Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.4 Bogotá Oct./Dec. 2018
https://doi.org/10.22516/25007440.223
Original articles
Experience with video capsule endoscopy (VCE) in the study and diagnosis of small bowel diseases in a tertiary hospital in Medellín, Colombia
1 Especialista en medicina interna, gastroenterología y endoscopia digestiva. Hospital Pablo Tobón Uribe. Medellín, Colombia
2 Residente de medicina interna, Universidad de Antioquia. Medellín, Colombia
3 Médica, Unidad de gastroenterología y endoscopia digestiva. Hospital Pablo Tobón Uribe. Medellín, Colombia
Introduction:
The small intestine is a difficult organ to study due to its large size and anatomical location. Conventional esophagogastroduodenoscopy and colonoscopy cannot evaluate the entirety of the small intestine and balloon enteroscopy is more invasive, has more adverse effects, and has higher complication rates. Video capsule endoscopy (VCE) is a minimally invasive technology that allows a dynamic and complete view of the mucosa of the small intestine. It is the safest direct method which has the lowest complication rates.
Methodology:
This is a cross-sectional descriptive observational study that describes clinical experience in the use of VCE at a highly complex hospital in Medellin, Colombia. It also describes the indications for VCE, and the most common symptoms and abnormal findings.
Results:
VCE was used to study 282 outpatients (75.4%) and 92 hospitalized patients (24.6%) during the study period. In both groups, the most frequent indication was obscure digestive bleeding (38.65% and 53.26% respectively), followed by chronic anemia in 27.65% of outpatients, and inflammatory bowel disease (IBD) in 21.74% of hospitalized patients. Abnormal findings were more frequent in the jejunum, and the most common lesions were angiodysplasias and inflammatory lesions.
Conclusions:
Potential sources of bleeding were documented in more than 70% of the cases of the most frequent indications which were obscure digestive bleeding and anemia. Vascular and inflammatory lesions were the most common findings. In follow-up evaluation of IBD, inflammatory lesions were documented in more than 50% of the cases. VCE is very safe, and there were no complications related to the VCE.
Keywords: Endoscopic capsule; enteroscopy; small intestine; dark digestive bleeding
Introducción:
el intestino delgado (ID) es un órgano difícil de estudiar debido a su gran tamaño y ubicación anatómica; los estudios endoscópicos convencionales (esofagogastroduodenoscopia y colonoscopia) no logran evaluarlo en su totalidad y la enteroscopia con balón es más invasiva, con mayores efectos adversos y tasas de complicaciones. La videocápsula endoscópica (VCE) es una tecnología mínimamente invasiva que permite visualizar de forma dinámica y completa la mucosa del ID; es el método directo más seguro y con menos tasas de complicaciones.
Metodología:
se realizó un estudio descriptivo de corte transversal, para describir la experiencia clínica en la utilización de la VCE en un hospital de alta complejidad en Medellín, Colombia; asimismo, determinar las indicaciones, síntomas más comunes y hallazgos anormales.
Resultados:
se realizaron 374 VCE en el período de estudio: 282 ambulatorias (75,4 %) y 92 hospitalizados (24,6 %). En ambos grupos la indicación más frecuente fue sangrado digestivo oscuro (38,65 % y 53,26 %, respectivamente), seguidos por anemia crónica en el 27,65 % de ambulatorios y por enfermedad inflamatoria intestinal (EII) en 21,74 % de los hospitalizados. Los hallazgos anormales fueron más frecuentes en el yeyuno y las lesiones más comunes fueron angiodisplasias y lesiones inflamatorias.
Conclusiones:
en las indicaciones más frecuentes (sangrado digestivo oscuro y anemia) se documentaron potenciales fuentes de sangrado en más del 70 % de los casos; siendo las lesiones vasculares e inflamatorias los hallazgos más comunes. En seguimiento o evaluación de EII se documentaron en más del 50 % lesiones inflamatorias. La VCE es muy segura, no se presentó ninguna complicación relacionada con la VCE.
Palabras clave: Cápsula endoscópica; enteroscopia; intestino delgado; sangrado digestivo oscuro
Introduction
Statement of the Problem and Justification
The small bowel is an organ located in the middle part of the digestive tract. Due to its size (on average 6 meters long), anatomical location and structural characteristics, it is difficult to inspect through conventional esophagogastroduodenoscopy and colonoscopy. Exploration of the small bowel through simple or double balloon enteroscopy is more invasive, generates more adverse effects, has higher rates of complications, and initial evaluation is limited by the entry route (antegrade or retrograde) which must be chosen very well. Intraoperative enteroscopy requires laparoscopy or an open laparotomy for surgically assisted passage of an endoscope into the intestine. Both procedures are very invasive and increase morbidity and mortality rates.
Endoscopic videocapsules (VCEs) are a minimally invasive technology which can be used to view the entire mucosa of the small bowel dynamically. VCEs are easy to use and comfortable for the patient, and they usually require no sedation. Since they were approved for use in humans, indications for this study have been extended to include obscure and occult digestive bleeding, chronic anemia, Crohn’s disease, tumors of the small bowel, hereditary polyposis syndromes, Celiac disease, chronic diarrhea and abdominal pain.1,2 In addition, VCE’s allow location of lesions in order to determine by the best invasive pathway for taking biopsy samples for histological diagnosis (anterograde enteroscopy versus retrograde enteroscopy).2,3
In August 2001, the Food and Drug Administration (FDA) approved diagnostic use of VCEs in the small bowel of humans. In 2003, Clínica Marly in Bogotá became the first medical center in Colombia, to acquire this technology. In 2009, its experience with VCE in 100 patients was published. 4 In the same year, the gastroenterology and digestive endoscopy unit here at Hospital Pablo Tobón in Medellín began using VCE. Initially, we used the Olympus VCE, and in 2011 we published our experience with the use of VCE to diagnose occult digestive bleeding. 5 Since 2014, we have used the PillCam SB 3 video capsule for evaluation of pathologies of the small bowel for outpatients as well as inpatient.
Given that the Hospital Pablo Tobón Uribe Hospital is a referral center for digestive diseases for the region around Medellín, we have decided to present our experience in determining indications for use of VCE, population risk factors, locations of lesions documented, and types of lesions found while also evaluating whether VCE results have significantly modified management of patients with abnormal findings.
Materials and methods
This is a descriptive cross-sectional study of patients who were diagnosed using VCE between January 2014 and December 2017. A detailed review of variables in the data obtained through the procedure and in the hospital’s medical history and the medical histories provided by outpatients. The data was recorded in Excel for further statistical analysis.
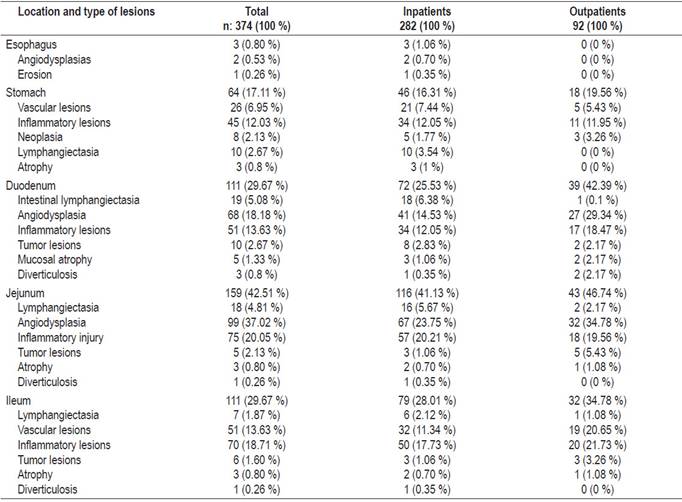
Table 1 contains demographic data including the numbers of inpatients and outpatients, indications for VCE, and the primary reason the patient was referred to our hospital as well as risk factors such as cigarette smoking, alcohol consumption, use of non-steroid anti-inflammatory drugs (NSAIDs), glucosamine, homeopathic medicines, anticoagulants, antiplatelet drugs, liver disease and history of chronic kidney disease (CKD). The preparation prior to VCE and findings from VCE are described in the results section.
Table 1 Demographic and clinical data plus indications for VCE at HPTU
IBD: inflammatory bowel disease; VCE: endoscopic videocapsule.
Patients over the age of 15 years were included after signing the hospital’s informed consent form.
Description of Procedure
The PillCam SB 3 video camera measures 26.2 mm x 11.4 mm and weighs 3 g. Its field of view is 156 degrees and can record photos for an estimated time of 8 hours. After activation, the capsule takes two to six photos per second.
Standard preparation of both outpatients and inpatients uses two envelopes of polyethylene glycol 3350 and one chewable simethicone tablet taken the day before the procedure In addition, patients must fast for at least eight hours before the procedure. Eight sensors are placed on the abdominal wall and connected to a data recorder that is located in a belt the patient wears throughout the examination. The manufacturer of the system is Given Imaging.
After synchronizing the capsule with the data recorder, patients swallowed the capsule with 10-20 mL of water. They stayed in the digestive physiology room until the capsule had advanced to the duodenum. When a capsule did not advance by itself, we advanced it endoscopically. In cases of patients with swallowing disorders, the capsule was passed through the advancement device. Patients were then instructed that they could drink liquids one hour after verification that the capsule had entered the small bowel. Four hours later patients were able to eat normally and perform daily activities. The recorder was removed after eight to ten hours.
In all cases, the video was thoroughly evaluated by the specialist in charge at a speed of five photos/second. Cases of doubts were reviewed and discussed with a second operator.
Data Collection Method and Analysis
Data for all variables were recorded in an Excel database. Descriptive statistics including mean frequencies and percentage distributions were used for nominal or ordinal categorical variables and measures of central tendency such as averages and medians were used for numerical variables.
Population and Sample
The study population consisted of patients older than 15 years who underwent VCE at HPTU in Medellín, Colombia.
Ethical Considerations
The study protocol was presented to the HPTU ethics committee where it was evaluated and approved. International and national ethical recommendations including the Helsinki Declaration and Resolution 8430 of 1993 of the Ministry of Health of Colombia were followed. According to that resolution, this study had minimal risk since it does not put patients’ integrity at risk.
Results
A total of 374 VCE studies were performed in the study period: 282 were outpatients (169 women, 113 men) and 92 patients (49 women, 43 men) were inpatients. Average participant age was 56.5 with a range of 15 to 92 years.
Preparation of the small bowel was considered to be adequate in 79/92 (85.87%) of the inpatients and in 258/282 (91.49%) of the outpatients. The most frequent indication was occult digestive bleeding for both outpatients and inpatients. It was observed in 109/282 (38.65%) of the outpatients and in 50/92 (53.26%) of the inpatients. Second most frequent among outpatients was chronic anemia in 78/282 (27.65%) while second most frequent among inpatients was follow-up or diagnosis of with Crohn’s disease in 20/92 (21.74%).
Risk factors related to digestive bleeding identified in inpatients included smoking (17/92, 18.48%), antiplatelet drugs (15/92, 16.30%), NSAIDs (7/92, 7.60%) and alcohol consumption (3/92, 3.26%). An ulcer with severe inflammatory stenosis was identified in one patient who had taken glucosamine (Figure 1A). Risk factors related to digestive bleeding identified in outpatients included smoking (40/282, 14%), alcohol consumption (26/282, 9%), use of antiplatelet drugs or anticoagulants (28/282, 10%), NSAIDs (25/282, 8.8 %), glucosamine (4/282, 1.4%), homeopathic drugs (1/282), chronic liver disease (9/282, 3.1%) and CKD (13/282, 4.6%).
In order of frequency, outpatients’ symptoms were anemia in 134 patients (47.52%), chronic diarrhea in 54 patients (19.15%), manifest digestive bleeding in 45 patients (15.95%), unexplained weight loss in 23 patients (8.15%) and abdominal pain in 16 patients (5.67%). For inpatients, the most frequent symptoms were bleeding in 49 patients (53.26%), anemia in 22 patients (23.91%), diarrhea in 15 patients (16.30%), abdominal pain in 4 patients (4.35%) and recurrent oral aphthae in one patient (1.08%).
Endoscopy had been performed previously on 86/92 inpatients (93.5%) and 81/92 (88%) had undergone colonoscopy.
Eighteen of the inpatients (19.56%) underwent enteroscopy due to abnormal VCE findings. Of these, ten had vascular lesions due to angiodysplasias and underwent enteroscopy with argon plasma coagulation. Five of these had been diagnosed with Osler-Weber-Rendu syndrome. Inflammation, tumors, or other lesions were found in the other eight patients, so they underwent enteroscopy to take biopsies and mark the lesions.
Of the 159 cases of occult digestive bleeding in both groups, 73 cases (45.91%) were due to vascular causes and 53 cases (33.33%) were due to inflammatory lesions. Potential sources of bleeding were identified in more than 70% of the 93 total cases of anemia: vascular lesions in 36 cases (38.71%) followed by inflammation in 26 cases (27.95%) and tumors in six cases (6.45%). Of the 62 cases related to diagnosis and follow-up of inflammatory bowel disease, 34 cases (54.83%) had inflammatory lesions (Figures 1B-1D) and seven cases (11.29%) had vascular lesions.
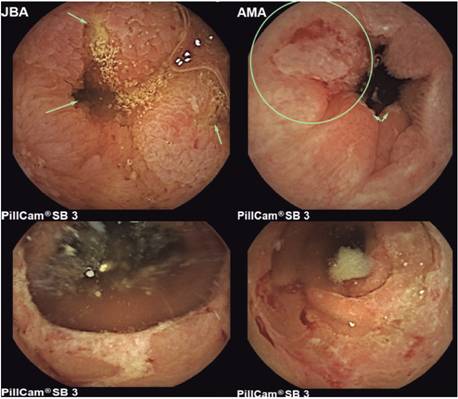
Figure 1A Ulcerated enteritis with stenosis due to glucosamine consumption. 1B. Ulcerated ileitis in a patient with Crohn’s disease. 1C. Inflammatory hemi-circumferential ulcer in the ileum of a patient with Crohn’s disease. 1D. Inflammatory ulcers with active bleeding in the jejunum.
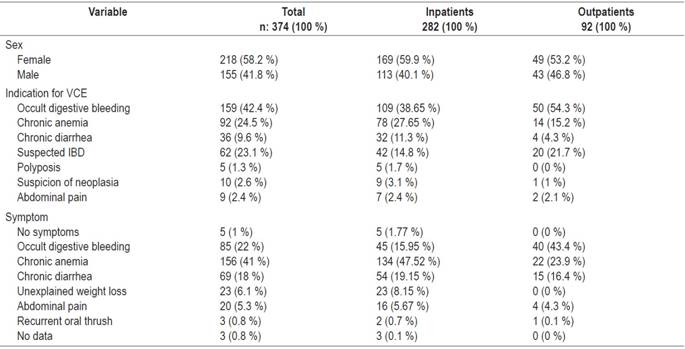
The most frequent location of abnormal findings in inpatients was the jejunum (43/92, 46.7%), and in these patients the most frequent lesions were angiodysplasias (32/43, 74.4%) and inflammatory lesions (18/43, 41.8%). The duodenum was the second most common location (39/92, 42.3%), but in these patients the most frequent lesions were angiodysplasias (27/39, 69.2%) followed by inflammatory lesions (17/39, 43.5%) (Table 2).
Twelve tumors were documented. Six were benign polyps in the stomach and duodenum, one patient had a gastric neoplasia and the rest had ulcerated subepithelial lesions that were related to neuroendocrine tumors in the jejunum and ileum.
Discussion
Currently available techniques for evaluation of the small bowel include VCE, balloon enteroscopy, CT enterography, magnetic resonance enterography and intraoperative enteroscopy (which is rare). These modalities can recognize the majority of small bowel lesions and can impact therapeutic strategies by making surgical interventions unnecessary or by decreasing surgical times due to better localization of a lesion. 1,2,3,6 Despite these advances in the study of the small bowel, the most efficient approach for management of patients suspected of bleeding in the small bowel bleeding has not been fully determined. Nevertheless, the strongest recommendation is to use VCE for diagnosis. 1,2,6 Because of all this growth in diagnostic methods to explore the small bowel, a recently published clinical guide recommends changing the term occult digestive bleeding to small bowel bleeding, reserving the term occult digestive bleeding for bleeding that cannot be identified after evaluation of the entire gastrointestinal tract. 7
The work of Maeda et al. has shown that the sensitivity and negative predictive value of VCE are both 100% for presence of lesions in the small bowel and for the therapeutic approach in cases with significant lesions. In this study, the VCE never missed the relevant findings in the small bowel. A fact of great interest is that the negative findings of a VCE almost always corresponded to an inadequate indication.3 A recent systematic review and metaanalysis has shown that negative VCE indicates a low risk of rebleeding in the future. Therefore, these patients should be discharged and can be treated safely with watchful waiting. 8 Nevertheless, a letter to the editor about that systematic review and metaanalysis has warned that negative results of an examination should never reassure an attending physician. On the contrary, close monitoring and a low threshold for repeating endoscopy is recommended in order to identify lesions not related to the small bowel in patients with overt bleeding. 9 Patients who bleed again after two years may need additional diagnostic study. 8
Diagnostic yield evidenced in the data used in this study was good: potential causes were documented for more than 70% of the two most frequent indications, digestive bleeding and anemia. A recent metaanalysis has found that the combined diagnostic yield of VCE in patients with occult digestive bleeding (overt or hidden) was 61.7%. 10 Several factors influence the probability of finding the lesion which causes the bleeding: active bleeding, a decrease of more than 3 g of hemoglobin, and the time of the study with respect to the last day of bleeding. Depending on these factors, the yield can vary between 11% and 87%.1,6
Inflammatory lesions were identified in 50% of the patients in our study who were suspected of having of inflammatory bowel disease or who had previous been diagnosed with IBD. Although up to 66% of patients with Crohn’s disease have small bowel compromise at diagnosis, up to 90% are in the distal ileum. 11 Some studies have shown that VCE evaluation of the small bowel increases diagnoses of Crohn’s disease by 22% to 24% due to discovery of lesions not evidenced in imaging studies and not found through colonoscopy due to the impossibility of entering the ileum.12,13 This makes the VCE an ideal complementary method for patients who have symptoms compatible with Crohn’s disease as well as for patients with elevated acute phase reactants or fecal calprotectin for whom an accurate diagnosis of the disease and/or its extension has been impossible to reach. VCE can result in reclassifying patients who had initially been diagnosed with ulcerative colitis or indeterminate colitis. When evidence of lesions in the small bowel is found, they should be managed as if they had Crohn’s disease. In addition, learning the degree of small bowel compromise can have implications for treatment, monitoring and prognosis of the disease. Finally, VCE can be used to monitor known lesions to evaluate response to treatment and determine deep remission or the need for modifications in maintenance therapy. 14
The capsule was fundamental for making diagnostic and therapeutic decisions in relation to abnormal findings. Double-balloon enteroscopy was performed in almost 20% of the inpatients with obscure gastrointestinal bleeding. Some of these were for therapeutic purposes through application of argon plasma coagulation of vascular lesions while others were diagnostic through taking of biopsies and marking of tumors for resection. For all cases of enteroscopy, VCE findings guided definition of the enteroscope entry path (antegrade or retrograde) by the topographic location in accordance with recommendations in the literature.1,2,3,6,7
Most inpatients had previously undergone endoscopy (86/92, 93.5%) and (81/92, 88%). But many patients in the study were outpatients, including those referred from other cities, who had not. Also, diagnostic suspicion of CD compromising the small bowel was the second most common reason for examining inpatients. For these patients, VCE is used to establish the extent of the disease and compromise of the small bowel. 10 Consequently, these data differ from those reported by Dr. Galiano et al. One hundred percent of that cohort of patients had had upper gastrointestinal endoscopy and colonoscopy before the VCE study. 4 Despite this, we do agree with, and adhere to, recommendations for conducting baseline studies, especially for patients with occult digestive bleeding or chronic anemia with suspected gastrointestinal blood loss.
The risks inherent to VCE are low. Retention of the capsule has been described, but this occurs in only about 1% of cases. 4 In our series there were no complications. Patients with obstructive symptoms such as vomiting associated with distension and/or abdominal pain have the greatest risks of capsule retention, so it is recommended that their small bowels be studied with CT enterography or MR enterography depending on local experience and institutional availability. 6
In conclusion, of the multiple indications for VCE in our center, occult digestive bleeding and anemia were the most frequent, and the diagnostic yield exceeded 70%. For inpatients, VCE was used to study and evaluate those with suspected or known diagnoses of Crohn’s disease. In the latter case, VCE provides exceptional additional information related to diagnosis, classification, prognosis and follow-up.
VCEs are safe - there were no complications related to this procedure in this study - and it is a very useful tool for defining the route of entry and the initial approach to digestive bleeding. To date, this is the largest series published in Colombia. Multicenter studies are recommended for our country so that we can gain a better understanding of the prevalence and incidence of small bowel lesions while learning the operational characteristics of this method in our population.
Referencias
1. Enns RA, Hookey L, Armstrong D, Bernstein CN, Heitman SJ, Teshima C, et al. Clinical Practice Guidelines for the Use of Video Capsule Endoscopy. Gastroenterology. 2017;152(3):497-514. doi: 10.1053/j.gastro.2016.12.032. [ Links ]
2. ASGE Standards of Practice Committee, Gurudu SR, Bruining DH, Acosta RD, Eloubeidi MA, Faulx AL, et al. The role of endoscopy in the management of suspected small-bowel bleeding. Gastrointest Endosc. 2017;85(1):22-31. doi: 10.1016/j.gie.2016.06.013. [ Links ]
3. Maeda Y, Moribata K, Deguchi H, Inoue I, Maekita T, Iguchi M, et al. Video capsule endoscopy as the initial examination for overt obscure gastrointestinal bleeding can efficiently identify patients who require double-balloon enteroscopy. BMC Gastroenterol. 2015;15:132. doi: 10.1186/s12876-015-0362-7. [ Links ]
4. Galiano MT, Sánchez F, Pineda LF. Experiencia clínica del uso de la videocápsula endoscópica en el diagnóstico de patología del intestino delgado. Rev Col Gastroenterol. 2009;24(1):17-25. [ Links ]
5. Juliao F, Muñoz E, Yepes C. Diagnostic performance of capsule endoscopy and findings from patients with obscure gastrointestinal bleeding at the Hospital Pablo Tobon Uribe in Medellin, Colombia. Rev Col Gastroenterol. 2013;28(2):109-17. [ Links ]
6. Pennazio M, Spada C, Eliakim R, Keuchel M, May A, Mulder CJ, et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2015;47(4):352-76. doi: 10.1055/s-0034-1391855. [ Links ]
7. Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015;110(9):1265-87; quiz 1288. doi: 10.1038/ajg.2015.246. [ Links ]
8. Yung DE, Koulaouzidis A, Avni T, Kopylov U, Giannakou A, Rondonotti E, et al. Clinical outcomes of negative small-bowel capsule endoscopy for small-bowel bleeding: a systematic review and meta-analysis. Gastrointest Endosc. 2017;85(2):305-317.e2. doi: 10.1016/j.gie.2016.08.027. [ Links ]
9. Van de Bruaene C, Hindryckx P, De Looze D. Capsule endoscopy in obscure GI bleeding: better to be negative, but let us not be too positive. Gastrointest Endosc. 2017;86(3):574-5. doi: 10.1016/j.gie.2017.04.012. [ Links ]
10. Teshima CW, Kuipers EJ, van Zanten SV, Mensink PB. Double balloon enteroscopy and capsule endoscopy for obscure gastrointestinal bleeding: an updated meta-analysis. J Gastroenterol Hepatol. 2011;26(5):796-801. doi: 10.1111/j.1440-1746.2010.06530.x. [ Links ]
11. Van Assche G, Dignass A, Panes J, Beaugerie L, Karagiannis J, Allez M, et al. The second European evidence-based Consensus on the diagnosis and management of Crohn’s disease: Definitions and diagnosis. J Crohns Colitis. 2010 Feb;4(1):7-27. doi: 10.1016/j.crohns.2009.12.003. [ Links ]
12. Dionisio PM, Gurudu SR, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, et al. Capsule endoscopy has a significantly higher diagnostic yield in patients with suspected and established small-bowel Crohn’s disease: a meta-analysis. Am J Gastroenterol. 2010;105(6):1240-8; quiz 1249. doi: 10.1038/ajg.2009.713. [ Links ]
13. Adler SN, Yoav M, Eitan S, Yehuda C, Eliakim R. Does capsule endoscopy have an added value in patients with perianal disease and a negative work up for Crohn’s disease? World J Gastrointest Endosc. 2012;4(5):185-8. doi: 10.4253/wjge.v4.i5.185. [ Links ]
14. Gomollón F, Dignass A, Annese V, Tilg H, Van Assche G, Lindsay JO, et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 1: Diagnosis and Medical Management. J Crohns Colitis. 2017;11(1):3-25. doi: 10.1093/ecco-jcc/jjw168. [ Links ]
Received: March 11, 2018; Accepted: June 01, 2018











 text in
text in