Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.3 Bogotá jul./set. 2018
https://doi.org/10.22516/25007440.285
Review articles
Necrotizing esophagitis (black esophagus): Presentation of cases and literature review
1Facultad de Medicina. Departamento de Medicina Interna. Unidad de Gastroenterología. Universidad Nacional de Colombia. Médico Gastroenterólogo, Gastroinvest S.A.S. Bogotá, Colombia. Correo electrónico: laangela@unal.edu.co
2Médico Cirujano, Gastroinvest S.A.S. Bogotá, Colombia
3Médico Gastroenterólogo, Gastroinvest S.A.S. Bogotá, Colombia.
Acute necrotizing esophagitis (black esophagus) is a rare pathology that is characterized by partial or total loss of the epithelium, ulceration up to the circumferential slough of all layers of the mucosa and submucosa, frequent involvement of deep muscle layers, and frequent perforations. Its blackish appearance in endoscopic examinations has given it the name of black esophagus. Five illustrative cases, all concordant with descriptions the medical literature, are presented in this study together with a review of the literature, case descriptions and risk and prognosis factors.
Key words: Necrotizing esophagitis; black esophagus; acute esophageal necrosis; case description; review; risk factors
La esofagitis necrotizante aguda (esófago negro) es una patología grave poco frecuente, que se caracteriza por presentar pérdida parcial o total del epitelio, con ulceración hasta el esfacelo circunferencial de todas las capas de la mucosa y submucosa. También se evidencia compromiso frecuente de las capas profundas musculares y perforación, con aspecto negruzco al examen endoscópico, que le ha dado su nombre más conocido, el de esófago negro. Se presentan cinco casos ilustrativos concordantes con la descripción de la literatura médica, que luego de ser revisada reportó todos los casos descritos, junto con los factores de riesgo y pronóstico.
Palabras clave: Esofagitis necrotizante; esófago negro; necrosis esofágica aguda; descripción de casos; revisión; factores de riesgo.
Introduction
Acute esophageal necrosis (AEN) is a rare pathology that presents in the mucosa with severity varying from partial loss of the epithelium with ulceration to the necrosis of all mucosal layers, compromise of deep muscular layers and perforation. It present as focal or extensive necrosis. Due to its blackish color under endoscopic examination, it is best known as black esophagus. There is little literature on the subject, its pathophysiology is unknown, and it can be easily confused with caustic burns because of its appearance. The first two cases were described by Brennan and by Lee et al in a patient with extensive esophageal necrosis and in a patient with severe hypothermia and spontaneous aortic rupture with extensive esophageal infarction.1,2
Given AEN’s dramatic nature from an endoscopic point of view and its clinical picture and possible outcomes, we decided to conduct a review of the available medical literature.
Subjects and methods
We describe five cases of patients with endoscopic diagnoses of acute esophageal necrosis who were treated in medical centers in Bogotá. Their clinical evolutions were compared with findings provided by the literature.
The review was carried out through searches in PubMed, Scielo, Google, Ovid, Hinari, Springer, Ebsco and Sinab (National University), using the terms “ Black esophagus”, “black esophagus”, “black oesophagus”, “necrotizing” AND “oesophagitis”, “necrotizing” AND “esophagitis”, and “necrotizing esophagitis”. The search was repeated in the bibliographies of all the articles found. All articles were accepted if they were in English, French, Spanish or Portuguese, or if at least the abstract was in one of these languages. We found a systematic review of the literature by Day and Sayegh, 2010 which included all the cases described until 2008. 3 We proceeded to describe cases reported from then until August 2017. Then we consolidated them into a table by authors in the same format used by Day and Sayegh to make them comparable and to adequately describe the totality of the cases.
Descriptions of cases
Case 1 (JL)
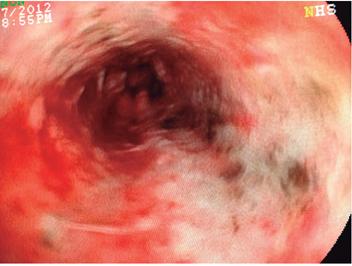
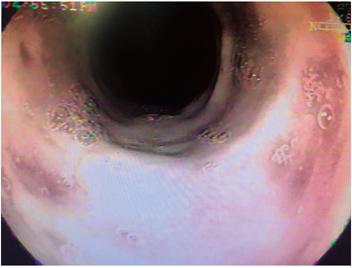
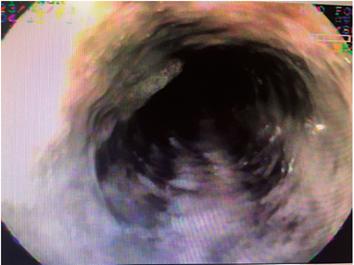
The patient was a 79-year-old woman who came to the emergency room because of melena and altered consciousness. Her medical history included resected meningioma, secondary seizure syndrome, uncontrolled arterial hypertension, and chronic obstructive pulmonary disease. Upon examination she was found to have leukocytosis with neutrophilia (89%); creatinine of 1.84 mg/dL, hypochloremia (92 mEq/L) and hyponatremia (129 mEq/L). Endoscopy showed esophageal epithelial necrosis in the lower two thirds and diffuse bleeding (Figures 1, 2, 3 and 4) without changes in the caliber of the esophagus. Her evolution and outcome are unknown.
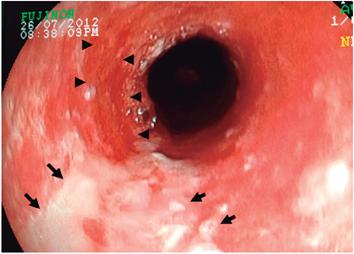
Figure 1 Fragments of necrotized mucosa in the proximal middle third of the esophagus (arrows) and bleeding in mucosal layer (arrowheads) (Case 1).
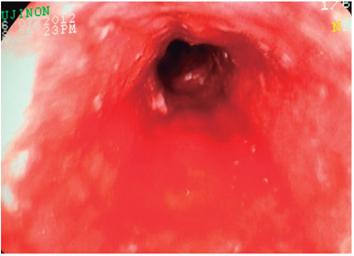
Figure 2 Diffuse necrotized remnants of the mucosa in the middle third of the esophagus with bleeding in mucosal layer (Case 1).
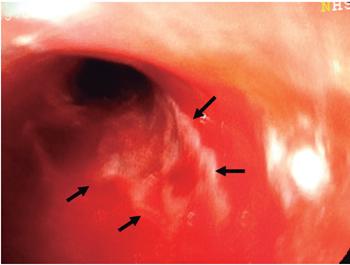
Figure 3 Fragments of necrotized esophageal mucosa in the middle third (arrows) and bleeding in mucosal layer (case 1).
Case 2 (MDA)
The patient was a 79-year-old who was seen for a follow-up examination due to a history of digestive hemorrhaging. She was treated in the emergency room due to endoscopic findings of proximal candidiasis and circumferential ulceration with a red, brown and black appearance suggesting hematin, areas of necrosis, friability, easy bleeding upon contact with the endoscope in the middle and distal third with severely edematous and rigid mucosa, without stenosis (no photographic document). The alterations disappear at the Z line which was raised to 32 cm. The widened esophageal hiatus had a giant hiatal hernia. She was diagnosed with severe esophagitis suggestive of a caustic injury. Biopsies performed on the distal esophagus showed acute esophagitis with extensive mucosal and submucosal necrosis, reactive epithelial damage, but with a viable muscular layer. The patient and family members said that there was no possibility of ingestion of caustics. The patient had had iron deficiency anemia four years before and had undergone previous endoscopies due to digestive hemorrhaging. She had had a 9 cm hiatal hernia one year earlier and Cameron erosions four years earlier. An endoscopic follow-up one month later showed a giant 9 cm hiatal and chronic erosive gastritis in the antrum with chronic mild non-atrophic gastritis in the antral biopsies.
Case 3 (HS)
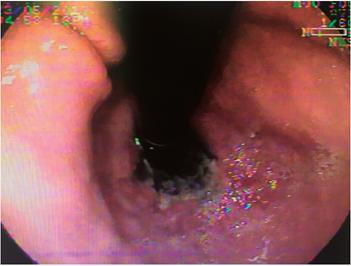
The patient was a 76-year-old man who had been referred for consultation due to three days of severe pain in the right hypochondrium with malaise, asthenia and adynamia. The examination was painful, and the patient had tachycardia, tachypnea, jaundice, and labored breathing with rales on the right side. He had no fever but tested positive for Murphy’s sign. The patient had a history of type 2 diabetes mellitus and arterial hypertension and had had right basal pneumonia, septicemia, thrombocytopenia, benign prostatic hypertrophy, exacerbated chronic renal failure, cholelithiasis with dilation of the bile duct and choledocholithiasis. An incidental finding during endoscopic ultrasonography was black mucosa throughout the entirety of the esophagus. It was covered with mucous exudate, without erosions, ulcers or narrowing, but the mucosa below the Z-line had the usual appearance. Videoendoscopy demonstrated esophageal ulceration from 21 cm of the dental arch which became circumferential at 23 cm. It was covered by black and gray fibrin from 27 cm to the gastroesophageal junction (Figures 5, 6 and 7) but the cardiac mucosa was unaffected (Figure 8). Endoscopic retrograde cholangiopancreatography (ERCP) demonstrated a dilated extrahepatic bile duct with filling defect in the middle and distal third. A small sphincterotomy was performed to address thrombocytopenia (31,000 platelets/mm3) (Figure 9), and small stones were removed with a balloon,. A 7 Fr x 7 cm plastic stent was placed. Bile drainage was clear but with microcalcifications. The patient’s development was satisfactory, and he was discharged after resolution of pain and jaundice. At 10 weeks he was asymptomatic and chose not to continue follow-up procedures.
Case 4 (JMR)
The patient was an 81-year-old man who had been diagnosed with mesenteric thrombosis and gastrointestinal bleeding. Digestive endoscopy showed that the entire esophageal mucosa had areas of necrosis, hemorrhaging, and ulcerated lesions covered by fibrin. However, there were no signs of active bleeding or perforations. The irregular Z line was located at 38 cm from the dental arch. The diagnosis was pancreatic necrosis and chronic pangastritis. There are no photographic records or later records of this patient.
Case 5 (MECL)
The patient was a 73-year-old woman who had been diagnosed with digestive hemorrhaging. Digestive endoscopy showed a large hematoma in the posterior wall of the esophagus, with mucosal dissection and spontaneous bleeding. There was mucosa in the middle third with areas of necrosis and mucosal fragments, but the distal third was normal. There are no photographic records or later records of this patient.
Discussion
Epidemiology
Acute esophageal necrosis (AEN), or black esophagus, is a rare condition that was initially described in autopsies of isolated cases. 1,2 Then a series of autopsies found a frequency of 0% to 0.02%, (4,5 and more recently a series of 310 autopsies found 32 cases of esophageal necrosis for an incidence of 10.3%. 6 According to the authors of one study, the subsequent appearance of endoscopy has led to findings of frequencies that range from 01% to 0.28% of endoscopies. 7 Grudell reported an incidence of 0.008% (Six cases out of 78,847 endoscopies), 8 Ramos described an incidence of 0.28% in a series of 3,976 consecutive endoscopies, 9 Gómez reported an incidence of 0.11% in a series of 6,011 consecutive endoscopies, 10 and Yasuda reported an incidence of 6% for endoscopies performed due to acute digestive hemorrhaging over a period of three years. 11 Our cases do not allow establishment of relative frequency, given that they are isolated cases in third-level institutions, although no episodes were found in a set of 12,638 endoscopies performed at a second-level diagnostic center. 12 This reflects the severity of the entity which, according to the literature, has associated comorbidities in 83% of all cases. 3,7. There is a predominance of male patients and elderly patients, particularly in the seventh and eighth decades. 3,7 The average age of our patients was 78 years. There were three women (60%) for 70 years and male dominance (3: 1) in the total series (Table 1).
Table 1 Summary of the most frequent findings in patients with necrotizing esophagitis (black esophagus) described in the literature*
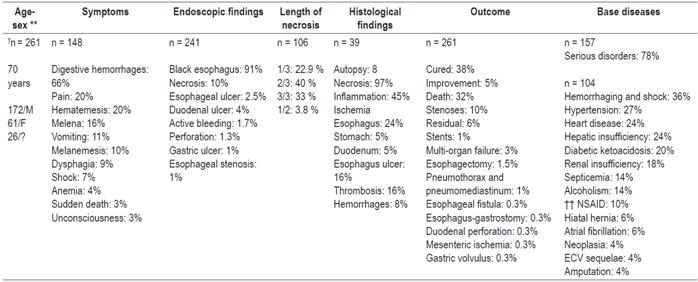
* Consolidated clinical findings and outcomes in all cases described in the literature 3,8,9,10,11,13-81.
** Sex: M: male, F: female.
† n: number of patients whose description is available for the corresponding item
†† NSAIDs: non-steroid anti-inflammatory drugs.
Clinical presentation
The previous literature described 261 cases of AEN. Together with the five cases described here, there are now 266 published cases. The vast majority of studies are descriptions of isolated cases, but there are some large series including one with 29 cases, 13 and one with 16 cases. 11 Only three extensive reviews of the literature were found. In 2006, Grudell et al. collected the first 52 cases of AEN reported between 1963 and 2003. 8 In the second, published in 2007, Gurvitts et al. collected 88 additional cases. (81) In the third study, Day and Sayegh collected the remaining cases until 2008. 3 Tables 1 and 2 show the data and findings of all the cases described in the literature. 3,8-11,13-81
Table 2 Cases of necrotizing esophagitis (black esophagus) described in the medical literature
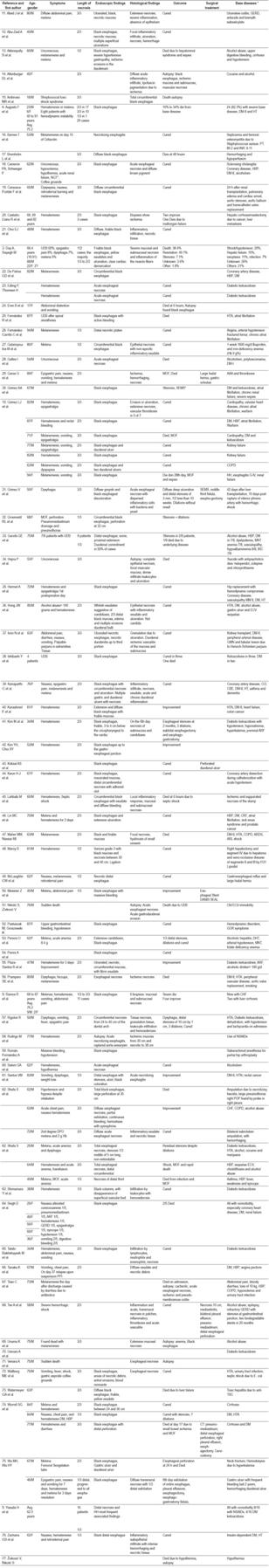
AAA: abdominal aortic aneurysm; NSAIDs: non-steroidal anti-inflammatory drugs; DHT: dehydration; DM: diabetes mellitus; DM-I: type I diabetes mellitus; DM-II: diabetes mellitus type II; MNT: malnutrition; CBE: cerebrovascular event; COPD: chronic obstructive pulmonary disease; GERD: gastroesophageal reflux disease; MOF: multi-organ failure; GMN: glomerulonephritis; HH: hiatal hernia; HT: arterial hypertension; UDB: upper digestive bleeding; CHF: congestive heart failure; ARF: acute renal failure; CRI: chronic renal failure; MM II: lower limbs; ARDS: acute respiratory distress syndrome; NGT: nasogastric tube; CT scan: computerized axial tomography; TB: tuberculosis; SEMS: Self-expanding metallic stent
As can be seen, our patients were older adults who were hospitalized and whose main indication was upper gastrointestinal bleeding (4/5). Active bleeding was confirmed in three cases, as were the total cases (Table 1). Other less frequent findings included dysphagia, shock, anemia, unconsciousness and sudden death. In our series, one patient was diagnosed incidental during study of complicated bile duct pathology.
Diagnosis of AEN is essentially endoscopic although it is occasionally made during emergency surgery or autopsies (Table 1). 1,2,4 The lesion lesions of four of the five cases were circumferential, and four cases had zones of necrosis. Necrosis was diffuse in cases 3 and 4, located in the distal two thirds of the esophagus in cases 1 and 2, and in the middle third of the esophagus in case 5. Seventy-three percent of the cases had two thirds of more the esophagus compromised (Table 1). The appearance of AEN is similar to caustic esophagitis which was suspected in one of our cases. It was clinically ruled out by the patient and family members who also demonstrated that he had already presented two episodes of bleeding as a result of a giant hiatal hernia and Cameron’s ulcerations.
Endoscopic findings are diverse, so diagnosis requires that other etiologies that produce similar alterations be discarded. These include ingestion of caustics, other toxics or carbon; infections; radiation therapy and metastatic melanoma.3,10 Findings can range from whitish membranes, which when removed leave a grayish or blackish mucous membrane, to diffuse necrosis with adherent yellowish exudates. The majority of cases feature ulceration and blackish or grayish appearance demarcated by the gastroesophageal junction, with the cardiac region having its usual appearance. Our cases fit this description. The spectrum of associated lesions is wide and includes gastric hemorrhages, duodenal hemorrhages, ulcerations and perforations. In the general case series there are ten cases of duodenal ulcers (4%), two cases of gastric ulcers (1%), two cases of duodenal ischemic necrosis (1%), four cases of active bleeding (2%), three cases of esophageal perforations (1.3%) and one case of duodenal perforation (0.5%)(Table 1).
Outcomes varied greatly. It was favorable for the second of our patients whose esophageal mucosa had normalized by the one month follow-up examination. Our third patient remained asymptomatic for ten weeks and then refused additional follow-ups. Nevertheless, we do not know how our other three patients evolved. In the general series, mortality reached 32% while 38% were cured. Partial resolution was achieved for the rest of the cases (Table 1). This included residual stenosis which was resolved in two thirds of the patients through dilations but required surgical treatment in 4% of these cases.
Associated comorbidity is a common finding in most cases in the literature. AEN occurs in high-risk patients. Risk is determined by the age of presentation, acute and chronic debilitating diseases, hemodynamic compromise and multiorgan dysfunction (Table 1). Also present in our patients were hyponatremia, hypochloremia and prerenal acute renal failure in Case 1; a giant hiatal hernia of 9 cm and severe gastroesophageal reflux disease with a history of bleeding in Case 2; baseline pneumonia, severe thrombocytopenia, exacerbated chronic renal failure and choledocholithiasis with obstruction of the bile duct in Case 3; and mesenteric thrombosis in Case 4. Table 1 shows comorbidity in the overall series. There were acute and severe diseases in 78% of 157 patients. The remaining 104 patients who are detailed had hemorrhaging, shock, arterial hypertension, heart disease, liver failure, diabetic ketoacidosis, renal failure, septicemia and alcoholism with more than one pathology in the majority of patients.
Histopathology and etiology
In Case 2, biopsies of the distal esophagus showed acute esophagitis with extensive mucosal and submucosal necrosis with a viable muscle layer and reactive epithelial changes. Histological findings are obtained in only a few cases, 15% of the overall series, either in biopsies taken during diagnostic endoscopy, from a surgical piece, or at autopsy. 3,10 Histological findings in the overall series demonstrate compromise of the submucosa and muscularis propria, deep compromise of the esophageal wall, necrosis in almost all cases, inflammation, thrombosis and ischemia not only of the esophagus, but also of the stomach and duodenum (Table 1).
The severity and depth of lesions were demonstrated by clinical evolution and associated complications such as esophageal perforations, mediastinal infection, abscesses, fistulas and esophageal stenoses. These resolved in only 40% of cases despite the dilations (Table 1). Of course, the mortality rate of 32% is high.
Based on the reported cases and the literature reviewed, the etiology is believed to be associated with hypoperfusion within the esophageal mucosa caused by decreased blood flow of various arterial branches. This gives rise to ischemia that leads to necrosis. Decreased blood flow is associated hemodynamic and electrolyte imbalances, hypersensitivity to medications such as antibiotics and NSAIDs, alcoholism, acid reflux, and to underlying diseases which can alter sensitivity and microvasculature. 3,7,14 This is corroborated by associated comorbidities and frequent multiorgan and hemodynamic compromise aggravated by digestive bleeding that leads the patient to consult a physician (Table 1). In addition, findings of ischemia and thrombosis in histopathological studies favor this hypothesis. There are no experimental studies that prove these hypotheses.
Prognosis
Patients’ prognoses depend on the severity of compromise of the patient’s general health status and on the patient’s age. In a group of patients who died, four did so in the first six hours, two died two days after admission, and there were six cases of sudden death or people found unconscious. The extension of necrosis seems to be related to fatal outcomes, since only two patients with a third or half of the esophagus compromised died, while the remaining 29 deaths occurred in people with two thirds or more of the esophagus compromised. The underlying disease was responsible for mortality in a large number of patients, and the authors described it as the main cause in 22 patients.
Risk factors include advanced age, male gender, extension of necrosis and associated comorbidities including hemorrhages, shock, sepsis, hypertension, heart disease, liver failure, kidney failure, diabetic ketoacidosis and alcoholism.
Treatment
The authors are emphatic and unanimous in stating that there is no specific treatment for necrotizing esophagitis in the absence of a defined etiology. Its association with multiple entities can lead to this situation. Interactions with associated comorbidities enhances the danger of esophageal injury with ischemia, thrombosis and necrosis of the mucosa and the esophageal wall. For these reasons, general support measures are recommended for management of the underlying diseases that trigger hypoperfusion (shock, sepsis, heart, kidney and liver failure and multiorgan failure). One key goal is to restore hemodynamic, acid-base and metabolic equilibrium. In cases of anemia, transfusions of packed red blood cells should be administered. Proton pump inhibitors can be administered intravenously to control associated acid-peptic lesions and aggravation of these lesions.3,7-11,14 Stents can even be used to manage profuse active bleeding. In one case reported, this was used as a rescue method. 54 Naturally, the management of relevant medical and surgical complications such as superinfection, perforations and fistulas is important as are dilating stenoses and stenting in cases of poor response.34,35,72 Even esophagectomies can be considered for patients with serious complications (Table 1).3,6-11,14,35,45,78,79.
Conclusions
Necrotizing esophagitis is a rare and severe esophageal disorder with high mortality and complication rates. The high comorbidity that accompanies it is, apparently, the trigger and cause of mortality for a large group. Comorbidity, together with advanced age, male gender and the extent of necrosis are important risk factors. The therapeutic approach must therefore be interdisciplinary and must aim at restoring the hemodynamic, acid-base, metabolic and acid-peptic equilibriums while managing infectious complications. Serious complications occur frequently and require close evaluation and timely management due to the risk to the patient’s life.
REFERENCES
1. Brennan JL. Case of extensive necrosis of the oesophageal mucosa following hypothermia. J Clin Pathol. 1967;20:581-4. doi: 10.1136/jcp.20.4.581. [ Links ]
2. Lee KR, Shark E, Shaw FE. Esophageal infarction complicating spontaneous rupture of the thoracic aorta. JAMA. 1977;237:1233-4. doi: 10.1001/jama.237.12.1233. [ Links ]
3. Day A, Sayegh M. Acute oesophageal necrosis: a case report and review of the literature. Int J Surg. 2010;8(1):6-14. doi: 10.1016/j.ijsu.2009.09.014. [ Links ]
4. Postlethwait RW, Musser AW. Changes in the esophagus in 1,000 autopsy specimens. J Thorac Cardiovasc Surg. 1974;68:953-6 (Abstract). [ Links ]
5. Etienne JP, Roge J, Delavierre P, Veyssier P. Esophageal necrosis of vascular origin. Sem Hop. 1969;45:1599-606 (Abstract). [ Links ]
6. Jacobsen NO, Christiansen J, Kruse A. Incidence of oesophageal necrosis in an autopsy material. Brief report. APMIS. 2003;111(5):591-4. doi: 10.1034/j.1600-0463.2003.1110509.x. [ Links ]
7. Gurvits GE. Black esophagus: Acute esophageal necrosis syndrome. World J Gastroenterol. 2010;26:3219-25. doi: 10.3748/wjg.v16.i26.3219. [ Links ]
8. Grudell ABM, Mueller PS, Viggiano TR. Black esophagus: report of six cases and review of the literature, 1963-2003. Dis Esophagus. 2006;19:105-10. doi: 10.1111/j.1442-2050.2006.00549.x. [ Links ]
9. Ramos R, Mascarenhas J, Duarte P, Vicente C, Casteleiro C. Esofagitis necrosante aguda: análisis retrospectivo. Rev Esp Enferm Dig (Madrid). 2008;100(9):583-5. doi: 10.4321/S1130-01082008000900010. [ Links ]
10. Gómez LJ, Barrio J, Atienza R, Fernández-Orcajo P, Mata L, Saracíbar E, et al. Esofagitis necrotizante aguda. Una patología poco conocida. Rev Esp Enferm Dig (Madrid). 2008;100(11):701-5. [ Links ]
11. Yasuda H, Yamada M, Endo Y, Inoue K, Yoshiba M. Acute necrotizing esophagitis: Role of nonsteroidal anti-inflammatory drugs. J Gastroenterol. 2006;41:193. (Abstract). doi: 10.1007/s00535-005-1741-6. [ Links ]
12. Ángel LA, Boada D, Villalba MP. Evolución epidemiológica de la enfermedad ácido péptica en un Centro de endoscopia diagnóstica de Bogotá entre 1993 y 2007. Rev Col Gastroenterol. 2010;25(2):139-53. [ Links ]
13. Augusto F, Fernandes V, Cremers MI, Oliveira AP, Lobato C, Alves AL, et al. Acute necrotizing esophagitis: A large retrospective case series. Endoscopy. 2004;36:411-5. doi: 10.1055/s-2004-814318. [ Links ]
14. Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: a rare syndrome. J Gastroenterol. 2007;42:29-38. doi: 10.1007/s00535-006-1974-z. [ Links ]
15. Abed J, Mankal P, Judeh H, Kim S. Acute Esophageal Necrosis: A Case of Black Esophagus Associated with Bismuth Subsalicylate Ingestion. ACG Case Rep J. 2014;1(3):131-3. doi: 10.14309/crj.2014.27. [ Links ]
16. Abu-Zaid A, Solimanie S, Abudan Z, Al-Hussaini H, Azzam A, Amin T. Acute esophageal necrosis (black esophagus) in a 40-year-old man. Ann Saudi Med. 2015;35(1):80-1. doi: 10.5144/0256-4947.2015.80. [ Links ]
17. Akkinepally S, Poreddy V, Moreno A. Black esophagus. Cleve Clin J Med. 2009;76(7):400. doi: 10.3949/ccjm.76a.08102. [ Links ]
18. Altenburger DL, Wagner AS, Li S, Garavaglia J. A Case of Black Esophagus With Histopathologic Description and Characterization. Arch Pathol Lab Med. 2011;135:797-8. [ Links ]
19. Ambrosio MR, Rocca BJ, Mastrogiulio MG, Lutfi A, Lazzi S, Tripodi SA. A case of acute esophageal necrosis (black esophagus) in a young man with Down syndrome. Esophagus. 2014;11(2):136. (Abstract). doi: 10.1007/s10388-013-0396-2. [ Links ]
20. Barnes T, Yan S, Kaakeh Y. Necrotizing Esophagitis and Bleeding Associated With Cefazolin. Pharmacother. 2014;48(9):1214-8. (Abstract). doi: 10.1177/1060028014537038. [ Links ]
21. Bremholm L, Winkel R, Born P, Suku ML. Acute esophageal necrosis. Ugeskr Laeger. 2009;171(45):3282-3. (Abstract). [ Links ]
22. Cameron PA, Schweiger F. Forsaken Foregut: Case Report of Simultaneous Black Esophagus and Ischemic Cholangiopathy. Case Reports in Medicine, Published 24 April 2017. doi: 10.1155/2017/8362613. [ Links ]
23. Caravaca-Fontán F, Jimenez S, Fernández-Rodríguez A, Marcén R, Quereda C. Black esophagus in the early kidney post-transplant period. Clin Kidney J. 2014;7:613-4. doi: 10.1093/ckj/sfu094. [ Links ]
24. Casta-o-Llano R, Matar-Khalil O, Cárdenas-Vásquez A, Ruiz M, Juliao F, Sanín E et al. El esófago negro: ¿Patología infrecuente o desconocida? Rev Colomb Gastroenterol. 2006;21(1):62-7. [ Links ]
25. Choi EJ, Lee SH, Lee SH. A case of acute necrotizing esophagitis. Korean J Gastroenterol. 2010;56(6):373-6. (Abstract). doi: 10.4166/kjg.2010.56.6.373. [ Links ]
26. De Palma GD, Persico M, Forestieri P. A case of coffee-ground emesis in an elderly patient. Clin Case Rep. 2014;2(1):18. doi: 10.1002/ccr3.45. [ Links ]
27. Edling P, Thomsen H. Acute oesophageal necrosis in patients with diabetic ketoacidosis. Ugeskr Laeger. 2013;175(48A) (Abstract). [ Links ]
28. Eren B, Turkmen N, Fedakar R. Black esophagus: a rare autopsy case. Bratisl Lek Listy. 2010;111(7):414-5 (Abstract). [ Links ]
29. Fernández R, Álvarez L, Puertas F, González A, García V, López V. Black esophagus (acute esophageal necrosis) after spinal anesthesia. Rev Esp Anestesiol Reanim. 2014;61(7):401-3. doi: 10.1016/j.redar.2013.06.001. [ Links ]
30. Fernández-Carrillo C, Barrios-Peinado C, Pons-Renedo F. Acute necrotizing esophagitis in a patient with femur fracture. Rev Esp Enferm Dig (Madrid). 2011;103(8):436-7. doi: 10.4321/S1130-01082011000800012. [ Links ]
31. Galanopoulos M, Anastasiadis S, Archavlis E, Mantzaris GJ. Black esophagus: an uncommon cause of upper gastrointestinal bleeding. Intern Emerg Med. 2015;11(7):1019-20. doi: 10.1007/s11739-015-1360-z. [ Links ]
32. Galtés I, Gallego MA, Esgueva R, Martin-Fumadó C. Necrosis esofágica aguda (esófago negro). Rev Esp Enferm Dig (Madrid). 2016;108(3):154-5. [ Links ]
33. Garas G, Wou C, Sawyer J, Amygdalos I, Gould S. Acute oesophageal necrosis syndrome. BMJ Case Reports. 2011. doi:10.1136/bcr.10.2010.3423. [ Links ]
34. Gómez ÁA, Guerrero D, Hani AC, Caadas R. Acute necrotizing esophagitis (black esophagus) with secondary severe stenosis. Rev Gastroenterol Peru. 2015;35(4):349-54 (Abstract). [ Links ]
35. Gómez V, Propst JA, Francis DL, Canabal JM, Franco PM. Black esophagus: an unexpected complication in an orthotopic liver transplant patient with hemorrhagic shock. Dig Dis Sci. 2014;59(10):2597-9. doi: 10.1007/s10620-014-3176-5. [ Links ]
36. Groenveld RL, Bijlsma A, Steenvoorde P, Ozdemir A. A black perforated esophagus treated with surgery: Report of a case. World J Gastrointest Surg. 2013;5(6):199-201. doi: 10.4240/wjgs.v5.i6.199. [ Links ]
37. Gurvits GE, Cherian K, Shami MN, Korabathina R, El-Nader EM, Rayapudi K, et al. Black esophagus: new insights and multicenter international experience in 2014. Dig Dis Sci. 2015;60(2):444-53 (Abstract). doi: 10.1007/s10620-014-3382-1. [ Links ]
38. Hejna P, Ublová M, Voříšek V. Black esophagus: acute esophageal necrosis in fatal haloperidol intoxication. J Forensic Sci. 2013;58(5):1367-9 (Abstract). doi: 10.1111/1556-4029.12151. [ Links ]
39. Hermet A, Lidove O, Grimbert S, Zeller V, Ducroquet F, Ziza JM. Black esophagus. Rev Med Int. 2014;35(6):393-5 (Abstract). doi: 10.1016/j.revmed.2013.06.006. [ Links ]
40. Hong JW, Kim SU, Park HN, Seo JH, Lee YC, Kim H. Black esophagus associated with alcohol abuse. Gut Liver. 2008;2(2):133-5. doi: 10.5009/gnl.2008.2.2.133. [ Links ]
41. Iorio N, Bernstein GR, Malik Z, Schey R. Acute Esophageal Necrosis Presenting With HenochSchönlein Purpura. ACG Case Rep J. 2015;3(1):17-9. doi: 10.14309/crj.2015.87. [ Links ]
42. Ishibashi Y, Matsuzono E, Goda T, Yokoyama F, Sugai N, Seki H, et al. Black esophagus due to acute necrotizing esophagitis: four case reports. Nihon Shokakibyo Gakkai Zasshi. 2011;108(5):759-8 (Abstract). [ Links ]
43. Kanaparthi C, Singhal S, Guillaume C, Sharma S, Anand S. Acute gastrointestinal necrosis: “black esophagus” or “black gut”. Trop Gastroenterol. 2011;32(4):323-6. [ Links ]
44. Karaahmet F, Hamamci M, Coban S, Yuksel I. A rare entity with coffee-ground vomit in elderly adults: black esophagus. J Am Geriatr Soc. 2014;62(8):1610-1. doi: 10.1111/jgs.12952. [ Links ]
45. Kim IK, Kim JS, Song IS. A Case of Acute Esophageal Necrosis with Gastric Outlet Obstruction. Korean J Gastroenterol. 2010;56:314-8. doi: 10.4166/kjg.2010.56.5.314. [ Links ]
46. Kim YH, Choi SY. Black esophagus with concomitant candidiasis developed after diabetic ketoacidosis. World J Gastroenterol. 2007;13(42):5662-3. doi: 10.3748/wjg.v13.i42.5662. [ Links ]
47. Köksal AS, Eminler AT, Parlak E, Uslan MI, Cücen E. Black esophagus and duodenal perforation: more than an incidental association. Acta Gastroenterol Belg. 2015;78(2):253-4 (Abstract). [ Links ]
48. Kwon HJ, Park SH, Ahn JH, Lee TH, Lee CK. Acute esophageal necrosis occurring in a patient undergoing percutaneous coronary intervention. Korean J Intern Med. 2014;29:379-82. doi: 10.3904/kjim.2014.29.3.379. [ Links ]
49. Lahbabi M, Ibrahimi A, Aqodad N. Acute esophageal necrosis: a case report and review. Pan Afr Med J. 2013;14:109. doi:10.11604/pamj.2013.14.109.2000. [ Links ]
50. Lin MC, Chu HC, Chen PJ. Clinical picture: Black oesophagus. QJM. 2015;108(10):839-40. doi: 10.1093/qjmed/hcv075. [ Links ]
51. Maher MM, Nassar MI. Black esophagus: a case report. Cases J. 2008;1:367. doi: 10.1186/1757-1626-1-367. [ Links ]
52. Maroy B. Black esophagus complicating variceal bleeding. Endoscopy. 2013;45(Suppl 2):E237. doi: 10.1055/s-0030-1256630. [ Links ]
53. McLaughlin CW, Person TD, Denlinger CE, Charleston SC. Management of acute esophageal necrosis syndrome. J Thorac Cardiovasc Surg. 2011;141:e23-e24. doi: 10.1016/j.jtcvs.2010.12.001. [ Links ]
54. Messner Z, Gschwantler M. Use of the Ella Danis stent in severe esophageal bleeding caused by acute necrotizing esophagitis. Endoscopy 2014;46:E225-6. doi: 10.1055/s-0034-1365384. [ Links ]
55. Nikolić S, Zivković V. Black esophagus--case report. Srp Arh Celok Lek. 2014;142(1-2):94-8 (Abstract). doi: 10.2298/SARH1402094N. [ Links ]
56. Pastuszak M, Groszewski K. Endoscopic image of “black esophagus”--case report. Pol Merkur Lekarski. 2009;26(155):468-71 (Abstract). [ Links ]
57. Pereira O, Figueira-Coelho J, Picado B, Neves-Costa J. Black Oesophagus. BMJ Case Rep. 2013. doi: 10.1136/bcr-2012-008188. [ Links ]
58. Pierini A, Imhof H, Burlando E, Gianinetti L, Pierini L. Acute necrotizing esophagitis. Case report. Acta Gastroenterol Latinoam. 2013;43(2):130-2 (Abstract). [ Links ]
59. Plaza-Santos R, Froilán-Torres C, Castro-Carbajo P, Martín-Chavarri S, Gea-Rodríguez F, Suárez de Parga JM. Esofagitis aguda necrosante asociada a coma diabético hiperosmolar. J Gastrohep. 2009;32(4):322-3. doi: 10.1016/j.gastrohep.2008.09.026. [ Links ]
60. Pramparo SE, Ruiz PM, Flores-Valencia R, Rodeyro J. Esofagitis necrotizante aguda: una entidad inusual. Medicina (Buenos Aires). 2010;70:524-6. [ Links ]
61. Rigolon R, Fossà I, Rodella L, Targher G. Black esophagus syndrome associated with diabetic ketoacidosis. World J Clin Cases. 2016;4(2):56-9. doi: 10.12998/wjcc.v4.i2.56. [ Links ]
62. Rodrigo M, Gorraiz BE, Merino C, Eguaras J, Elizalde JM, Soler W. Acute necrotizing esophagitis in an unstable patient. An Sist Sanit Navar. 2009;32(1):113-6. [ Links ]
63. Román-Fernández A, López-Álvarez A, Fossati-Puertas S, Areán-González I, Varela-García O, Via-o-López PM. Black esophagus (acute esophageal necrosis) after spinal anesthesia. Rev Esp Anestesiol Reanim. 2014;61(7):401-3. doi: 10.1016/j.redar.2013.06.001. [ Links ]
64. Salem GA, Ahluwalia S, Guild RT. A case of acute oesophageal necrosis (AEN) in a hypothermic patient. The grave prognosis of the black oesophagus. Arab J Gastroenterol. 2015;16(3-4):136-8 (Abstract). doi: 10.1016/j.ajg.2015.05.002. [ Links ]
65. Santos VM, Villaça RB, Gouvêa IP, Sá DAR. Comentario a la nota clínica: Esofagitis necrotizante aguda en paciente inestable. An Sist Sanit Navar. 2009;32(3):439-42. [ Links ]
66. Shafa S, Sharma N, Keshishian J, Dellon ES. The Black Esophagus: A Rare But Deadly Disease. ACG Case Rep J. 2016;3(2):88-91. doi: 10.14309/crj.2016.9. [ Links ]
67. Shimamura Y, Nakamura K, Ego M, Omata F. advanced endoscopic imaging of black esophagus. Can J Gastroenterol Hepatol. 2014;28(9):471-2. doi: 10.1155/2014/620709. [ Links ]
68. Singh D, Singh R, Laya AS. Acute esophageal necrosis: a case series of five patients presenting with “Black esophagus”. Indian J Gastroenterol. 2011;30(1):41-5 (Abstract). doi: 10.1007/s12664-011-0082-z. [ Links ]
69. Talebi-Bakhshayesh M, Samiee-rad F, Zohrenia H, Zargar A. Acute Esophageal Necrosis: A Case of Black Esophagus with DKA. Arch Iran Med. 2015;18(6):384-5. [ Links ]
70. Tanaka K, Toyoda H, Hamada Y, Aoki M, Kosaka R, Noda T, et al. Relapse of acute necrotizing esophagitis. Endoscopy. 2007;39:E305. doi: 10.1055/s-2007-966789. [ Links ]
71. Tsao C, Thomas L, McGoey RR. Black esophagus detected at autopsy in a patient with abdominal pain and bloody diarrhea. Diagnosis: Acute esophageal necrosis, ischemic and pseudomembranous colitis. J La State Med Soc. 2014;166(4):188-190 (Abstract). [ Links ]
72. Tse A, Basu S, Ali H, Hamouda A. Black necrotic oesophagus following the use of biodegradable stent for benign oesophageal stricture. J Surg Case Rep. 2015;7:1-3. doi: 10.1093/jscr/rjv072. [ Links ]
73. Unuma K, Harada K, Funakoshi T, Uemura K. Sudden death of an alcoholic elderly man with acute esophageal necrosis (black esophagus). Forensic Sci Int. 2011;212(1-3):e15-7 (Abstract). doi: 10.1016/j.forsciint.2011.05.024. [ Links ]
74. Usmani A, Samarany S, Nardino R, Shaib W. Black esophagus in a patient with diabetic ketoacidosis. Conn Med. 2011;75(8):467-8. [ Links ]
75. Venara A, Pavageau AH, Maillart CR, Jousset N. Sudden death due to black esophagus: a case report. Am J Forensic Med Pathol. 2013;34(1):16-7 (Abstract). doi: 10.1097/PAF.0b013e3182717b98. [ Links ]
76. Wallberg ME, Young P, Finn BC, Thomé M, Chueco AA, Villarejo F. Esófago negro secundario a esofagitis necrotizante aguda. Reporte de un caso clínico. Rev Med Chile. 2009;137:672-4. doi: 10.4067/S0034-98872009000500011. [ Links ]
77. Watermeyer GA, Shaw JM, Krige JEJ. Gastrointestinal: Acute necrotizing esophagitis. J Gastroenterol Hepatol 2007;22:1162. doi: 10.1111/j.1440-1746.2007.05013.x. [ Links ]
78. Worrell SG, Oh DS, Greene CL, DeMeester SR, Hagen JA. Acute Esophageal Necrosis: A Case Series and Long-Term Follow-Up. Ann Thorac Surg. 2014;98:341-2. doi: 10.1016/j.athoracsur.2013.09.023. [ Links ]
79. Wu MH, Wu HY. Incremental change in acute esophageal necrosis: report of two cases. Surg Today. 2014;44(2):363-5. doi: 10.1007/s00595-013-0526-4. [ Links ]
80. Zacharia GS, Sandesh K, Ramachandran TM. Acute Esophageal Necrosis: An Uncommon Cause of Hematemesis. Oman Med J. 2014;29(4):302-4. doi: 10.5001/omj.2014.79. [ Links ]
81. Zivković V, Nikolić S. The unusual appearance of black esophagus in a case of fatal hypothermia: a possible underlying mechanism. Forensic Sci Med Pathol 2013;9(4):613-4 (No abstract). doi: 10.1007/s12024-013-9445-3. [ Links ]
Received: October 13, 2017; Accepted: July 26, 2018











 texto en
texto en