technique similar to the one we used, but the small amplitude of the initial window (10 mm) forced an extension of the window six weeks after the initial procedure due to recurrence of symptoms. Consequently, creating a window that is sufficiently wide is essential for complete marsupialization of the cyst. In our study we used an intermediate amplitude determined by the diameter of the lesion and a stepwise technique to maximize the safety of the procedure.
Once the diagnosis of duplication cyst is established, treatment may vary depending on symptoms. In symptomatic patients, surgical resection is often the option chosen for relief of symptoms. In asymptomatic patients, surgical resection is controversial. Some authors defend resection due to the possibility of malignancy of the duplication cyst, but others have supported observation.
Since there have been case reports of stable duplication cysts monitored by EUS, this may be an appropriate method of ambulatory follow-up with surgical resection considered if the patient develops symptoms. In any case, the choice between surgical and non-surgical management of asymptomatic duplication cysts is likely to remain controversial until more is understood about the development of these cysts over time and the risk factors associated with their malignant degeneration.
To date, there are no other reports of esophageal duplication cysts that allow us to extrapolate conclusions regarding management. Our case report aims to raise the safety and efficacy of endoscopic methods for treatment of these lesions and to serve as a basis for future studies to shed light on this uncommon condition.
Referencias
1. Ildstad ST, Tollerud DJ, Weiss RG, et al. Duplications of the alimentary tract. Clinical characteristics, preferred treatment, and associated malformations. Ann Surg. 1988;208(2):184-9. https://doi.org/10.1097/00000658-198808000-00009. [ Links ]
2. Arbona JL, Fazzi JG, Mayoral J. Congenital esophageal cysts: case report and review of literature. Am J Gastroenterol. 1984;79(3):177-82. [ Links ]
3. Harvell JD, Macho JR, Klein HZ. Isolated intra-abdominal esophageal cyst. Case report and review of the literature. Am J Surg Pathol. 1996;20(4):476-9. https://doi.org/10.1097/00000478-199604000-00011. [ Links ]
4. McGregor DH, Mills G, Boudet RA. Intramural squamous cell carcinoma of the esophagus. Cancer. 1976;37(3):1556-61. [ Links ]
5. Singh S, Lal P, Sikora SS, Datta NR. Squamous cell carcinoma arising from a congenital duplication cyst of the esophagus in a young adult. Dis Esophagus. 2001;14(3-4):258-61. https://doi.org/10.1046/j.1442-2050.2001.00204.x. [ Links ]
6. Wildi SM, Hoda RS, Fickling W, et al. Diagnosis of benign cysts of the mediastinum: the role and risks of EUS and FNA. Gastrointest Endosc. 2003;58(3):362-8. https://doi.org/10.1067/S0016-5107(03)00009-9. [ Links ]
7. Wiechowska-Kozłowska A, Wunsch E, Majewski M, Milkiewicz P. Esophageal duplication cysts: endosonographic findings in asymptomatic patients. World J Gastroenterol. 2012;18(11):1270-2. doi: 10.3748/wjg.v18.i11.1270. [ Links ]
8. Will U, Meyer F, Bosseckert H. Successful endoscopic treatment of an esophageal duplication cyst. Scand J Gastroenterol. 2005;40(8):995-9. https://doi.org/10.1080/00365520510023125. [ Links ]
9. Joyce AM, Zhang PJ, Kochman ML. Complete endoscopic resection of an esophageal duplication cyst (with video). Gastrointest Endosc. 2006;64(2):288-9. https://doi.org/10.1016/j.gie.2006.04.046. [ Links ]
10. Iyer A, Yadav S. Postoperative care and complications after thoracic surgery. En: Firstenberg MS (editor). Principles and practice of cardiothoracic surgery. Intech; 2013. p. 57-84. https://doi.org/10.5772/55351. [ Links ]
Received: August 22, 2017; Accepted: April 13, 2018











 text in
text in