Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.3 Bogotá jul./set. 2018
https://doi.org/10.22516/25007440.283
Case report
Diagnosis of helminthiasis by endoscopic videocapsule
1Gastroenterólogo Clínico Quirúrgico. Coordinador, Programa de Posgrado en Gastroenterología Clínico-Quirúrgica, Universidad de Caldas, Manizales, Colombia
2Medicina Interna. Gastroenterología. Docente, Universidad de Caldas, Manizales, Colombia
3Gastroenterólogo Clínico Quirúrgico, Universidad de Caldas, Manizales, Colombia
4Gastroenterólogo Clínico Quirúrgico, Universidad de Caldas, Manizales, Colombia
5Fellow de Gastroenterología Clínico-Quirúrgica, Universidad de Caldas, Manizales, Colombia
Helminthiasis is an intestinal parasitosis that is very prevalent in developing countries but is increasing in developed countries. Taking into account the life cycle of helminths, their presentation is related to high-risk environmental and socioeconomic situations. Endemic presence can be considered a public health problem. Several methods are available for diagnosis including the study of fecal matter, endoscopy and diagnostic imaging such as X-ray studies of the digestive tract, CT scans and magnetic resonance. Recently, there have been reports of diagnosis of helminthiasis by capsule endoscopy which has also allowed the study of the ecology and in situ pathology of these parasites. We present a clinical case of helminthiasis compatible with strongyloidiasis that was diagnosed by endoscopic capsule by the surgical clinical gastroenterology group of the University of Caldas in Manizales, Colombia.
Keywords: Strongyloides stercoralis; helminthiasis; capsular endoscopy
La helmintiasis corresponde a una parasitosis intestinal altamente prevalente en países en desarrollo, y que viene aumentando en los países desarrollados. Teniendo en cuenta el ciclo de vida de los helmintos, su presentación se relaciona con situaciones ambientales y socioeconómicas de alto riesgo. Por tanto, su presencia endémica puede considerarse un problema de salud pública. Para el diagnóstico, se disponen de varios elementos que incluyen el estudio de la materia fecal, la endoscopia y las imágenes diagnósticas como los estudios de rayos X de vías digestivas, la tomografía axial computarizada (TAC) y la resonancia magnética (RM). En la actualidad, existen reportes de diagnóstico de helmintiasis por cápsula endoscópica que también han permitido el estudio de la ecología y de la patología in situ de estos parásitos. Se presenta un caso clínico de helmintiasis compatible con estrongiloidosis, diagnosticado por cápsula endoscópica por el Grupo de Gastroenterología Clínico-Quirúrgica de la Universidad de Caldas, Colombia.
Palabras clave: Strongyloides stercoralis; helmintiasis; endoscopía capsular
Introduction
The helminths are organisms that are present in developing countries, especially in those with poor health conditions. Nevertheless, they are also found in non-endemic countries that have migrants from areas where they normally occur. They are among the most widely distributed infectious agents in humans and especially attack marginal, low-income and resource- scarce regions. Currently, it is estimated that more than 1 million people in developing countries are infected by at least one type of helminth. These parasites cause morbidity that includes iron deficiency anemia, seizures, portal hypertension, chronic diarrhea and chronic abdominal pain. 3 It is well known that the morbidity produced by these parasites leads to a vicious circle of poverty, low productivity and inadequate socioeconomic development. 1,2
Helminths are multicellular worms which cannot multiply in the human body in their adult form. Consequently, they are usually transmitted by contact with infected feces or through contaminated soil, food or water. They measure between one mm and several meters depending on the species and live in the the small intestine or the colon where they are nourished by the endoluminal content or by blood from the intestinal wall. In Colombia, there are no recent data on prevelance, but the National Intestinal Parasitism Survey of 1980 reported 33.6% for Ascaris lumbricoides, 37.5% for Trichuris trichiura and 23% for Uncinaria stenocephala in the general population. In the Colombian Amazon, very high prevalences of geohelminths were demonstrated in children aged 2 to 16 years. The most frequent was Strongyloides stercoralis at 49.3%. 4,5. Because of globalization, helminths have increased their prevalence in developed countries such as the United States, Japan and some European countries 6,7.
The Centers for Disease Control and Prevention (CDC) have established the following tests for diagnosis of parasitosis: fecal examination, endoscopy, serological tests and imaging tests including x-rays, magnetic resonance imaging (MRI) and computed axial tomography (CAT). 8
The endoscopic capsule was first reported in 2000, approved by the FDA in 2001, and established as a non-invasive method for the study of the small intestine. Currently. digestive bleeding of unknown origin is the most important indication for usage. It also allows evaluation of the entirety of the small intestine, provides high resolution images, and does not require sedation, surgery or exposure to radiation. 9,10 The system consists of three fundamental elements: the capsule, a data recorder and a workstation. The capsule contains an optical dome, lens, light source, battery, transmitter and an antenna. The viewing angle goes from 140° to 170° with 8X magnification.
This article presents a case of helminthiasis diagnosed by means of an endoscopic capsule by the Clinical-Surgical Gastroenterology group of the University of Caldas, Colombia.
Clinical case
The patient was an 18-year-old man with a clinical history of two years of intermittent episodes of generalized colicky abdominal pain sometimes associated with diarrhea without blood. These episodes resolved spontaneously, but because he was a patient who frequented rural areas of the Colombian tropics, he received empirical anti-parasite treatments including albendazole, nitazoxanide and secnidazole. The only important antecedent was familial dyslipidemia, manifested by hypertriglyceridemia, for which he takes gemfibrozil.
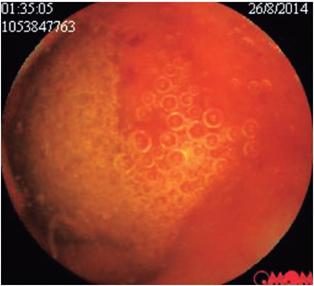
The patient’s abdominal pain became exacerbated, especially in the epigastric area. This time it was associated with diarrhea, vomiting and fever which required admission to the emergency department of a third level institution. Results of multiple tests performed upon admission showed normal levels of serum lipase, amylase and serum electrolytes. Total abdominal ultrasound was within normal limits. Upper digestive endoscopy found antral follicular gastritis. Stool tests were negative for intestinal parasites but inconclusive for infections although the stool culture was negative. A CT scan of the abdomen was within normal limits. The initial blood tests showed a leukocyte count of 17,210 with 30.9% neutrophils and 43.9% eosinophils. The hemoglobin count was 14.3 g/dL while hematocrit was 48.1%. Given the findings of eosinophilia and leukocytosis, it was decided to supplement the study with a thick-film test which was negative. A left colonoscopy showed no evidence of lesions but samples were taken from the sigmoid colon and rectum. The pathology results showed indeterminate colitis and chronic proctitis. Another set of blood tests showed that the leukocyte level was 19,350 with 24.9% neutrophils and 59% eosinophils and a hemoglobin level of 14.5 g/dL with hematocrit of 42.6%. Bone marrow aspirate showed evidence of eosinophilia with adequately matured cells and hypercellular bone marrow with eosinophilic hyperplasia. Final in-hospital blood tests reported a leukocyte count of 17,500 with 15% neutrophils, 64.5% eosinophils, hemoglobin at 15 g/dL and hematocrit at 43.8%. The possibility of hypereosinophilic syndrome was considered, although this diagnosis requires a not-yet-identified target organ. As a second possibility, eosinophilic leukemia was considered. The patient achieved adequate control of abdominal pain and was discharged for outpatient follow-up and blood tests. Management was begun with a short cycle of steroids and a complementary endoscopic capsule and other hematological studies were ordered. The finding of the endoscopic capsule was conclusive as it showed evidence of erosions (Figure 1) and a large ulcer covered with fibrin in the jejunum (Figure 2). Later, multiple small intestinal parasites were seen adhering to the intestinal wall with one portion that was white and another portion that was transparent (Figures 3 and 4). Treatment was begun with Irvermectin a single 200 mcg/kg dose of Irvermectin which was repeated 15 days later. In addition, the patient was given 400 mg of oral albendazole every 12 hours for 10 days. The patient managed to control his episodes of abdominal pain, and is now asymptomatic.
Discussion
Although it is not one of the methods recommended by the CDC for diagnosis of parasites, an endoscopic video capsule can be used for this purpose. In 2003, Soares and colleagues were the first to describe its use for the in-vivo viewing of parasites, in that case, A. lumbricoides. 11 The endoscopic capsule can not only be used to assess the presence of parasites but can also be used to assess the ecology and pathology in relation to the parasitosis. Similarly, it can play an important role in evaluating the effectiveness of treatments aimed at eliminating parasites.12,13 The main limitations of endoscopic capsules are that they cannot be used for any therapeutic measures and their high cost with respect to other available modalities. They also depends on peristalsis to advance through the gastrointestinal tract. This leads inability to see many areas of the mucosal surface, although this problem is currently being resolved as capsules that allow 360 ° rotation of the lens for complete evaluation are becoming available.2,14
In the case presented here, identification of macroscopic characteristics of the parasite plus local pathological findings and clinical manifestations of the patient allowed us to diagnose infestation by S. stercoralis which is an almost transparent parasite. It measures between 2.2 and 2.5 mm, has a diameter of 50 μm, and lives in tunnels between the enterocytes of the small intestine of the host. All of this matched observations in our case. 15 The classical fecal examination for parasites has a very low yield in detection of S. stercoralis (less than 30%). For this reason, smears and stains with Lugol’s iodine or Auramine-phenol stain are used. Periodic examination of feces is recommended for improving the diagnostic yield, although there are other diagnostic techniques that are not generally performed routinely in the laboratories of the centers that provide health services. These include funnel tests, culturing on agar plates and the filter paper method. The patient received treatment with two doses of one mg/kg of ivermectin plus 200 mg of oral albendazole every 12 hours for 10 days. To date, the patient remains free of symptoms. 15
There are only few cases in the literature about diagnosis of parasitosis by means of capsule endoscopy, but with increasing use of this method, its use for this purpose will undoubtedly become more common and better known. 12,16
Referencias
1. Hotez PJ, Molyneux DH, Fenwick A, Kumaresan J, Sachs SE, Sachs JD, et al. Control of neglected tropical diseases. N Engl J Med. 2007;357(10):1018-27. doi: 10.1056/NEJMra064142. [ Links ]
2. Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, Jacobson J. Helminth infections: the great neglected tropical diseases. J Clin Invest. 2008;118(4):1311-21. doi: 10.1172/JCI34261. [ Links ]
3. Soga K, Handa O, Yamada M, Sakagamia J, Yagi N, Naito Y, et al. In vivo imaging of intestinal helminths by capsule endoscopy. Parasitol Int. 2014;63(1):221-8. doi: 10.1016/j.parint.2013.09.006. [ Links ]
4. Arciniegas E, Corredor A, Hernández CA. Parasitismo intestinal. Bogotá, Colombia: Instituto Nacional de Salud; 2000. [ Links ]
5. Ordóñez LE, Angulo ES. Desnutrición y su relación con parasitismo intestinal en niños de una población de la Amazonia colombiana. Biomedica. 2002;22(4):486-98. doi: 10.7705/biomedica.v22i4.1175. [ Links ]
6. Dupouy-Camet J, Peduzzi R. Current situation of human diphyllobothriasis in Europe. Euro Surveill. 2004;9(5):31-5. doi: 10.2807/esm.09.05.00467-en. [ Links ]
7. de Marval F, Gottstein B, Weber M, Wicht B. Imported diphyllobothriasis in Switzerland: molecular methods to define a clinical case of Diphyllobothrium infection as Diphyllobothrium dendriticum, August 2010. Euro Surveill. 2013;18(3). pii: 20355. [ Links ]
8. Center for Disease Control and Prevention [Internet]. Diagnosis of Parasitic Diseases. Última actualización: mayo 9 de 2018. Disponible en: Disponible en: http://www.cdc.gov/parasites/references_resources/diagnosis.html . [ Links ]
9. Ladas SD, Triantafyllou K, Spada C, Riccioni ME, Rey JF, Niv Y, et al. European Society of Gastrointestinal Endoscopy (ESGE): recommendations (2009) on clinical use of video capsule endoscopy to investigate small-bowel, esophageal and colonic diseases. Endoscopy. 2010;42(3):220-7. doi: 10.1055/s-0029-1243968. [ Links ]
10. Sidhu R, Sanders DS, Morris AJ, McAlindon ME. Guidelines on small bowel enteroscopy and capsule endoscopy in adults. Gut. 2008;57(1):125-36. doi: 10.1136/gut.2007.129999. [ Links ]
11. Soares J, Lopes L, Villas-Boas G, Pinho C. Ascariasis observed by wireless-capsule endoscopy. Endoscopy. 2003;35(2):194. doi: 10.1055/s-2003-37008. [ Links ]
12. Barnett K, Emder P, Day AS, Selby WS. Tapeworm infestation: a cause of iron deficiency anemia shown by capsule endoscopy. Gastrointest Endosc. 2007;66(3):625-7. doi: 10.1016/j.gie.2006.12.004. [ Links ]
13. Hosoe N, Imaeda H, Okamoto S, Bessho R, Saito R, Ida Y, et al. A case of beef tapeworm (Taenia saginata) infection observed by using video capsule endoscopy and radiography (with videos). Gastrointest Endosc. 2011;74(3):690-1. doi: 10.1016/j.gie.2011.05.011. [ Links ]
14. Awadzi K, Barakat R, Basáñez M, Boatin B, García H, Gazzinelli A, et al. Research Priorities for Helminth Infections. Technical Report of the TDR Disease Reference Group on Helminth Infections. Ginebra, Suiza: World Health Organization; 2012. Disponible en: http://www.who.int/iris/bitstream/10665/75922/1/WHO_ TRS_972_eng.pdf. [ Links ]
15. Farthing M, Fedail S, Savioli L, Bundy D, Krabshuis J. Manejo de la estrongiloidiasis. Milwaukee, Estados Unidos: World Gastroenterology Organisation; 2014. Disponible en: http://www.worldgastroenterology.org/guidelines/global-guidelines/management-of-strongyloidiasis/management-of-strongyloidiasis-spanish. [ Links ]
16. Hosoe N, Ogata H, Hibi T. Endoscopic imaging of parasites in the human digestive tract. Parasitol Int. 2014;63(1):216-20. doi: 10.1016/j.parint.2013.08.003. [ Links ]
Received: August 14, 2017; Accepted: October 30, 2017











 texto en
texto en