Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.4 Bogotá out./dez. 2018
https://doi.org/10.22516/25007440.222
Original articles
Clinical and epidemiological approach to Hepatitis C in Cali, Colombia
1Departamento de Medicina Interna, Gastroenterología, Fundación Clínica Valle del Lili. Cali, Colombia
2Especialización en medicina interna, Facultad de Ciencias de la Salud, Universidad ICESI. Cali, Colombia
3Departamento de Medicina Interna, Gastroenterología, Fundación Clínica Valle del Lili. Cali, Colombia
4Programa de Medicina, Facultad de Ciencias de la Salud, Universidad ICESI. Cali, Colombia
5Departamento de Medicina Interna, Gastroenterología y Hepatología, Fundación Clínica Valle del Lili. Cali, Colombia
Introduction:
In Colombia, Hepatitis C virus infections have high rates of morbidity and high costs. The advent of new more effective treatments has produced a need for better knowledge of this population’s characteristics to allow their proper use.
Objectives:
The objective of this study is to describe the epidemiological and clinical characteristics of patients with hepatitis C at a referral center for liver diseases.
Materials and methods:
We conducted a cross-sectional descriptive study of a population of adults with serological diagnoses of hepatitis C between 2011 and 2016.
Results:
We evaluated 214 clinical records of patients with confirmed serological diagnoses of hepatitis C. Their median age was 59 years, and 62% were women. The HCV genotypes of 114 patients were reported: 75% had genotype 1B. Transfusions of one or another type of blood product had been administered to 36.9% of the patients, and 5% had tattoos. The prevalence of cirrhosis was 29.4% while that of hepatocellular carcinoma was 3.3%. Hepatitis B virus coinfections were found in 1.8% of these patients, and 5.1% of the patients had human immunodeficiency virus coinfections.
Conclusion:
The determinants of hepatitis C virus infection in Cali are similar to those reported in scientific literature worldwide and requires emphasis on prevention in the at-risk population. Genotype 1b continues to be the most frequent in our environment which makes this population susceptible to new treatments.
Keywords: Hepatitis C virus; hepatocellular carcinoma; cirrhosis; genotype; hepatitis B virus; transfusions; direct antiviral agents
Introducción:
en Colombia, la infección por el virus de la hepatitis C (VHC) representa alta morbilidad y elevados costos. Con la llegada de nuevos tratamientos más efectivos, se hace necesario conocer las características propias de esta población para su adecuado uso.
Objetivos:
describir las características epidemiológicas y clínicas de los pacientes con VHC manejados en un centro de referencia en enfermedades hepáticas.
Materiales y métodos:
se realizó un estudio descriptivo de corte transversal en una población de adultos con diagnóstico serológico de VHC entre el 2011 y el 2016.
Resultados:
se evaluaron 214 historias clínicas de pacientes con diagnóstico serológico confirmado de VHC. La mediana de edad fue de 59 años y el 62 % fue de sexo femenino. El genotipo se reportó en 114 pacientes, el 75 % presentó genotipo 1B. El 36,9 % de los pacientes había recibido algún hemoderivado y el 5 % tenía tatuajes. La prevalencia de cirrosis fue del 29,4 % y de hepatocarcinoma fue del 3,3 %. El 1,8 % y el 5,1 % de los pacientes presentó coinfección con el virus de la hepatitis B (VHB) y virus de la inmunodeficiencia humana (VIH), respectivamente.
Conclusión:
los factores determinantes de la infección por el VHC en Cali presentan un comportamiento clínico similar al que reporta la literatura científica a nivel mundial, lo que obliga a enfatizar en la prevención de la población en riesgo. El genotipo 1B continúa siendo el más frecuente en nuestro medio, lo que hace a esta población susceptible a los nuevos tratamientos.
Palabras clave: Virus de la hepatitis C; hepatocarcinoma; cirrosis; genotipo; virus de la hepatitis B; trasfusiones; agentes antivirales directos.
Introduction
The hepatitis C virus (HCV), a member of the Flaviviridae family, generates acute infections that become chronic in 50% to 85% of cases. There are six known genotypes and at least 50 different subtypes. The main route of transmission of this virus is parenteral (85%), but there are less frequent routes such as sexual transmission (less than 2%) and vertical transmission (10%). 1 Between 5% and 30% of individuals with chronic infections develop cirrhosis. In developed countries such as the United States, HCV infections are the most important causes of liver diseases, as well as the most frequent indication for liver transplantation. 2
The time it takes for an individual to develop cirrhosis after infection has been estimated in a systematic review by Hla-Hla Thein et al. that evaluated 111 studies of which 16% found cirrhosis was still prevalent 20 years after infection. 3
It is thought that one third of patients with hepatocellular carcinoma have HCV infections. Once cirrhosis is diagnosed, several reports have estimated the risk of hepatocellular carcinoma is between 0% and 3% per year. 4,5
HCV and hepatitis B virus (HBV) coinfections are not uncommon since they share similar modes of transmission. The occurrence of these simultaneous infections is much more prevalent in areas where both viruses are endemic and among groups of people at high risk of parenteral infection. Diagnosing HCV/HBV coinfections is clinically important both for a patient’s prognosis, since these patients present more adverse outcomes, and for treatment options. 6
Human immunodeficiency virus (HIV) coinfections are also among the most commonly found HCV patients. Approximately 10% of HCV positive patients are also positive for HIV, and approximately 25% of HIV positive patients are also positive for HCV. This association has been observed mainly in high risk groups such as intravenous drug users. It is known that the presence of both viruses facilitates the transmission of HCV sexually. Likewise, it conditions a more aggressive course of the infection so that end stage liver disease is the main cause of death in this population. This makes timely and adequate screening of these patients fundamental. 7
The 2005 global estimate was that 184 million people had positive antibodies to HCV and that there were moderate prevalences between 1.5% and 3.5% in Latin America. 8 According to the Centers for Disease Control and Prevention (CDC), estimated total incidence in 2010 was 0.3 per 100,000 people in the United States. 9,10
Epidemiological studies in Colombia only present general data. The statistics of SIVIGILA (Sistema Nacional de Vigilancia en Salud Pública - Colombian National Public Health Monitoring System) indicate specific data for at-risk subgroups. Their data show high incidences of infection among blood transfusion recipients (18.9%), homosexuals (12.8%), people with multiple sexual partners (12.6%) and intravenous drug users (9.1%), 11 but information on genotypes and the most frequent outcomes of the disease (cirrhosis, hepatocellular carcinoma and transplants) is not included.
The incidence of infection was impacted by implementation of compulsory screening for HCV by blood banks in 1993. Prior to this measure, the probability of receiving a unit of infected blood was 0.74%, and the probability of an infection transmitted by a transfusion was 0.67%. These figures placed Colombia among the countries with the highest risk of transmission of infection in Latin America. In 2002, there was a 99.7% increase in the screening for HCV in blood banks, with a notable reduction in the risk (0.0024%) of receiving infected blood. 12
Information the epidemiological and clinical behavior of the disease in Cali and Valle del Cauca there is scarce, so this study fills a gap by identifying the most prevalent genotypes and the most frequent complications and factors associated with this entity.
Materials and methods
Type of Study
The inclusion criteria of this cross-sectional descriptive study were that patients had to be adults patients of either sex at the gastrohepatology service of the institution who had been diagnosed with HCV because of total antibodies against HCV and/or a positive viral load.
Clinical records of patients in the institution’s computer system (SAP1) were reviewed to identify diagnoses by ICD-10 codes for HCV and viral hepatitis who had been treated between 2011 and 2016. The information was then recorded on a data collection form designed for that purpose.
Data Analysis
Clinical information, test results and epidemiological data were recorded in an electronic database. The data were summarized using standard deviations, medians, and interquartile ranges as appropriate. Univariate analysis used the Shapiro-Wilk test to evaluate distributions of numerical variables. Qualitative variables were expressed as proportions. Data were analyzed with Stata® (Stata Corp, 2011, Stata 12 Base Reference Manual, College Station, TX, United States).
Results
The study evaluated 232 clinical records of patients with ICD-10 diagnoses of HCV who had been treated at the gastrohepatology outpatient service of the Valle de Lili Foundation between January 1, 2011 and December 31, 2016. Of this population, 214 patients met the inclusion criteria. The remaining 18 were excluded because they did not have confirmed diagnoses of HCV infection or because they had died by the time of data collection (mortality was not a subject of this study). The general characteristics of this population can be found in Table 1.
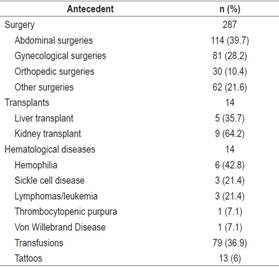
Evaluation of antecedents related to the contagion of the virus (Table 2) showed that the majority of patients (75%) had undergone at least one surgical procedure, with a general average of 1.34. surgeries per patient. Kidneys were the organs most frequently transplanted among these patients (64.2%). Liver transplantation was found less frequently, but there is no clarity in the clinical histories about whether viral infections required this procedure.
It is widely recognized that, because patients with hematological diseases frequently require transfusion of blood products throughout life, they are at great risk of HCV infection through this route. In the population analyzed, 6.5% of the patients had some alteration of this nature: 42.8% , had hemophilia, 21.4% had sickle cell anemia, and 21.4% had neoplasms.
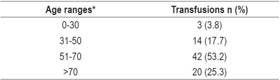
Histories of tattoos and/or transfusions of blood products were also analyzed for associations with HCV, and 6.07% of the patients were found to have tattoos noted in medical records while 36.92% of patients with chronic HCV infections had had blood transfusions. Of the 59 people with histories of transfusion, the majority were female (64.5%). Of the total transfused, 53.16% were between 51 and 70 years old, and about 25% were older than 70 years (Table 3). Although people over 50 years of age more frequently had histories of transfusions, these associations were not statistically significant.
HIV/HBV coinfections were also estimated. We found 4 patients (1.86%) who had simultaneous HBV and HCV, and 11 patients (5.14%) with simultaneous HCV and HIV. Of the latter, 100% were male. Only one of the four patients with HBV was female. The majority (63.6%) of patients with HIV had coinfections with HCV genotype 1A.
The most frequent complication found in patients with chronic HCV infections was cirrhosis, with a prevalence of 29.4%. Hepatocellular carcinoma was found in about 3.3% of patients.
It was observed that 75% of the patients had HCV genotype 1B, 13% had genotype 1A and the remaining 12% had other genotypes (Figure 1). 2 Of the 117 patients with genotype 1B, the majority (72 individuals) were born between 1941 and 1960. The presence of cirrhosis among patients with genotype 1B was 67.5%, with a p of 0.70.
Discussion
The study showed a higher prevalence of infected women (61.6%) than men in Colombia with a tendency similar to that of the most recent epidemiological reports in the United States where 52% of those infected are women. 13 The majority of individuals were adults in the fifth decade of life. The highest proportion (54.7%) of patients were born between 1941 and 1960, unlike the prevalence found in a study conducted by Smith et al. in which around 80% of the patients had been born between 1945 and 1965. 14
Colombian statistics reported SIVIGILA for 2017 show a predominance of males (57.3%), but proportions by sex vary according to departments and districts. The highest proportion reported by age was 26.4% for populations aged 65 and over. 15 This finding is of special importance for evaluating HCV risk factors since, prior to the nineties, routine screening for HCV was not performed for blood products in blood banks in Colombia. As reported by La Hoz et al. in the Colombian HCV consensus, 16 the probability of contracting the virus among transfused people in the entire country 1.5% in 1992. Therefore, it is possible that this has been the source of contagion for a large proportion of patients born in this age group.
Tattoos are a widely recognized HCV risk factor both in terms of the use of contaminated needles and because of skin and mucosal lesions which expose epithelial barriers to infection by the virus. In our population, 6% of the individuals studied had tattoos. However, the clinical histories do not clearly state either where or when tattoos were done, so there is no information about whether they were done prior to diagnosis or after. By the same token there is no information about conditions of hygiene. This information would be of great epidemiological value, but it was difficult to obtain since many patients had been previously seen in other institutions where this information is not routinely recorded. The SIVIGILA statistics for 2017 mention this important risk factor, and national compulsory reporting for the epidemiological record (code INS 340) covers aesthetic procedures such as piercings and tattoos, but there is no place where the circumstances of these procedures are recorded. Therefore, it is difficult to report more detailed data that closely relate the infection to the type of tattoo and the conditions under which it was done. This is a limitation of the study.
A significant factor associated with chronic infections in our institution was transfusion of blood products whose prevalence was 36.9%. This coincides with findings from other regions of the country as described by Yepes et al. in a case-control study conducted on the Colombian Caribbean coast where a significant Odds Ratio (OR) was evidenced for this risk factor. 17 This study also found that a slightly higher proportion (64.5%) of women, most of whom were over 50 years old, had been transfused. However, careful evaluation of the data showed that most of these women had undergone surgery with low risk of bleeding, especially hysterectomies which accounted for 55.5% of the patients. This procedure has low rates of perioperative bleeding that range between 1% and 2%. They can even be lower depending on the surgical approach used. 18
The most important risk factor found in the population studied was surgical history, with a prevalence of 75% among patients with HCV. Most of these patients had undergone more than one surgical procedure, with a total of 287 surgeries of various kinds recorded in the medical records. It should be noted that many patients had no other antecedents or risk factors for contagion at their first visit to hepatology for the infection, so this could be a significant source of transmission of the virus. Nevertheless, it is difficult to establish a causal relationship since the descriptive design of this study does not allow it. Its retrospective nature makes it difficult to determine whether surgery was really prior to viral contagion and whether there were other factors such as surgical time, bleeding and type of surgery that favor infection.
Another important point is the incidence of hematological diseases among infected patients since they require large amounts of transfusions. Hematological diseases were found in 6.5% of the patients studied with hemophilia being the most frequent pathology, possibly due to its high risk of major bleeding.
Previous Colombian studies support the findings of this study that genotype1B occurs in about 75% of the patients. The second most frequent was 1A (12%). In 2017, a study by Santos et al. reported that 70% of patients had genotype 1B and 13.5% had genotype 1A. That study’s objective was to describe the genotypes and subtypes of HCV in infected Colombian patients. (19) They found that this is important because genotype 1B has been closely related to the use of blood products and invasive procedures in which bleeding and mucosal manipulation occur. This have been associated with inadequate hygiene, so this could be the main factor associated with transmission of the disease in Colombia. Another important observation regarding genotype is the fact that new direct antiviral treatments have shown higher success rates against subtype 1B than against other subtypes, so that it may be possible to treat more than 70% of those infected in Colombia without interferon.
Coinfections of HIV and HCV are particularly important for appropriate diagnosis and treatment. A metaanalysis of about 780 studies that evaluated HIV-infected populations around the world has estimated that overall prevalence of HCV coinfections is to 6%. 20. Colombian prevalence of HIV was found to be 5.14% which is very close to the epidemiological data found worldwide. A high prevalence of coinfections has been documented in Colombia, especially among patients who use intravenous drugs in Armenia, Cúcuta and Bogotá, cities in which studies were conducted on patients who use these psychotoxic agents. 21,22 These two studies found that sexual relations between men, failure to use condoms, and promiscuity were the main risk factors. Despite the epidemiological importance of these data, it was not possible for this study to determine the number of sexual partners of coinfected individuals since this information was not routinely recorded in clinical records.
There were no intravenous drug users among the patients treated at this institution which can be explained by the fact that this population of patients is treated at rehabilitation centers and specific HIV management programs. It is essential to specify that there could be an information bias in general questions about patients histories of psychotoxic drug consumption rather than asking specifically about intravenous drug use. It is also possible that many patients omitted this information despite drug use for fear of being valued in a negative way. This should motivate the institution both to improve the quality of the registry of risk factors in clinical histories and to establish a series of specific questions (time and duration of exposure, number of sexual partners, etc.) for patients identified as members of vulnerable populations.
In the study population, 1.86% of patients had HBV coinfections. This prevalence might be due to the fact that many co-infected patients lacked serological markers for HBV infections. This was illustrated in a study in which 33% of 200 patients infected with HCV had negative surface antigen for HBV (HBsAg) but had detectable viral loads for HBV. The reason why some patients with HCV who are infected with HBV lack HBsAg is unknown. However, the data found in this study did not differ much from prevalence reports of coinfection by other authors. 11 We suggest that it would be pertinent to study both the presence of the surface antigen for HBV and the viral load of patients with HCV infections.
The prevalences of cirrhosis and hepatocellular carcinoma found in the study population were very similar to what was expected according to reports in the literature: 29.4% had cirrhosis, and 3.3% had hepatocellular carcinoma. Overall, it is expected that 20% to 30% of patients with HCV will develop cirrhosis, 23 and that 0% to 3% per year will develop hepatocellular carcinoma. 4,5. A prevalence of 35.7% of liver transplants was observed among the transplant group. Unfortunately, it was not possible to establish whether all transplants were performed due to deterioration of liver function secondary to HCV infections since the medical records did not consistently record this information.
On the one hand, the main limitation of this study was the heterogeneity of the clinical records registered by the different specialists (hepatologists, infectious disease specialists and gastroenterologists). Similarly, there was inadequate information regarding tattoos, blood transfusions, sexual health, use of psychotoxic agents and surgical history; This leads to replanting the importance of recording this information, since this could be used to implement intervention measures at the public health level, such as the inclusion of more specific questions about these risk factors in the epidemiological files (INS code 340).
On the other hand, the main strength of this study is its epidemiological analysis of variables associated with chronic HCV infections. This information is current and combines both serological information and the main clinical characteristics of the population of Valle del Cauca. According to the latest report from the National Health Institute, this population ranks fifth in the incidence of HCV in 2018, 24 and held first place in the number of deaths attributable to the virus in 2017. 15 Therefore, this information can serve as a basis for studies that focus on diagnosis and antiviral treatment of this entity.
Conclusion
Based on this study’s results, it can be concluded that HCV infections in the Colombian population evaluated behave in a manner very similar to that found in the scientific literature. Viral genotype 1B predominates, so much of our population could be treated with the new direct antiviral agents which have less adverse effects and higher rates of cure for this subtype. This study also shows that, despite public policies for handling of blood products and guaranteeing hygienic practices for invasive procedures, this route of infection continues to be the main factor associated with infections. Consequently, we must continue working on education and prevention of infection. In addition, we propose an active search throughout the country for patients with a history of blood transfusions prior to 1993. This could follow pilot screening strategy implemented in Antioquia by Arroyave et al. 25 for HCV in patients who had received transfusions before 1994. It found a prevalence of 6.6% for antibodies to the virus and 4.2% for chronic HCV, and it was shown to be an effective screening strategy. Therefore, we proposed that this type of screening been implemented first on an institutional basis and later on a departmental basis.
Acknowledgments
The authors especially want to thank the Valle de Lili Foundation and its Clinical Research Center for their support and collaboration in the development of this work
REFERENCES
1. Cercenado Mansilla E, Cantón Moreno R. Diagnóstico microbiológico de las hepatitis víricas. Procedimientos en Microbiología Clínica. España: SEIMC; 2014. [ Links ]
2. Chopra S, Di Bisceglie AM, Bloom A. Clinical manifestations and natural history of chronic hepatitis C virus infection. UpToDate [internet] 2015 [acceso el 21 de agosto de 2017]. Disponible en: Disponible en: https://www.uptodate.com/contents/clinical-manifestations-and-natural-history-of-chronic-hepatitis-c-virus-infection . [ Links ]
3. Thein HH, Yi Q, Dore GJ, Krahn MD. Estimation of stage-specific fibrosis progression rates in chronic hepatitis C virus infection: a meta-analysis and meta-regression. Hepatology. 2008;48(2):418-31. doi: 10.1002/hep.22375. [ Links ]
4. Hu KQ, Tong MJ. The long-term outcomes of patients with compensated hepatitis C virus-related cirrhosis and history of parenteral exposure in the United States. Hepatology. 1999;29(4):1311-6. doi: 10.1002/hep.510290424. [ Links ]
5. Fattovich G, Giustina G, Degos F, Tremolada F, Diodati G, Almasio P, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112(2):463-72. [ Links ]
6. Chu CJ, Lee SD. Hepatitis B virus/hepatitis C virus coinfection: epidemiology, clinical features, viral interactions and treatment. J Gastroenterol Hepatol. 2008;23(4):512-20. doi: 10.1111/j.1440-1746.2008.05384.x. [ Links ]
7. Maier I, Wu GY. Hepatitis C and HIV co-infection: a review. World J Gastroenterol. 2002;8(4):577-9. [ Links ]
8. Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013;57(4):1333-42. doi: 10.1002/hep.26141. [ Links ]
9. Wasley A, Grytdal S, Gallagher K; Centers for Disease Control and Prevention (CDC). Surveillance for acute viral hepatitis--United States, 2006. MMWR Surveill Summ. 2008;57(2):1-24. [ Links ]
10. Centers for Disease Control and Prevention. Viral Hepatitis Surveillance - United States, 2010. CDC [internet] 2012 [acceso el 16 de septiembre de 2018]. Disponible en: Disponible en: https://www.cdc.gov/hepatitis/Statistics/2010Surveillance/index.htm . [ Links ]
11. Cacciola I, Pollicino T, Squadrito G, Cerenzia G, Orlando ME, Raimondo G. Occult hepatitis B virus infection in patients with chronic hepatitis C liver disease. N Engl J Med. 1999;341(1):22-6. doi: 10.1056/NEJM199907013410104. [ Links ]
12. Páez Rodríguez OE, Peñaloza F. I. Epidemiología. Rev Col Gastroenterol. 2012;27(Suppl 2): 4-6. [ Links ]
13. Suryaprasad AG, White JZ, Xu F, Eichler BA, Hamilton J, Patel A, et al. Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006-2012. Clin Infect Dis. 2014;59(10):1411-9. doi: 10.1093/cid/ciu643. [ Links ]
14. Smith BD, Patel N, Beckett GA, Jewett A, Ward JW. Hepatitis C virus antibody prevalence, correlates and predictors among persons born from 1945 through 1965, United States, 1999-2008 [Abstract]. Presented at The Liver Meeting; San Francisco, California. 4-8 November 2011; Abstract 241. [ Links ]
15. Peralta Carvajal JC. Informe de evento. Hepatitis B, C y B-D. Colombia, año 2017. Colombia: Instituto Nacional de Salud; 2017. [ Links ]
16. de la Hoz F. Epidemiología de la hepatitis C en Latinoamérica y Colombia. Biomedica. 2000;20(1):66-72. [ Links ]
17. Yepes IJ, Lince B, Caez C, De Vuono G. Risk factors for hepatitis C virus infection in the Colombian Caribbean coast: A case-control study. Biomedica. 2016;36(4):564-571. doi: 10.7705/biomedica.v36i4.3105. [ Links ]
18. Parker WH, Wagner WH. Gynecologic surgery and the management of hemorrhage. Obstet Gynecol Clin North Am. 2010;37(3):427-36. doi: 10.1016/j.ogc.2010.05.003. [ Links ]
19. Santos O, Gómez A, Vizcaíno V, Casas MC, Ramírez MP, Olaya P. Genotipos circulantes del virus de la hepatitis C en Colombia. Biomédica. 2017;37(1):22-7. doi: 10.7705/biomedica.v37i1.3173. [ Links ]
20. Platt L, Easterbrook P, Gower E, McDonald B, Sabin K, McGowan C, et al. Prevalence and burden of HCV co-infection in people living with HIV: a global systematic review and meta-analysis. Lancet Infect Dis. 2016;16(7):797-808. doi: 10.1016/S1473-3099(15)00485-5. [ Links ]
21. Berbesi-Fernández DY, Segura-Cardona AM, Montoya-Velez LP, Santamaría AÁ. Use of injected heroin and risk of hepatitis C in three cities in Colombia. Rev Bras Epidemiol. 2017;20(3):435-44. doi: 10.1590/1980-5497201700030007. [ Links ]
22. Berbesi-Fernández D, Segura-Cardona Á, Montoya-Vélez L, Castaño-Pérez GA. Hepatitis C y VIH en usuarios de drogas inyectables en Armenia-Colombia. Adicciones. 2015;27(4):246-52. doi: 10.20882/adicciones.749. [ Links ]
23. Alberti A, Chemello L, Benvegnù L. Natural history of hepatitis C. J Hepatol. 1999;31 Suppl 1:17-24. [ Links ]
24. Peralta Carvajal JC. Informe de evento. Hepatitis B, C y B-D. Colombia, período VI de 2018. Colombia: Instituto Nacional de Salud ; 2018. [ Links ]
25. Arroyave JC, Álvarez C, Correa G, Balcázar NM, Arbeláez MP, Navas MC. Infección por el virus de la hepatitis C en individuos transfundidos antes de 1994 en Antioquia, Colombia. Rev Col Gastroenterol. 2014;29(4):383-9. [ Links ]
Received: March 04, 2018; Accepted: June 10, 2018











 texto em
texto em