Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.3 Bogotá jul./set. 2018
https://doi.org/10.22516/25007440.281
Original articles
Effect of alcohol consumption on diagnosis of liver cirrhosis patients’ survival at a University Hospital in Medellín
1Grupo de Gastrohepatología, Facultad de Medicina, Universidad de Antioquia. Hospital Pablo Tobón Uribe, Medellín, Colombia.
2Hospital Pablo Tobón Uribe, Medellín, Colombia
Worldwide, alcohol consumption is a well-known risk factor for premature death, morbidity and disability. Records of mortality associated with alcohol consumption are not centralized. The aim of this study was to record the mortality rate associated with alcohol intake in patients with cirrhosis who were treated at a university hospital in the city of Medellin.
Materials and methods:
We included 163 patients who had been diagnosed with cirrhosis in the outpatient hepatology clinic of a 277 bed referral hospital in Medellín. Patients were monitored until 2016. Sociodemographic, paraclinical and clinical variables were measured. Alcohol consumption was considered at the beginning of the follow-up. Survival and complications associated with cirrhosis were described and recorded for patients who consumed alcohol as well as for those who did not, and then the two groups were compared.
Results:
One hundred sixty-three patients were followed until December 2016. The mortality rate among those who consumed alcohol was 51% while it was only 39% for those who did not consume alcohol (P = 0.19). Comparison of complications of cirrhosis showed that 68% of alcohol users developed ascites vs. 43% of non-consumers (P = 0.01); 40.6% of alcohol users developed encephalopathy vs. 13.5% of non-consumers (P = 0.00); and 29% of alcohol users developed hepatocellular carcinoma (HCC) vs. 17% of non-consumers (P = 0.08). In the subgroup analysis, patients with hepatitis C who consumed alcohol had a higher mortality rate than patients who did not consume alcohol (OR: 33, 95% CI: 1.06 to 1023).
Conclusions:
Although alcohol consumption was not related to increased mortality among patients with cirrhosis in this study, increased mortality was observed in the subgroup of patients with hepatitis C.
Keywords: Cirrhosis; alcohol consumption; alcoholism; mortality; chronic liver disease
El consumo de alcohol es un conocido factor de riesgo para muerte prematura, morbilidad y discapacidad a nivel mundial. Los registros de la mortalidad que se asocian con el consumo de alcohol están fraccionados. El objetivo de este estudio fue escribir la mortalidad relacionada con la ingesta de alcohol en pacientes con cirrosis atendidos en un hospital universitario de la ciudad de Medellín.
Materiales y métodos:
se incluyeron 163 pacientes con diagnóstico de cirrosis, evaluados en la consulta externa de hepatología de un hospital de referencia en la ciudad de Medellín con 277 camas y seguimiento hasta el 2016. Se midieron variables sociodemográficas, paraclínicas y clínicas. Se consideró el consumo de alcohol al inicio del seguimiento. Se describió la supervivencia y las complicaciones asociadas con la cirrosis según el estado de consumidores vs. no consumidores de alcohol.
Resultados:
se siguieron 163 pacientes hasta diciembre del 2016, encontrando una mortalidad en el 51% en consumidores de alcohol vs. 39% en no consumidores (P = 0,19). Las complicaciones de la cirrosis en consumidores de alcohol fueron ascitis en 68% vs. 43% (P = 0,01) en el grupo sin consumo de alcohol, encefalopatía 40,6% vs. 13,5% (P = 0,00) y carcinoma hepatocelular (HCC) en 29% vs. 17% (P = 0,08). En el análisis por subgrupos, los pacientes con hepatitis C con consumo de alcohol tuvieron una mortalidad más alta comparado con los pacientes que no consumieron alcohol (OR 33, IC 95%: 1,06 a 1023).
Conclusiones:
a pesar que el consumo de alcohol no se relaciona con aumento de la mortalidad en pacientes con cirrosis en este estudio, sí se observa incremento de esta en ciertas poblaciones, como en el subgrupo de pacientes con hepatitis C.
Palabras clave: Cirrosis; consumo de alcohol; alcoholismo; mortalidad; hepatopatía crónica
Introduction
Alcohol consumption is known to be a risk factor for premature death, morbidity and disability everywhere in the world. In Colombia, about 7 million people between the ages of 12 and 65 consume alcohol, and 35% consume more than 100 g/day. 1 In France, 33% of all cases of liver fibrosis are related to heavy alcohol consumption, and this is responsible for 3.8% of overall mortality, especially among young people. 2,3 The situation is not very different in the United States where alcohol consumption is considered to be the second cause of liver transplantation, and 44% of deaths due to advanced liver disease are associated with alcohol consumption. 4,5
The spectrum of liver disease caused by alcohol is broad and includes various stages which can be consecutive or overlapping which makes study of these diseases complex. 6 Steatohepatitis is described in about 90% of those who consume more than 80 g/day of alcohol. 7 After continuously high levels of alcohol consumption, alcoholic hepatitis can develop. Mortality rates reach 35%, and when it occurs in individuals with cirrhosis, the prognosis is even more ominous 8,9.
The Dionysos study of a cohort of 6,543 described the prevalence of alcohol-induced liver disease in an Italian community. It showed that consumption of more than 30 g/day was associated with increased risk for development of liver cirrhosis while consumption of more than 120 g/day of alcohol increased the risk of developing cirrhosis by 63 times. Even so, the prevalence of cirrhosis was only 13.5%. 10
The patterns of alcohol consumption associated with the development of cirrhosis and liver disease have also been studied, especially in occasional consumers of large amounts of alcohol. Binge drinking, understood as intake of alcohol sufficient to raise the blood alcohol concentration above 0.08 g/dL in 2 hours, has been considered a risk factor for cirrhosis. 11 In addition to the amount and pattern of consumption, gender has also been linked to increased risks of cirrhosis. For example, women are more likely to suffer long-term effects because they need less alcohol than men to develop liver cirrhosis. 12,13,14,15
Alcohol has a direct relationship to the development of terminal liver disease. Moreover, when it is consumed by a person with other diseases such as viral hepatitis, its harmful effect is enhanced and outcomes worsen. Consumption is also associated with higher rates of infection and cancer. 13,16-21 In Colombia, information about alcohol intake in the context of liver disease is fragmented, and we only have a few isolated reports. 22 It was found to be the primary first cause of liver cirrhosis in a population of 100 patients in Pereira, twenty-three of whom consumed alcohol. This contrasts with a report from two referral centers in Bogotá which followed a cohort of 419 patients with liver cirrhosis. Alcohol consumption was reported to be the second cause of cirrhosis accounting for 14% of patients. 23,24 In Medellín, a report on liver transplant experience at the Hospital Pablo Tobón Uribe found that alcohol cirrhosis was the second leading cause of liver transplantation between 2004 and 2010. 25 Also, alcohol consumption was a risk factor for hepatocellular carcinoma in a study conducted between 2005 and 2007 in the same institution. 26 The objective of this study was to describe the effect of alcohol consumption on the survival of patients with liver cirrhosis in a cohort of patients from Medellin.
Methodology
This is a descriptive observational study of a retrospective cohort of patients seen in the hepatology outpatient clinic of the Hospital Pablo Tobón Uribe during 2004 to 2006. The hospital is a fourth level health care institution in Medellin that has 277 beds. To be included patients had to be over 18 years of age, had to have had a diagnosis of liver cirrhosis by imaging or liver biopsy, and had to have been followed up until December 2016.
Sociodemographic, biochemical and clinical variables were evaluated at the beginning of the follow-up. Patients were classified according to their alcohol consumption in the year prior to diagnosis. High consumption was defined as more than 80 g/day in men and as more than 40 g/day in women, moderate consumption was defined as between 50 and 80 g/day in men and as between 20 and 40 g/day in women, and low consumption was defined as less than 50 g/day in men and less than 20 g/day in women. A fourth group did not consume alcohol. For calculation of mortality and complications associated with alcohol consumption, patients were classified as either alcohol consumers (regardless of quantity) and non-consumers.
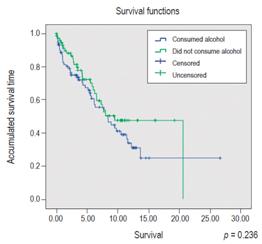
Categorical variables are presented as absolute and relative frequencies, and continuous variables are presented as medians, ranges and interquartile ranges. To assess the survival of patients, the Kaplan-Meier method was used. The Logrank test was used for the bivariate analysis, with a statistical significance value of p <0.05. The outcome of interest for this analysis was death, and transplant patient data were censored. Tabulation and analysis of data were done through Epidat 4.2, and survival curves were made with SPSS 21. The study was approved by the Ethics Committee of the Hospital Pablo Tobón Uribe and is classified as a study without risk according to Resolution 8430 of 1993. The researchers adhered to the 2013 version of the Helsinki Declaration.
Results
We included 163 adult patients who had been diagnosed with liver cirrhosis. Sixty-four percent were male (Table 1). According to the clinical history reports, the median age was 60 years with an interquartile range (IQR) of 52 to 66 years, and 68% were of mixed race. The most frequent cause of cirrhosis was alcohol consumption (64/163 or 39%). At the start of follow-up, 35.5% of patients were classified as Child Turcotte Pugh (CTP) A. Observed complications related to cirrhosis were ascites in 57% of patients, coagulopathy in 36%, variceal bleeding in 32%, encephalopathy in 28%, and hepatocellular carcinoma in 23%.
Table 1 Demographic and clinical characteristics of 163 patients diagnosed with liver cirrhosis and treated at the Hospital Pablo Tobón Uribe between 2004 and 2006.
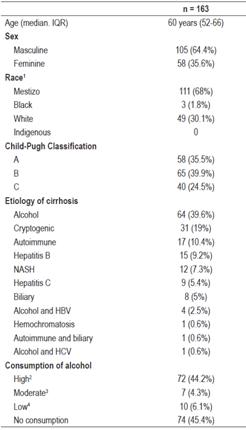
1 According to report in the clinical history.
2 More than 80 g/day of alcohol in men and more than 40 g/day in women.
3 Between 50 and 80 g/day of alcohol in men and between 20 and 40 g/day in women.
4 Less than 50 g/day of alcohol in men and less than 20 g/day of alcohol in women.
With regard to alcohol consumption, 45.4% reported no consumption of alcohol, 44.2% of patients reported high alcohol consumption, 6.1% of patients reported low consumption, and 4.2% of patients reported moderate consumption. Eighty-nine percent of alcohol users were male, with a median age of 60 years (IQR 29 to 82 years). Among those who did consume not alcohol, 67% were female (P = 0.00). Ascites was found in 68% of alcohol users and 43% (P = 0.00) of the group without alcohol consumption. Thirty-seven patients (41%) were CTP B, 26 patients (29%) were CTP A, and 26 patients (29%) were classified as CTP C (Table 2).
Table 2 Comparison of outcomes of patients who consumed alcohol with those of patients who did not consume alcohol in a cohort of 163 patients diagnosed with liver cirrhosis and treated at the Hospital Pablo Tobón Uribe.
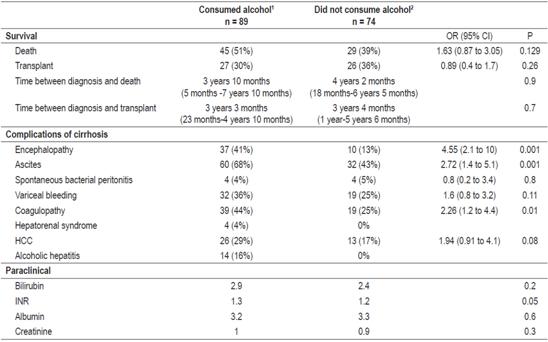
1 Any high, moderate or low alcohol consumption.
2 Without alcohol consumption.
Mortality was 45% (74/163) with a median survival of 4 years and 2 months after diagnosis. Fifty-three patients (33%) underwent liver transplantation after a median time of 3 years and 4 months. Of the patients who consumed alcohol, 45 patients (51%) died after a median time of 3 years and 10 months compared to 4 years and 2 months in the group who did not consume alcohol (P = 0.9). The OR for death was 1.63 (95% CI: 0.87 to 3.05). There were 21 CPT B patients (46%), 13 CPT C patients (28%) and 11 CTP A patients (25%).
The patient breakdown according to the etiology of cirrhosis was 17 cases of autoimmune etiology (10.4%) all whom did not consume alcohol, 10 cases of CTP B (59%) and 7 patients classified as CTP A (41%). Ten patients with other etiologies did not consume alcohol, one of whom had hereditary hemochromatosis and was classified as CTP C. The remaining 10 patients had cirrhosis of biliary etiology. One patient was classified as CTP 3 (5%), and four were classified as CTP 2.
Nineteen patients (11.7%) had cirrhosis due to hepatitis B. Nine of them (47%) reported alcohol consumption, three reported high consumption. Six patients died (6/19, 31%), two patients (2/9, 22%) who consumed alcohol and four patients (4/10, 40%) who did not (OR 0.43, 95% CI 0.060 to 3.22, P = 0.4). Nine patients (47%) underwent liver transplantation: five of these patients (55%) had consumed alcohol and four (40%) had not (OR 1.88, 95% CI: 0.3 to 11.63; = 0.4). Three patients in the group of alcohol users (33%) had HCC, and three patients in the group of non-alcohol users (30%) presented HCC (OR 1.17, 95% CI 0.17 to 8.09, P = 0.8)
Of the 10 patients with cirrhosis due to hepatitis C, five (50%) reported alcohol consumption, and five (50%) were abstainers. Of these, two were classified as CTP B, two as CTP C and one as CTP A. Four patients died during the follow-up, all of whom were alcohol users (OR 33, 95% CI: 1.06 to 1023). Of these, two were classified as CTP B, one as CTP A, and one as CTP C. Five patients underwent liver transplantation, four of whom ( 80%) had not been alcohol consumers, and one patient (20%) who had been an alcohol consumer and was classified as CTP A and had HCC (OR 2.25, 95% CI: 0.06 to 87, P = 0.058). There were two cases of HCC, one in the group of alcohol users and another in the non-consumer group.
Of the 31 patients with cirrhosis of cryptogenic etiology, there were 8 (25%) with moderate alcohol consumption, and 23 (74%) without alcohol consumption. Eighteen patients (58%) died: six (75%) were alcohol users and 12 (52%) were non-alcohol users (OR 2.75, CI 0.46 to 16, P = 0.2). A total of 9 patients (29%), two from the group of alcohol users (25%) and seven (30%) from the group without alcohol consumption, underwent liver transplantation (OR 0.76, 95% CI: 0.1 to 4.7; P = 0.4). Ten patients had HCC, four (50%) with alcohol consumption and six (26%) without alcohol consumption (OR 1.83, CI 0.53 to 15) (Figure 1).
Twelve patients (7.3%) had cirrhosis due to non-alcoholic steatohepatitis, three of whom reported low alcohol consumption (25%). Eight patients (66%), including two of those who consumed alcohol(66%) and six of those who did not (66%). One patient from each group underwent liver transplantation (OR 4, 95% CI 0.17 to 95, P = 0.3).
Of the 64 patients who had alcoholic cirrhosis, 62 (96%) had high levels of consumption, and two (4%) had moderate consumption. Thirty-one patients (41%) died during the follow-up period. Thirty of these patients had high levels of alcohol consumption (OR 0.94, CI 0.06 to 15). Of the 17 patients who underwent liver transplantation, 16 had high levels of alcohol consumption (OR 0.35, 95% CI 0.02 to 5.8), and 15 of the 16 cases of HCC also showed high levels of alcohol consumption.
Discussion
Alcohol consumption has been a topic of interest in Colombia which has a national strategy against alcohol consumption. 1 Patients with cirrhosis have been characterized in Pereira and Bogotá at two referral centers, and in the city of Medellín at the Hospital Pablo Tobón Uribe where the characteristics of the patients who underwent liver transplantation were described. This study described the characteristics of a cohort of 163 patients diagnosed with liver cirrhosis who had been followed for 10 years during which time the consumption of alcohol was also quantified to evaluate its effect on the survival of patients with established cirrhosis. 24
Alcohol consumption was the most frequent cause of cirrhosis in this cohort, similar to what was found in the Pereira cohort and in other cohorts followed in Europe and the United States.3,23,28 Patients observed in the seventh decade of life, predominantly men, had variable severity of liver disease. At the start of follow-up 2/3 of the patients had decompensated cirrhosis, with CTP B and CTP C accounting for 65% of the population described. This is probably related to the late access of patients to institutions with a high level of complexity, such as the Hospital Pablo Tobón Uribe, at the time of development of complications associated with cirrhosis.
Hepatitis B and C were observed in 17% of these patients. About 50% reported some type of alcohol consumption. The majority of them reported high consumption with only 6% reporting low consumption. Low levels of consumption have been found in European and Eastern populations where it has been related to a decrease in cardiovascular mortality in non-cirrhotic patients and a reduction in the presence of steatohepatitis in Japanese patients. 28,29. However, in our population very few patients had low consumption of alcohol.
The mortality rates of alcohol consumers non-consumers were the same, but survival time between the diagnosis of cirrhosis and death was greater in the group of non-alcohol users although the difference was not statistically significant. This is explained by the access of patients to liver transplantation. Twenty-seven percent of the patients who consumed alcohol underwent liver transplantation which altered the natural history of alcohol consumption. Of the 53 liver transplant patients, 16 (30%) had cirrhosis due to alcohol, but none of these patients had alcoholic hepatitis. Alcohol cirrhosis was the main reason for transplantation at Hospital Pablo Tobón Uribe.
The relationship between alcohol consumption and mortality due to cirrhosis has been described in multiple cohorts. The amount and pattern of consumption as well as the type of alcoholic beverage consumed are determinants in the development of liver disease and death related to cirrhosis. This constitutes a limitation for studies with long follow-up periods such this study. Consumption patterns and the quantity and characteristics of beverages tend to vary over time which makes their evaluation as determinants impossible. When alcohol consumption associated with the different etiologies of liver cirrhosis is detailed, we observed an increase in mortality in patients with hepatitis C. All these patients who died had had high levels of alcohol consumption and appeared to be as sick as the non-consumers with similar CTP classifications. This situation is similar to those reported in the literature. Patients with autoimmune liver cirrhosis did not report alcohol consumption unlike patients with other etiologies of cirrhosis.
With respect to the complications associated with cirrhosis, obviously patients who consumed alcohol had more complications than those who did not. This situation may result in longer hospital stays with greater costs, but this was not considered in this study and requires additional studies.
Among the strengths of this study are its 10-year follow-up of all patients and the size of the cohort. The quantification of alcohol consumption allowed establishment of the relationship between the amount of alcohol consumed and increased mortality in scenarios such as hepatitis C.
Categorization of alcohol consumption according to the international literature could be seen as a limitation of this study, since the Colombian population, specifically that of Medellín, may need different amounts of alcohol to die from cirrhosis. This study was designed to determine mortality due to any cause which is also a limitation. Under this approach, other variables were not evaluated, such as hospitalizations during follow-up. In addition, it should be noted that 30% of patients who consumed alcohol underwent liver transplantation.
Conclusions
Although alcohol consumption did not increase mortality in this cohort, the survival times of patients with hepatitis C with similar CTP ratings did decrease. Alcohol consumption was the main cause of cirrhosis in this cohort, and consumption increased occurrence of complications of cirrhosis which are signs of decompensation of liver disease. With respect to the pattern of alcohol consumption, this cohort had extreme consumption, with similar numbers in the high consumption group and the non-alcohol consumption group. Liver transplantation in this population changed the natural history of the disease which could explain the similar mortality rates in the two groups of our cohort with respect to those reported in the other referenced cohorts.
Acknowledgements
We would like to thank Luis Enrique Martínez R, Luisa Calle, Juan David Vélez, Natalia Giraldo, Juan Camilo Pérez
REFERENCES
1. Ministerio de Salud. Estrategia nacional de respuesta integral frente al consumo de alcohol en Colombia. 2013. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/ENT/estrategia-nacional-alcohol-colombia.pdf [ Links ]
2. Roulot D, Costes JL, Buyck JF, Warzocha U, Gambier N, Czernichow S, et al. Transient elastography as a screening tool for liver fibrosis and cirrhosis in a community-based population aged over 45 years. Gut. 2010;60:977-84. doi: https://doi.org/10.1136/gut.2010.221382. [ Links ]
3. European Association for the Study of the Liver. EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol. 2012;57(2):399-420. doi: https://doi.org/10.1016/j.jhep.2012.04.004. [ Links ]
4. Sherlock S. Alcoholic liver disease. Lancet. 1995; 345 (8944): 227-9. doi: https://doi.org/10.1016/S0140-6736 (95)90226-0. [ Links ]
5. Yoon YH, Yi HY, Thomson PC. Liver cirrhosis mortality in the United States, 1970- 2009, surveillance report #93. National Institute on Alcohol Abuse and Alcoholism. 2012. [ Links ]
6. Plunk AD, Syed-Mohammed H, Cavazos-Rehg P, Bierut LJ, Grucza RA. Alcohol consumption, heavy drinking, and mortality: rethinking the j-shaped curve. Alcohol Clin Exp Res. 2014;38(2):471-8. doi: https://doi.org/10.1111/acer.12250. [ Links ]
7. Dugum M, Mccullough A. Diagnosis and management of alcoholic liver disease. J Clin Transl Hepatol. 2015;3(2):109-16. doi: 10.14218/JCTH.2015.00008. [ Links ]
8. Mathurin P, O’Grady J, Carithers RL, Phillips M, Louvet A, Mendenhall CL, et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: meta-analysis of individual patient data. Gut. 2011;60(2):255-60. doi: https://doi.org/10.1136/gut.2010.224097. [ Links ]
9. Mathurin P, Moreno C, Samuel D, Dumortier J, Salleron J, Durand F, et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med. 2011;365(19):1790-800. doi: 10.1056/NEJMoa1105703. [ Links ]
10. Bellentani S, Saccoccio G, Costa G, Tiribelli C, Manenti F, Sodde M, et al. Drinking habits as cofactors of risk for alcohol induced liver damage. The Dionysos Study Group. Gut. 1997;41:845-50. doi: https://doi.org/10.1136/gut.41.6.845. [ Links ]
11. Chacko KR, Reinus J. Spectrum of alcoholic liver disease. Clin Liver Dis. 2016;20(3):419-27. doi: https://doi.org/10.1016/j.cld.2016.02.002. [ Links ]
12. Saitz R. Unhealthy alcohol use. N Engl J Med. 2005; 352(6):596-607. doi: https://doi.org/10.1056/NEJMcp042262. [ Links ]
13. Chan C, Levitsky J. Infection and alcoholic liver disease. Clin Liver Dis. 2016;20(3):595-606. doi: https://doi.org/10.1016/j.cld.2016.02.014. [ Links ]
14. Mandayam S, Jamal MM, Morgan TR. Epidemiology of alcoholic liver disease. Semin Liver Dis. 2004;24:217-32. doi: https://doi.org/10.1055/s-2004-832936. [ Links ]
15. Lieber CS, Jones DP, Decarli LM. Effects of prolonged ethanol intake: production of fatty liver despite adequate diets. J Clin Invest. 1965;44:1009-21. doi: https://doi.org/10.1172/JCI105200. [ Links ]
16. Albanis E, Friedman SL. Pathogenesis and principles of therapy. Curr Futur Treat Ther Liver Dis. 2001;5(2):315-34. [ Links ]
17. Larkin J, Clayton MM, Liu J, Feitelson MA. Chronic ethanol consumption stimulates hepatitis B virus gene expression and replication in transgenic mice. Hepatology. 2001;34:792-7. doi: https://doi.org/10.1053/jhep.2001.27565. [ Links ]
18. Westin J, Lagging LM, Spak F, Aires N, Svensson E, Lindh M, et al. Moderate alcohol intake increases fibrosis progression in untreated patients with hepatitis C virus infection. J Viral Hepat. 2002;9:235-41. doi: https://doi.org/10.1046/j.1365-2893.2002.00356.x. [ Links ]
19. Lin CW, Lin CC, Mo LR, Chang CY, Perng DS, Hsu CC, et al. Heavy alcohol consumption increases the incidence of hepatocellular carcinoma in hepatitis B virus-related cirrhosis. J Hepatol. 2013;58:730-5. doi: https://doi.org/10.1016/j.jhep.2012.11.045. [ Links ]
20. Seitz H, Sticke LF. Molecular mechanisms of alcohol-mediated carcinogenesis. Nat Rev Cancer. 2007;7(8):599. doi: https://doi.org/10.1038/nrc2191. [ Links ]
21. Jee SH, Ohrr H, Sull JW, Samet JM. Cigarette smoking, alcohol drinking, hepatitis B, and risk for hepatocellular carcinoma in Korea. J Natl Cancer Inst. 2004;96:1851-6. doi: https://doi.org/10.1093/jnci/djh334. [ Links ]
22. Suárez Quintero Y. Consumo de alcohol en Colombia: ¿sabemos en qué estamos? Rev Colomb Gastroenterol. 2015;30(4):387-8. [ Links ]
23. Giraldo A, Barraza M, Villa H, Martínez J, García G. Caracterización epidemiológica de pacientes con cirrosis en una consulta de gastroenterología en Pereira, Colombia, 2009-2012. Rev Med Risaralda. 2014;20(5):86-94. [ Links ]
24. Prieto JE, Sánchez S, Prieto RG, Rojas EV, González L, Mendivelso F. Características clínicas y descompensación en pacientes con cirrosis hepática atendidos en dos centros de hepatología en la ciudad de Bogotá DC, 2010-2014. Rev Colomb Gastroenterol. 2016;31(1). doi: http://dx.doi.org/10.22516/25007440.66. [ Links ]
25. Santos O, Londoño M, Marín J, Muñoz O, Mena A, Guzmán C, et al. An experience of liver transplantation in Latin America: a medical center in Colombia. Colomb Med. 2015;46:8-13. [ Links ]
26. Cortes-Mancera F, Loureiro CL, Hoyos S, Restrepo JC, Correa G, Jaramillo S, et al. Etiology and viral genotype in patients with end-stage liver diseases admitted to a hepatology unit in Colombia. Hepat Res Treat. 2011;2011:363205. doi: 10.1155/2011/363205. [ Links ]
27. Singal AK, Kamath PS, Gores GJ, Shah VH. Alcoholic hepatitis: current challenges and future directions. Clin Gastroenterol Hepatol. 2014;12(4):555-64. doi: 10.1016/j.cgh.2013.06.013. [ Links ]
28. Chiva-Blanch G, Arranz S, Lamuela-Raventos RM, Estruch R. Effects of wine, alcohol and polyphenols on cardiovascular disease risk factors: evidences from human studies. Alcohol Alcohol. 2013;48(3):270-7. doi: 10.1093/alcalc/agt007. [ Links ]
29. Sogabe M, Okahisa T, Taniguchi T, Tomonari T, Tanaka T, Tanaka H, et al. Light alcohol consumption plays a protective role against non - Alcoholic fatty liver disease in Japanese men with metabolic syndrome. Liver Int. 2015;35(6)1707-14. doi: 10.1111/liv.12754. [ Links ]
Received: April 28, 2017; Accepted: May 07, 2018











 texto en
texto en