Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.3 Bogotá July/Sept. 2018
https://doi.org/10.22516/25007440.287
Original articles
Diagnostic efficacy of mean nocturnal basal impedance, a new parameter for the study of gastroesophageal reflux disease
1Especialista en Medicina Interna, Gastroenterología y Epidemiología. Presidente de la Asociación Colombiana de Gastroenterología. Profesor servicio de motilidad gastrointestinal, Universidad Nacional de Colombia. Director Científico, Instituto Gut Médica. Bogotá D.C., Colombia
2Especialista en Medicina Interna. Fellow de Gastroenterología y Endoscopia Digestiva, Universidad del Rosario. Bogotá D.C., Colombia
3Especialista en Cirugía. Fellow en Cirugía Gastrointestinal, Instituto Nacional de Cancerología. Bogotá D.C., Colombia
4Enfermera jefe. Magíster en Administración en Salud. Coordinadora de Educación e Investigaciones, Instituto Gut Médica. Bogotá D.C., Colombia
5Especialista en Medicina Interna y Gastroenterología, Universidad Nacional de Colombia. Hospital Universitario Méderi. Servicio de Gastroenterología y Endosonografía, Instituto Gut Médica. Bogotá D.C., Colombia
6Especialista en Medicina Interna y Gastroenterología. Profesor de posgrado, Universidad Nacional de Colombia. Servicio de Gastroenterología y Endosonografía, Instituto Gut Médica. Bogotá D.C., Colombia
7Especialista en Medicina Interna, Gastroenterología. Profesor asistente de Medicina en el departamento de Gastroenterología y Hepatología, Baylor College of Medicine. Director del Servicio de Motilidad Gastrointestinal, Baylor Medical Center. Houston Texas, EE. UU
Introduction and Objectives:
Analysis of nocturnal basal impedance (IBNM) has been proposed as a way to increase accuracy of GERD diagnosis. Our objective was to evaluate the diagnostic performance of this test in a group of patients known to have GERD.
Materials and methods:
We included 123 individuals: 58 with GERD and 65 healthy controls. They underwent consecutive pH-impedance monitoring between January 2015 and June 2017. All had undergone endoscopy in the 6 months prior to testing. Criteria used for diagnosis of GERD were abnormal acid exposure time (AET > 4.2%), pyrosis and/or regurgitation in the previous 6 months. We found 58 patients with GERD of whom 24 had erosive reflux disease (ERE) and 34 had non-erosive reflux disease (NERD). The remaining 65 were asymptomatic healthy controls with normal endoscopic results and pH impedance monitoring. A second observer who did not know the previous data measurements analyzed all pH impedance monitoring traces for IBMN. Statistical analysis included multiple Bonferroni tests for comparison between groups, linear regression for continuous variables, and receiver operating characteristic (ROC) curve analysis to find high performance IBNM values. The IBNM cutoff point was used for diagnostic precision parameters. Statistical significance was set at p <0.01, and 95% confidence intervals were used for all calculations.
Results:
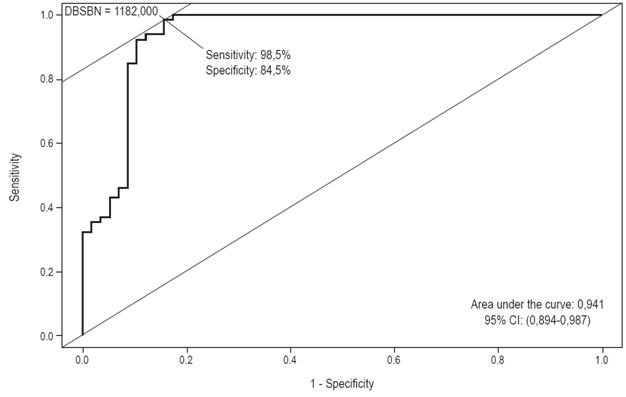
IBNM measures were significantly lower for patients with ERE and NERD than for the control group (p <0.01). A negative correlation was observed between IBNM and acid exposure time values (r = 0.59, p = <0.001) and also between IBNM and number of reflux events (r = 0.37, p = <0.001). ROC curve analysis found that the area under the curve for IBNM was 0.941 (95% CI: 0.894-0.987), and the cutoff point with the highest efficiency was 1,102 ohms (sensitivity 98.5%, specificity 84.5%). Using this value (<1.102), the IBNM had a sensitivity for detecting GERD of 91% (NERD 86% and ERE 100%) and a specificity of 98%.
Conclusion:
IBNM has high sensitivity and specificity for diagnosis of GERD. Addition of this test to conventional pH-impedance analysis and current methods for studying GERD can significantly improve our ability to diagnose this disease.
Keywords: ROC AUC; esophageal baseline impedance; pH impedance monitoring; heartburn; GERD
Introducción y objetivos:
el análisis de la impedancia basal nocturna media (IBNM) se ha propuesto para incrementar la precisión diagnóstica de enfermedad por reflujo erosiva (ERGE). Nuestro objetivo fue evaluar el rendimiento diagnóstico de esta prueba en un grupo de pacientes con ERGE conocida.
Materiales y métodos:
incluimos 123 individuos (58 con ERGE y 65 controles sanos) a quienes se les realizó pH-impedanciometría (pH-IMM) consecutiva entre enero de 2015 y junio de 2017. Todos los pacientes tenían endoscopia tomada en los 6 meses previos. El tiempo de exposición ácida (TEA) anormal (>4,2%) y la presencia de pirosis y/o regurgitación en los 6 meses previos fueron los criterios para el diagnóstico de ERGE. Se encontraron 58 pacientes con ERGE, 24 con enfermedad por reflujo erosiva (ERE) y 34 con enfermedad por reflujo no erosiva (ERNE). Los 65 restantes fueron controles sanos (CS) asintomáticos con EGD y pH-IMM normales. Todos los trazos de pH-IMM se reanalizaron para medir la IBNM por un segundo observador que desconocía los datos previos. El análisis estadístico incluyó pruebas múltiples de Bonferroni para comparar los grupos; regresión lineal para variables continuas; y análisis de curva ROC para buscar valor IBNM con mayor rendimiento. Para los diferentes parámetros de precisión diagnóstica se utilizó el punto de corte de la IBNM. Se usó significancia estadística con valor de p <0,01 e intervalos de confianza de 95% (IC 95%) para todos los cálculos.
Resultados:
los pacientes con ERE y ERNE presentaron valores de IBNM significativamente más bajos que el grupo control (p <0,01). Se observó una correlación negativa entre los valores de la IBNM y TEA (r = 0,59; p = <0,001), y también entre la IBNM y número de eventos de reflujo (r = 0,37; p = <0,001). En el análisis de curva ROC, el área bajo la curva de la IBNM fue de 0,941 (IC 95%: 0,894-0,987) y el punto de corte con mayor eficiencia 1102 ohms (sensibilidad 98,5%; especificidad 84,5%). Usando este valor (<1,102), la IBNM tuvo una sensibilidad para detectar ERGE de 91% (ERNE 86% y ERE 100%) y una especificidad de 98%.
Conclusión:
la IBNM tiene alta sensibilidad y especificidad para el diagnóstico de la ERGE. Adicionar esta prueba al análisis convencional de la pH-impedancia y a los métodos actuales de estudio de la ERGE puede mejorar significativamente nuestra capacidad para diagnosticar la enfermedad.
Palabras clave ROC AUC; impedancia esofágica basal; monitorización de pH-impedanciometría; acidez; ERGE
Introduction
Gastroesophageal reflux disease (GERD) is a condition that develops when gastric contents cause symptoms in the esophagus that are sufficiently intense to affect quality of life or cause structural damage. 1 Diagnosis of the disease can be based on symptoms and/or esophagogastroduodenoscopy (EGD) findings although the vast majority of patients’ EGDs are normal. In patients who have not undergone any sort of testing, GERD can be presumed in those symptomatic patients who respond to PPIs. However, this has important limitations, since many individuals without GERD respond to these medications through the placebo effect including when they have other diseases such as dyspepsia or eosinophilic esophagitis. In addition, some patients with demonstrated GERD may fail to respond to PPIs or may have partial and unsatisfactory clinical responses. 2,3,4 When symptoms persist despite proton pump inhibitor (PPI) therapy, the diagnosis may be in doubt and an objective evaluation is indicated. 4
Currently, measurement of esophageal pH impedance is considered to be the most complete direct test for reflux. However, this test is not totally objective. Its efficiency depends on many factors that are potential sources of error. These include the accuracy with which the patient registers symptoms during monitoring, the manual editing abilities of doctors and the variability of day-to-day perception of symptoms and acid exposure time (AET). 5 For all of the above reasons, the diagnostic accuracy of impedance pH monitoring based only on AET, symptom association probability [SAP] and the symptom index [SI]) is far from ideal.
Several studies have reported that mean nocturnal baseline impedance (MNBI), a proposed new diagnostic parameter, is an appropriate predictor of GERD. Measurements are significantly lower in patients with GERD than in control subjects who do not have GERD. This new measurement appears to be a potentially useful and easily applicable parameter for diagnosis of GERD, but studies validating it remain to be done. To date, studies of this new parameter are very scarce everywhere in the world, and in Colombia they are nonexistent. 6-11
Based on these premises, we developed this analytical study to determine the diagnostic effectiveness of this test for detection of gastroesophageal reflux disease. The main objective of this study was to establish the diagnostic yield of MNBI in a group of patients with known GERD diagnoses. The study was conducted at an outpatient referral center for studies of gastrointestinal physiology and motility.
Materials and methods
All patients considered for outpatient impedance pH monitoring to investigate GERD symptoms between January 2015 and June 2017 were considered for this consecutive study. All accepted the procedure and signed an informed consent form. The examinations were carried out at a referral outpatient center with recognized experience, which has a high technology laboratory for gastrointestinal physiology. The units of analysis are the impedance pH monitoring studies carried out during this period.
Inclusion Criteria
Patients were considered for inclusion if they were over 18 years of age, had cardinal symptoms of GERD (heartburn and/or regurgitation) at least twice a week during the previous 6 months, had had upper digestive endoscopy performed during the previous six months, and had not used PPIs in the previous four weeks.
Exclusion Criteria
The exclusion criteria were incomplete clinical data, referral to the monitoring study for investigation of extra-esophageal symptoms, Sjogren’s syndrome, scleroderma, prior esophageal or gastric surgery, use of PPIs in the previous four weeks, major esophageal motor disorders such as achalasia, jackhammer esophagus, distal esophageal spasms, and absence of peristalsis, as well as histories of esophageal or gastric cancer.
Sociodemographic variables for all patients were also recorded. They included age, gender, body mass index (BMI), socioeconomic status, occupation and origin. All data were provided by patients consecutively before performance of esophageal impedance pH monitoring. Data were collected by two of the investigators, and stored separately. To guarantee privacy and confidentiality patient identification information was eliminated from study data forms. All information was recorded in a data base designed for that purpose. Cases were numbered in chronological order from the one closest to the start date of the impedance pH monitoring period.
Esophageal pH-impedance studies
In all cases, the lower esophageal sphincter was located manometrically before transnasal insertion of the monitoring catheter. The catheter allowed monitoring of changes in intraluminal impedance at 3, 5, 7, 9, 15 and 17 cm while pH was monitored with a sensor at 5 cm above the upper edge of the lower esophageal sphincter as defined manometrically. BioView Analysis software (Sandhill Scientific, Inc., Highland Ranch, CO) which is specifically designed for analysis of esophageal manometry, was used. All traces were also analyzed manually by a single expert observer. The analysis was done in two-minute windows, using the zoom tool as needed. Symptomatic indexes were only examined for esophageal symptoms of heartburn and regurgitation if they occurred within five minutes following a reflux event. Data for episodes of liquid reflux and mixed liquid and gas reflux were analyzed to determine acid pH (nadir of pH <4) and non-acidic pH (nadir of pH> 4). The AET percentage, number of reflux events and percentage of bolus exposure were calculated. SAP and SI were considered positive if they were greater than> 95% and 50%, respectively.
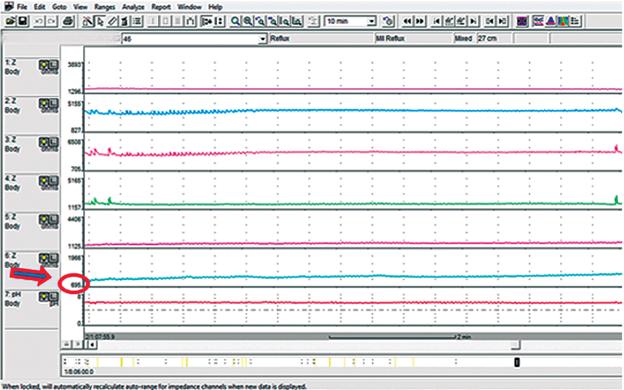
Measurement of mean night baseline impedance
MNBI was analyzed by a second observer who did not know patients’ prior data. The MNBI was evaluated in the most distal impedance channel with the patient in supine position during the night. Three 10-minute periods around 1:00 a.m., 2:00 a.m. and 3:00 a.m. were selected (Figure 1). The average baseline of each period was computed with the help of the software. Time windows containing swallowing, reflux or pH drop were avoided. The average of the three measurements was calculated manually, and the result was taken as the value of the MNBI.
Clinical Groups
All subjects who had an AET> 4.2 as measured by pH-impedance and who had cardinal esophageal symptoms were included in the group of patients with GERD. These patients were subdivided into two groups according to endoscopic findings: those with erosive esophagitis and those with NERD. Symptomatic indexes were not taken into account for diagnosis of GERD, only abnormal AET. The healthy controls were taken from a group of patients referred to our center who had no esophageal or gastrointestinal symptoms and whose endoscopy and pH-impedance measurements were normal.
Statistical analysis
Statistical tools used depended on need and the type of variable. The differences between and among the GERD, EE and NERD, and healthy control groups were analyzed through multiple pairwise tests with Bonferroni correction with a significance of p <0.05. Simple linear regressions were constructed between MNBI and AET and between MNBI and the number of reflux events in order to determine the relationship of these variables through the correlation coefficients.
A receiver operating characteristic (ROC) curve was constructed to locate the point where the GERD and control groups differed most. By measuring the area under the curve, the effectiveness of the MNBI cut-off point for determining differences was measured. The value of this cut-off point was used to calculate sensitivity, specificity, positive and negative predictive values, and accuracy for the groups. For each of these measures, 95% confidence intervals were calculated.
Ethical issues
This study is a review and reanalysis of pH-impedance traces taken consecutively in patients suspected of having GERD who had been referred to our physiology unit for this test. All clinical, demographic and physiological parameters used for the study were collected for these routine studies. The patients who underwent the examination had clear indications for the procedure and signed informed consent forms before undergoing it and in accordance with current regulations. No identification or location of patients was used in order to guarantee anonymity, privacy and confidentiality. A unique identification number for use in our database was assigned to each of the eligible patients and their corresponding study results. All of this was safeguarded under the responsibility of the institution’s research coordinator. Consolidated anonymous information was shared in a secure and confidential manner only with the team of researchers and study collaborators.
According to Article 11 of Colombian Resolution 8430 of 1993, this investigation is be classified in the no risk category. In addition, the first paragraph of Article 11 establishes that the Ethics Committee of the research institution may exempt the researcher from obtaining informed consent for this category of investigation.
Results
Demographic and Clinical Characteristics
The 123 individuals included in this study were subdivided into 3 groups. The EE group consisted of 24 patients: four with grade C/D esophagitis, eight with grade B/D esophagitis and 12 with grade A/D esophagitis (Los Angeles classification). The NERD group included 34 patients, and the group of healthy controls included 65 people. The baseline characteristics of these individuals are presented in Table 1. Patients in the EE group included 10 men and 14 women whose average age was 56 ± 14 years. Patients in the NERD group included 9 men and 25 women whose average age was 54 ± 11 years. The control group included 16 men and 49 women whose average age was 52 ± 12 years. There were no significant differences with respect to age, gender and BMI, p = ns (not significant) for all comparisons between groups. The prevalence of hiatal hernia was higher in patients with EE (54%) than in those with NERD (18%) and the control group (17%) (p <0.05 between EE and the two remaining groups), but there was no significant difference between the NERD and the control groups (p = ns).
Table 1 Demographic characteristics and pH-impedance data for patients with erosive esophagitis (EE), NERD and healthy controls
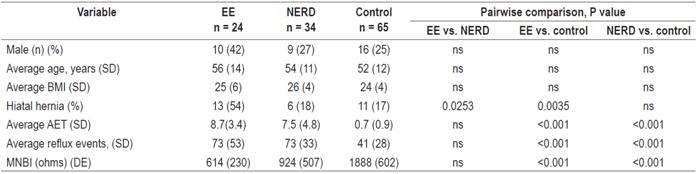
SD: standard deviation; EE: erosive esophagitis; NERD non-erosive gastroesophageal reflux; MNBI: mean night baseline impedance; BMI: body mass index; ns: difference not statistically significant; AET: acid exposure time in the esophagus.
Acid exposure time and reflux events evaluated by impedance analysis
The outpatient pH-impedance monitoring study was well tolerated by patients, and there were no technical failures or difficulties in the data analysis. The percentage of AET was not significantly different between the EE and NERD groups (8.7 + 3.4 and 7.5 + 4.8, respectively, p = ns), but was between the control group and the other two (p <. 0.001). The number of total reflux events showed a similar trend, there were no differences between the EE and NERD groups (73 + 53 and 73 + 33, respectively; p = ns), but these two groups had significantly higher numbers of events than did the control group (41 + 28, p <0.001 vs. EE vs. NERD).
Analysis of the mean night baseline impedance
MNBI analysis of the three groups was performed according to the protocol described in the methods section. The MNBIs were lower in the EE group (614 + 230) than in the NERD group (924 + 50) and the control group (1,888 + 602). The difference between the numbers for the ERGE and NERD groups is not significant (p = ns), but the differences between the control group and the other two groups are significant (p <0001) (Table 1 and Figure 2). A negative linear correlation was found between MNBI and AET (r = 0.59, p <0.001) (Figure 3). This negative correlation was also observed between the MNBI and the total number of reflux events (r = 0.37, p <0.001) (Figure 4).
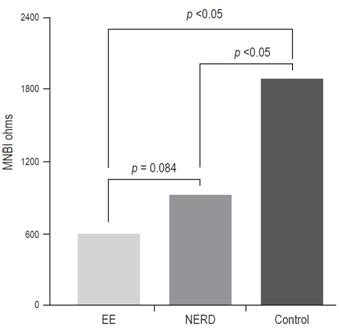
Figure 2 Mean night baseline impedance (MNBI) in patients with EE, non-erosive reflux disease (NERD) and control group.
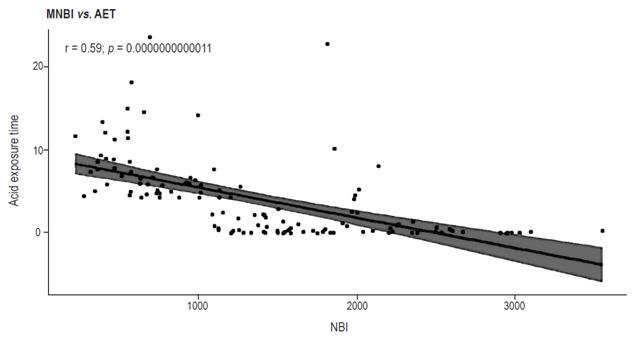
Figure 3 Linear correlation (negative) between AET and MNBI. The shaded area shows the 95% CI of the regression line.
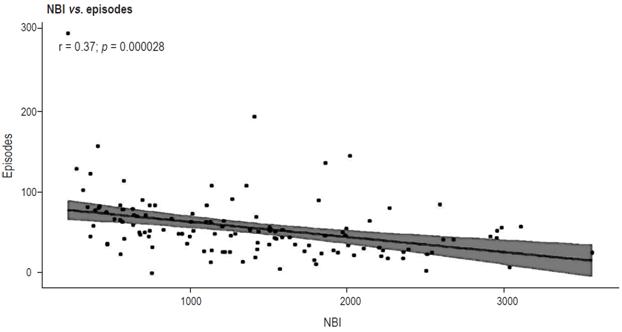
Figure 4 Negative linear correlation between number of reflux episodes and night baseline impedance. The shaded area shows the 95% CI of the regression line.
Overall capacity to diagnose GERD was determined by ROC analysis. The area under the curve (AUC) was 0.941 (95% CI: 0.894-0.987) for MNBI, and value that maximized the sum of sensitivity and specificity was 1,102 ohms (sensitivity 98.5%, specificity 84.5%). This was used as the cut-off point for evaluating prediction of GERD based on normal or abnormal acid exposure time (Figure 5).
Diagnostic yield of mean baseline nocturnal impedance in subgroups of patients with GERD
The cutoff point of the MNBI (1,102 ohms) showed high sensitivity and specificity in patients with GERD (EE and NERD). Diagnostic accuracy parameters for this test are presented in Table 2. The sensitivity of the MNBI to detect EE was higher than that for NERD (96% and 86%, respectively), but the specificity was the same for both groups (98%). In order to evaluate the capacity of MNBI to detect GERD, the same procedure was carried out for both groups of patients with high AET (GERD + NERD). The MNBI test proved highly sensitive and specific for the detection of all patients with GERD (91% and 98%, respectively).
Table 2 MNBI diagnostic parameters in patients with GERD
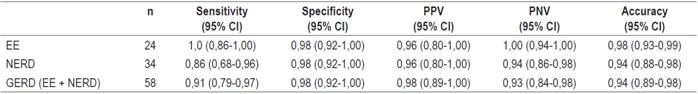
GERD: gastroesophageal reflux disease; EE: erosive gastroesophageal reflux disease; NERD: disease due to non-erosive gastroesophageal reflux; CI: confidence interval; NPV: negative predictive value; PPV: positive predictive value.
The measurements for MNBI as a diagnostic test for the groups studied are presented together with their respective confidence intervals in Table 2. None of the patients in the control group had an MNBI below 1,102 ohms, demonstrating that healthy esophagi and low acid exposure of the epithelium are associated with high levels of electrical impedance of the mucosa. On the other hand, none of the patients with EE and only five of the 34 with NERD (14%) had normal MNBI measurements. In conclusion, all measurements consistently demonstrate that low MNBI measurements are more prevalent in patients with abnormal exposure to acid and/or EE.
Discussion
In this study, we reviewed the pH-impedance tracings of 58 patients with already confirmed GERD. All had cardinal symptoms of reflux, heartburn and/or regurgitation and abnormal acid exposure, that were serious enough to seek medical attention. In addition, none of them had used PPIs in the four weeks prior to the test to ensure total absence of acid blockade. A new parameter (mean nocturnal baseline impedance) was assessed to determine its ability to predict GERD. The study has shown that its levels were significantly lower for patients with EE and NERD than for 65 healthy controls which confirms its high pathophysiological correlation with the integrity of the esophageal mucosa. Through the ROC analysis, an abnormal MNBI value <1,102 ohms was defined and adopted as a cut-off point. Using this cut-off point, the sensitivity and specificity of this test for identifying the two phenotypes of GERD, EE and NERD, were both quite high and consistent.
PH-impedance monitoring is the most widely used test for diagnosing NERD in patients with symptoms of reflux and negative endoscopy for whom PPIs totally or partially fail. 4,5 This test’s many attributes make it a candidate for the best diagnostic test. Its quantifies the total number of reflux events, determines the composition of the reflux material (air, gas or mixed), measures esophageal clearance time and bolus exposure time, determines the proximal level reached by the retrograde bolus, classifies the pH of the material refluxed as acidic, weakly acidic or weakly alkaline, and it can be used to establish whether there is any association between these events and the symptoms felt by the patient. (4
Despite all these advantages, pH-impedance monitoring is far from being an ideal test. The number of reflux events and acid exposure time of a given patient varies from day to day, so the result can be negative on a day with little pathophysiological abnormality. On the other hand, the reliability of the IS and SAP symptomatic indexes directly depend on the patient’s ability to record them accurately during monitoring. Other issues that affect diagnostic yield include the facts that pH-impedance events cannot be reliably detected in patients with low intraluminal baseline impedance and that automated analysis is unreliable and does not replace manual review of the study. Finally, there is wide interobserver variability among the doctors who review and interpret examination data. All this makes the sensitivity of conventional pH-esophageal impedance parameters depend a great deal on the individual conditions of each patient, the standardization of the examination in the different medical centers, and the experience of those who interpret the results. 12,13
Consequently, a surrogate marker for the evaluation of GERD that is not affected by these limitations is evaluation of damage to mucosal integrity associated with acid exposure. 6,7,8,9,10,11 Changes to mucosal integrity occur through the dilation of intercellular spaces that fill with electrolyte-rich liquids which are good conductors of electric current that produce a low impedance signal. (14,15 In addition, in-vivo acid exposure leads to decreasing epithelial electrical impedance in control subjects and in patients with NERD. 6 This alteration of the mucosal integrity can be evaluated by measuring increases of ionic conductance thus becoming the basis for measurement of intraluminal impedance as a marker of mucosal damage. 16 Observational studies have shown low intraluminal impedance in patients with esophagitis and in patients with NERD.
A series of 35 patients with GERD and 17 patients with functional heartburn has found that those with GERD had lower levels of impedance measured for 30 minutes at night than did those with functional heartburn. In addition, esophageal biopsies showed an inverse association between the intracellular spaces and the baseline impedance in the distal esophagus, suggesting a pathophysiological correlation between these two phenomena. That study found that an impedance cut-off point of 2,100 ohms identified patients with GERD with positive and negative predictive values of 75%. 6 Interestingly, patients with hypersensitive esophagi have also been shown to have significantly lower baseline impedance than do healthy controls with similar acid exposure times. 5
Another study of 48 patients with GERD found that mean baseline impedance rose from 886 to 1,372 ohms after administration of PPIs, indicating that the reduction of epithelial aggression factors not only decreases inflammation but also reestablishes baseline impedance levels. 8 In a cohort study of 30 patients with heartburn, the baseline impedance was significantly lower in those who responded to PPIs than in those who did not. 9 Another similar study found that a baseline impedance of 2,446 ohms had positive and negative predictive values for identifying patients with heartburn who respond to PPIs of 82% and 96%, respectively. 10
Finally, a very recent study of 289 patients with GERD found that MNBI identified patients with EE and patients with NERD with high levels of sensitivity and specificity. Sensitivity for EE was 100%, and specificity for EE was 91% while they were 99% and 86% respectively for pH positive NERD and 77% and 56% respectively for pH negative NERD. That study was based on diagnosis of patients with GERD symptoms who had responded to treatment with PPI. For this parameter the cut-off point for MNBI was 2,292 ohms. 11 The results of these studies indicate that baseline impedance correlates with changes in mucosal integrity, and that it can discriminate between NERD and hypersensitive esophagus from functional heartburn and can serve as a predictor of PPI response in patients with GERD.
In this study, patients with GERD were defined as those who had an abnormal AET greater than 4.2%. They were divided into EE and GERD groups using ROC analysis based on endoscopy. We defined the cut-off value of the MNBI that best separates patients with GERD from healthy controls with high diagnostic accuracy.
According to the ROC analysis, the best level of AUC for differentiating GERD patients from healthy patients was achieved with 1,102 ohms. To avoid adverse effects of PPIs on AUC performance, we only included patients who had not used these drugs for the previous four weeks. Our MNBI cut-off point is lower than those reported in previously mentioned studies. 9,11 This is probably because selection of healthy and sick patients in those studies was based on the symptomatic response to PPIs. Consequently, some healthy patients could have been wrongly categorized. Also patients with milder forms of GERD such as hypersensitive esophagus could have been wrongly categorized. In our study, we only admitted patients with high values of AET, with or without esophagitis, which guaranteed that all patients with GERD were truly positive. For the same reason, it is possible that the severity of the disease was greater in our sample than in those of other studies.
We found that the MNBI is inversely related to AET and to the total number of reflux events, two known parameters of the pathophysiology of GERD. This suggests that changes in MNBI are direct consequences of damage to the integrity of the mucosa. The lowest levels of MNBI were found in patients with EE which is consistent with the idea that greater epithelial damage reduces baseline impedance more and also suggests that baseline impedance could be restored with the use of PPIs.
In our series, only five of 58 patients with GERD (8.6%) had normal MNBI values (> 1,102 ohms). This corresponds to a sensitivity of 91%. All these patients belonged to the NERD group. In contrast, all patients with EE had abnormal MNBIs (<1,102 ohms), highlighting the fact that this parameter is directly related to the magnitude of epithelial damage. On the other hand, only one (1.5%) of the healthy controls had an abnormal value of MNBI conferring a high level of specificity to the test (98%). This means that the MNBI has a great capacity for ruling out GERD when measurements are normal for a given patient.
Unlike conventional pH-impedance analysis and editing that takes an average of 30 minutes, the MNBI calculation is easy. It only takes a few minutes and is not operator-dependent since it only requires measurements of the distal baseline impedance during three separate ten-minute period. Our study did not allow us to conclude that this new parameter should replace the complete impedance pH monitoring examination, but it is an additional criterion that can support or reject a diagnosis when the results are borderline or the interpretation is erroneous.
Because of MNBI’s high levels of diagnostic sensitivity and specificity, we believe when there is a high level of clinical suspicion of GERD, but normal parameters of pH-impedance measurement and abnormal values of MNBI, a diagnosis of GERD cannot be ruled out. The usefulness of this new parameter for predicting responses to surgical or endoscopic antireflux procedures in patients with refractory GERD or in those who do not respond to PPI is a point that should be investigated in future prospective studies.
In conclusion, MNBI improves the diagnostic yield of conventional esophageal impedance pH monitoring for GERD. It is not affected by the known limitations of pH-impedance because it is a reliable indicator of mucosal integrity. Adding the MNBI measurement to the conventional criteria of impedance studies can significantly improve our ability to diagnose GERD.
REFERENCES
1. Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R, Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101(8):1900-20. doi: https://doi.org/10.1111/j.1572-0241.2006.00630.x. [ Links ]
2. Numans ME, Lau J, de Wit NJ, Bonis PA. Short-term treatment with proton-pump inhibitors as a test for gastroesophageal reflux disease: a meta-analysis of diagnostic test characteristics. Ann Intern Med. 2004;140(7):518-27. doi: https://doi.org/10.7326/0003-4819-140-7-200404060-00011. [ Links ]
3. Molina-Infante J, Ferrando-Lamana L, Ripoll C, Hernandez-Alonso M, Mateos JM, Fernandez-Bermejo M, et al. Esophageal eosinophilic infiltration responds to proton pump inhibition in most adults. Clin Gastroenterol Hepatol. 2011;9(2):110-7. doi: 10.1016/j.cgh.2010.09.019. [ Links ]
4. Katz PO, Gerson L, Vela M. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013;108:308-28. doi: https://doi.org/10.1038/ajg.2012.444. [ Links ]
5. Ravi K, Katzka DA. Esophageal impedance monitoring: clinical pearls and pitfalls. Am J Gastroenterol. 2016;111(9):1245-56. doi: https://doi.org/10.1038/ajg.2016.256. [ Links ]
6. Kandulski A, Weigt J, Caro C, Jechorek D, Wex T, Malfertheiner P. Esophageal intraluminal baseline impedance differentiates gastroesophageal reflux disease from functional heartburn. Clin Gastroenterol Hepatol. 2015;13(6):1075-81. doi: 10.1016/j.cgh.2014.11.033. [ Links ]
7. Hemmink GJ, Álvarez Herrero L, Bogte A, Bredenoord AJ, Bergman JJ, Smout AJ, et al. Esophageal motility and impedance characteristics in patients with Barrett’s esophagus before and after radiofrequency ablation. Eur J Gastroenterol Hepatol. 2013;25:1024-32. doi: https://doi.org/10.1097/MEG.0b013e32836283dc. [ Links ]
8. Kessing BF, Bredenoord AJ, Weijenborg PW, Hemmink GJ, Loots CM, Smout AJ. Esophageal acid exposure decreases intraluminal baseline impedance levels. Am J Gastroenterol. 2011;106:2093-7. doi: https://doi.org/10.1038/ajg.2011.276. [ Links ]
9. Martinucci I, de Bortoli N, Savarino E, Piaggi P, Bellini M, Antonelli A, et al. Esophageal baseline impedance levels in patients with pathophysiological characteristics of functional heartburn. Neurogastroenterol Motil. 2014;26:546-55. doi: https://doi.org/10.1111/nmo.12299. [ Links ]
10. de Bortoli N, Martinucci I, Savarino E, Tutuian R, Frazzoni M, et al. Association between baseline impedance values and response proton pump inhibitors in patients with heartburn. Clin Gastroenterol Hepatol. 2015;13:1082-8. doi: https://doi.org/10.1016/j.cgh.2014.11.035. [ Links ]
11. Frazzoni M, Savarino E. Analyses of the post-reflux swallow-induced peristaltic wave index and nocturnal baseline impedance parameters increase the diagnostic yield of impedance pH monitoring of patients with reflux disease. Clin Gastroenterol Hepatol. 2016;14:40-6. doi: https://doi.org/10.1016/j.cgh.2015.06.026. [ Links ]
12. Smits MJ, Loots CM, van Wijk MP, Bredenoord AJ, Benninga MA, Smout AJ. An expert panel-based study on recognition of gastro-esophageal reflux in difficult esophageal pH-impedance tracings. Neurogastroenterol Motil. 2015;27(5):637-45. doi: https://doi.org/10.1111/nmo.12536. [ Links ]
13. Loots CM, van Wijk MP, Blondeau K, Dalby K, Peeters L, Rosen R, et al. Interobserver and intraobserver variability in pH-impedance analysis between 10 experts and automated analysis. J Pediatr. 2012;160(3):441-6. doi: https://doi.org/10.1016/j.jpeds.2011.08.017. [ Links ]
14. Tobey NA, Argote CM, Vanegas XC, Barlow W, Orlando RC. Electrical parameters and ion species for active transport in human esophageal stratified squamous epithelium and Barrett’s specialized columnar epithelium. Am J Physio Gastrointest Liver Physiol. 2007;293:70. doi: https://doi.org/10.1152/ajpgi.00047.2007. [ Links ]
15. Orlando LA, Orlando RC. Dilated intercellular spaces as a marker of GERD. Curr Gastroenterol Rep. 2009;11:190-4. doi: 10.1007/s11894-009-0030-6. [ Links ]
16. Woodland P, Lee C, Duraisamy Y, Farré R, Dettmar P, Sifrim D. Assessment and protection of esophageal mucosal integrity in patients with heartburn without esophagitis. Am J Gastroenterol. 2013;108:535-43. doi: https://doi.org/10.1038/ajg.2012.469. [ Links ]
Received: April 05, 2018; Accepted: May 24, 2018











 text in
text in