Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.4 Bogotá Oct./Dec. 2018
https://doi.org/10.22516/25007440.311
Original articles
Outpatient gastroenterology survey of the beliefs and perceptions of patients with chronic constipation regarding etiology, complications and efficacy of general measures
1Médico General, Universidad Nacional de Colombia. Bogotá D. C., Colombia.
2Profesor titular de Medicina, Coordinador de Gastroenterología, Universidad Nacional de Colombia, Hospital Universitario Nacional. Gastroenterólogo, Clínica Fundadores. Bogotá D. C., Colombia.
3Internista Gastroenteróloga, Universidad Nacional de Colombia. Gastroenteróloga, Clínica Fundadores. Bogotá D. C., Colombia.
Introduction:
Chronic constipation affects 14% of the world’s population. It leads to high costs for health systems due to diverse treatments. Frequently, patients and doctors have erroneous perceptions about constipation’s etiology, complications and treatment.
Materials and methods:
Patients with chronic constipation were surveyed at the outpatient clinic of a gastroenterology service of a university institution. The most frequent erroneous beliefs regarding the condition found among patients diagnosed with constipation were investigated.
Results:
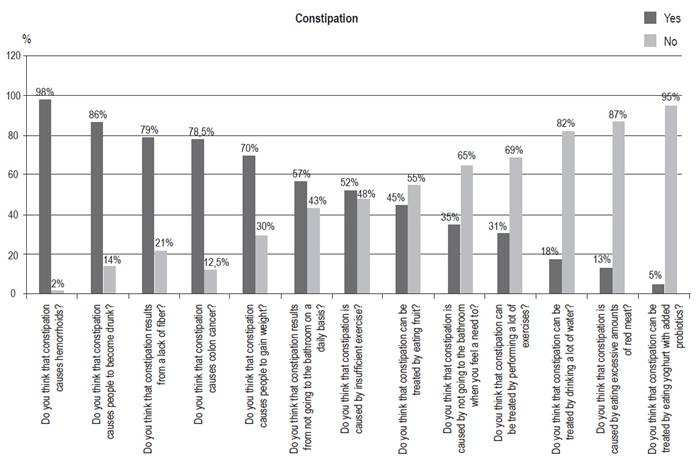
A total of 278 patients who met the inclusion criteria were surveyed. Ninety-eight percent consider that chronic constipation is the cause of hemorrhoids, eighty-six percent believe that it leads to poisoning, and seventy-eight percent believe that it causes colon cancer. Other misconceptions were that low fiber consumption causes constipation (79%) and that low levels of physical activity cause constipation (52%). Fifty-five percent do not consider that high fiber diets (55%) or regular exercise (69%) are useful for treatment. The most frequent observation was abundant consumption of fiber without improvement.
Keywords: Survey; constipation; perceptions; fiber; cancer; hemorrhoids; exercise
Introducción:
el estreñimiento crónico (EC) afecta al 14 % de la población mundial y genera altos costos para los sistemas de salud por los diferentes tratamientos. Con frecuencia, pacientes y médicos tienen percepciones erróneas sobre la etiología, complicaciones y el tratamiento de la entidad con medidas generales.
Materiales y métodos:
se realizó una encuesta a pacientes con EC atendidos en la consulta externa de un servicio de gastroenterología de una institución universitaria. Con interrogantes todos falsos, se investigaron las creencias erróneas más frecuentes en los pacientes con diagnóstico de estreñimiento respecto a su enfermedad.
Resultados:
se encuestaron 278 pacientes que cumplieron con los criterios de inclusión. El 98 % consideró que el EC es la causa de las hemorroides, mismo que produce intoxicación (86 %) y causa cáncer de colon (78 %). Otros conceptos erróneos fueron el bajo consumo de fibra (79 %) como causa de la enfermedad, al igual que la baja actividad física (52 %). No consideran útil para el tratamiento la dieta alta en fibra (55 %) ni realizar ejercicio de forma regular (69 %). La observación más frecuente fue el consumo abundante de fibra sin presentar mejoría.
Palabras clave: Encuesta; estreñimiento; percepciones; fibra; cáncer; hemorroides; ejercicio
Introduction
Globally, chronic constipation affects 14% of all adult patients and 30% of those who are over 60 years old. 1,2 It occurs most frequently in women and institutionalized people, 1,2 is associated with low socioeconomic status and psychiatric illnesses, 1,3 and markedly alters quality of life. 4 In addition, it is expensive for health care systems because of its high prevalence. 3,4 In the United States, it is responsible for 8 million annual outpatient visits at a cost exceeding 230 million dollars. 5 In addition, 1.2 million patients are referred to gastroenterology for this pathology. 4,5 In that country, the annual direct medical care costs for women with chronic constipation are almost double those of women without constipation. 2,5. In the USA, 2.5 million people suffer chronic constipation. If they all underwent colonoscopies, the annual cost would reach 5 billion dollars. 5,6
There are many popular beliefs and myths about the causes of chronic constipation as well as treatment among patients and many doctors. 7 Among these, the most frequently heard are that inadequate consumption of fiber is one cause, that chronic constipation induces colon cancer (and that CC produces food poisoning which can be treated by ingesting large amounts of water). 7,8 Other beliefs about treatment include the idea that it can be relieved by consumption of probiotics, alone or with yogurt, and exercise improves symptoms of constipation.
Taking into account its prevalence, high costs identified in other countries, and the perception in outpatient gastroenterology services that it occurs frequently (although this has not been measured), we decided to carry out this study at the gastroenterology and digestive endoscopy unit of Clínica Fundadores de Bogotá, a third-level institution attached to the graduate program in gastroenterology at the National University of Colombia.
Materials and methods
This study was conducted among patients diagnosed with chronic constipation using the Rome IV criteria at the gastroenterology outpatient clinic of the Clínica Fundadores in Bogotá, Colombia between May and October 2016. 9 Patients were included after being instructed about the nature and purposes of the research and voluntarily deciding to participate in the study as indicated by their signatures on informed consent forms. The information was collected with a survey form designed specifically for this research. It included demographic data and 14 dichotomous questions based on concerns and doubts identified by patients of the gastroenterology clinic. These concerns were identified during the 6 months prior to the study. The form also included space for the survey participants to write any additional comments or beliefs about the disease. The survey was conducted by one of the authors (ADM) during his special internship in the gastroenterology unit. The patients belong to socioeconomic strata 2, 3 and 4.
Results
Of the 278 patients included in the study, 75% were female and the average age was 50 years. All patients had received initial treatment with fiber, specifically, wheat bran and psyllium (30 grams), and home remedies. With those measures, 20% of patients had improved. At the time of the survey, the remaining 80% were receiving 17 g/day of polyethylene glycol 3350 (Contumax®, PEG®) or 5-10 mg/day of sodium picosulfate. These patients reported being satisfied with these last two types of treatment due to the significant improvement of their symptoms. The questions and the frequencies of administration, which are the objectives of this study, are shown in Figure 1.
Discussion
The results of this study show that patients from this Colombian population have many of the beliefs found in similar studies from other countries. 7,8 The most frequent were that chronic constipation is the cause of the hemorrhoids (98%), causes food poisoning (86%) and also causes CC. With regard to the latter, there is no relationship since CC is mainly associated with family history of CC, smoking, alcohol consumption, obesity, diabetes, consumption of processed meats and inflammatory bowel disease. 10 Similarly, there is no definitive evidence that constipation produces hemorrhoids. 7
It is noteworthy that more than half (55%) do not believe that fiber forms like fruit have utility in the diet even though most patients (79%) consider the lack of fiber in the diet to be a cause of constipation. This last assessment is probably the result of not having empirical experience in the use of large amounts of fruit. In fact, research has not yet shown clear benefits from fiber. 11 A recent meta-analysis has found marginal benefits from psyllium, but the studies it looked at had multiple methodological biases and were of poor quality. 12 Although some current management guidelines recommend increasing fiber intake during initial treatment, 13,14,15 the evidence supporting these recommendations is of low quality. 11,12 In addition, insoluble fiber can induce or exacerbate flatulence, and in some people it can worsen constipation. 12,16 Soluble fiber such as psyllium or ispaghula has shown marginal benefits, but in the long term these results have not been maintained. 13,14,15 Despite the evidence published, most physicians continue to believe that fiber and fruit are fundamental for management of chronic constipation.
Fifty-two percent of respondents believe that lack of exercise is an etiological factor of constipation, but, paradoxically, 69% do not believe that performing exercise serves as a treatment. Studies have not shown that regular exercise improves constipation or reduces the need for laxatives. 17,18 A commonsense everyday inference is that, if exercise increased colon transit and favored bowel movements, then high performance athletes could not compete because they would often have diarrhea. Exercise has proven beneficial effects for the cardiovascular system. 19
In relation to the benefit of, Eighty-two percent of respondents said that they did not consider consuming a lot of liquids useful for treating constipation. This assessment is true since there is no evidence to show the benefit of taking a lot of fluids,11,20 except in cases of hospitalized and dehydrated patients. 11 It has been found that probiotics can increase colonic transit, but they have not been shown to relieve constipation in either adults or children.21,22,23 The majority of respondents (85%) do not consider that yogurt with probiotics is useful for treating this entity.
Contrary to popular beliefs, management of chronic constipation is complex due to the heterogeneity of patients who can be classified into the following subgroups: patients with normal colonic transit, patients with slow transit, patients with dysfunction of the pelvic floor (anism, pelvic floor dyssynergia), patients with constipation secondary to opioids which is part of narcotic bowel syndrome, an entity with great morbidity and mortality. 3,9,24,25,26
Pharmacological strategies with proven efficacy include osmotic laxatives such as polyethylene glycol and lactulose, stimulant laxatives such as sodium picosulfate, secretagogues such as linaclotide and lubiprostone, prucalopride which is a universal prokinetic and 5HT4 agonist. 27 Methylnaltrexone and alvimopan can be used to treat constipation secondary to opioids 28.
Conclusions
Most patients mistakenly believe that constipation causes CC and hemorrhoids. The vast majority do not consider consumption of fruit to be a useful treatment for constipation. Patients consider that exercise does not work as a treatment of this disease. According to the results and the scientific evidence, the most frequent assessments given by patients is correct. Even though they attribute low fiber intake and lack of exercise as etiological factors, most did not consider that increasing either of them improves constipation. It is possible that the correct answers of the population studied in regarding to popular beliefs is due to the fact that many of them attend the educational talks that a member of our service (WO) gives about chronic pathologies.
Referencias
1. Suares NC, Ford AC. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(9):1582-91; quiz 1581, 1592. doi: 10.1038/ajg.2011.164. [ Links ]
2. Mugie SM, Benninga MA, Di Lorenzo C. Epidemiology of constipation in children and adults: a systematic review. Best Pract Res Clin Gastroenterol. 2011;25(1):3-18. doi: 10.1016/j.bpg.2010.12.010. [ Links ]
3. Camilleri M, Ford AC, Mawe GM, Dinning PG, Rao SS, Chey WD, et al. Chronic constipation. Nat Rev Dis Primers. 2017;3:17095. doi: 10.1038/nrdp.2017.95. [ Links ]
4. Dennison C, Prasad M, Lloyd A, Bhattacharyya SK, Dhawan R, Coyne K. The health-related quality of life and economic burden of constipation. Pharmacoeconomics. 2005;23(5):461-76. doi: 10.2165/00019053-200523050-00006. [ Links ]
5. Choung RS, Branda ME, Chitkara D, Shah ND, Katusic SK, Locke GR 3rd, et al. Longitudinal direct medical costs associated with constipation in women. Aliment Pharmacol Ther. 2011;33(2):251-60. doi: 10.1111/j.1365-2036.2010.04513.x. [ Links ]
6. Martin BC, Barghout V, Cerulli A. Direct medical costs of constipation in the United States. Manag Care Interface. 2006;19(12):43-9. [ Links ]
7. Müller-Lissner SA, Kamm MA, Scarpignato C, Wald A. Myths and misconceptions about chronic constipation. Am J Gastroenterol. 2005;100(1):232-42. doi: 10.1111/j.1572-0241.2005.40885.x. [ Links ]
8. Ziegenhagen DJ, Tewinkel G, Kruis W, Herrmann F. Adding more fluid to wheat bran has no significant effects on intestinal functions of healthy subjects. J Clin Gastroenterol. 1991;13(5):525-30. [ Links ]
9. Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, et al. Bowel Disorders. Gastroenterology. 2016. pii: S0016-5085(16)00222-5. doi: 10.1053/j.gastro.2016.02.031. [ Links ]
10. Kolligs FT. Diagnostics and Epidemiology of Colorectal Cancer. Visc Med. 2016;32(3):158-64. doi: 10.1159/000446488. [ Links ]
11. Fathallah N, Bouchard D, de Parades V. Diet and lifestyle rules in chronic constipation in adults: From fantasy to reality…. Presse Med. 2017;46(1):23-30. doi: 10.1016/j.lpm.2016.03.019. [ Links ]
12. Christodoulides S, Dimidi E, Fragkos KC, Farmer AD, Whelan K, Scott SM. Systematic review with meta-analysis: effect of fibre supplementation on chronic idiopathic constipation in adults. Aliment Pharmacol Ther. 2016;44(2):103-16. doi: 10.1111/apt.13662. [ Links ]
13. Ford AC, Moayyedi P, Lacy BE, Lembo AJ, Saito YA, Schiller LR, et al. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol. 2014;109 Suppl 1:S2-26; quiz S27. doi: 10.1038/ajg.2014.187. [ Links ]
14. Tuteja AK, Talley NJ, Joos SK, Woehl JV, Hickam DH. Is constipation associated with decreased physical activity in normally active subjects? Am J Gastroenterol. 2005;100(1):124-9. doi: 10.1111/j.1572-0241.2005.40516.x. [ Links ]
15. Bharucha AE, Pemberton JH, Locke GR 3rd. American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;144(1):218-38. doi: 10.1053/j.gastro.2012.10.028. [ Links ]
16. Markland AD, Palsson O, Goode PS, Burgio KL, Busby-Whitehead J, Whitehead WE. Association of low dietary intake of fiber and liquids with constipation: evidence from the National Health and Nutrition Examination Survey. Am J Gastroenterol. 2013;108(5):796-803. doi: 10.1038/ajg.2013.73. [ Links ]
17. Eswaran S, Muir J, Chey WD. Fiber and functional gastrointestinal disorders. Am J Gastroenterol. 2013;108(5):718-27. doi: 10.1038/ajg.2013.63. [ Links ]
18. Daley AJ, Grimmett C, Roberts L, Wilson S, Fatek M, Roalfe A, et al. The effects of exercise upon symptoms and quality of life in patients diagnosed with irritable bowel syndrome: a randomised controlled trial. Int J Sports Med. 2008;29(9):778-82. doi: 10.1055/s-2008-1038600. [ Links ]
19. Karjalainen JJ, Kiviniemi AM, Hautala AJ, Piira OP, Lepojärvi ES, Perkiömäki JS, et al. Effects of physical activity and exercise training on cardiovascular risk in coronary artery disease patients with and without type 2 diabetes. Diabetes Care. 2015;38(4):706-15. doi: 10.2337/dc14-2216. [ Links ]
20. Young RJ, Beerman LE, Vanderhoof JA. Increasing oral fluids in chronic constipation in children. Gastroenterol Nurs. 1998;21(4):156-61. [ Links ]
21. Quigley EM. The enteric microbiota in the pathogenesis and management of constipation. Best Pract Res Clin Gastroenterol. 2011;25(1):119-26. doi: 10.1016/j.bpg.2011.01.003. [ Links ]
22. Dimidi E, Christodoulides S, Scott SM, Whelan K. Mechanisms of Action of Probiotics and the Gastrointestinal Microbiota on Gut Motility and Constipation. Adv Nutr. 2017;8(3):484-494. doi: 10.3945/an.116.014407. [ Links ]
23. Wojtyniak K, Szajewska H. Systematic review: probiotics for functional constipation in children. Eur J Pediatr. 2017;176(9):1155-1162. doi: 10.1007/s00431-017-2972-2. [ Links ]
24. Serrano-Falcón B, Rey E. The safety of available treatments for chronic constipation. Expert Opin Drug Saf. 2017;16(11):1243-1253. doi: 10.1080/14740338.2017.1361402. [ Links ]
25. Krogh K, Chiarioni G, Whitehead W. Management of chronic constipation in adults. United European Gastroenterol J. 2017;5(4):465-472. doi: 10.1177/2050640616663439. [ Links ]
26. Farmer AD, Gallagher J, Bruckner-Holt C, Aziz Q. Narcotic bowel syndrome. Lancet Gastroenterol Hepatol. 2017;2(5):361-368. doi: 10.1016/S2468-1253(16)30217-5. [ Links ]
27. Omer A, Quigley EMM. An update on prucalopride in the treatment of chronic constipation. Therap Adv Gastroenterol. 2017;10(11):877-887. doi: 10.1177/1756283X17734809. [ Links ]
28. Nee J, Zakari M, Sugarman MA, Whelan J, Hirsch W, Sultan S, et al. Efficacy of Treatments for Opioid-Induced Constipation: Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2018;16(10):1569-1584.e2. doi: 10.1016/j.cgh.2018.01.021. [ Links ]
Received: February 05, 2018; Accepted: July 03, 2018











 text in
text in