Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.4 Bogotá oct./dic. 2018
https://doi.org/10.22516/25007440.313
Review articles
Surgical risk assessment in patients with liver cirrosis
1Hepatólogo, Unidad de Hepatología y Trasplante Hepático, Hospital Pablo Tobón Uribe. Medellín, Colombia
Cirrhotic patients may require surgical procedures and face higher morbidity and mortality than the general population. Adverse results are associated with multiple factors, but the most important are the severity of the liver disease, the urgency of the procedure and the type of surgery. The Child-Turcott-Pugh score (CTP) and the MELD score can be used to determine the severity of liver disease and to stratify the risk. Patients with CTP A are considered to tolerate elective surgery well, and surgery is permissible in patients with CTP B or MELD <14 with good preoperative preparation. It is contraindicated in patients with CTP C or MELD> 15 with albumin <2.5 gr/dL. Ideally, elective, minimally invasive procedures are used in specialized centers with doctors trained in the care of this type of patient. Preoperative optimization after risk stratification and careful management are mandatory before and after surgery. A multidisciplinary, individualized and specialized approach can improve results.
Keywords: Surgical risk; cirrhosis; surgery; results; Child; MELD
Los pacientes cirróticos pueden requerir procedimientos quirúrgicos y están relacionados con mayor morbimortalidad que la población general. Los resultados adversos están asociados con múltiples factores, pero los más importantes son la severidad de la enfermedad hepática, la urgencia del procedimiento y el tipo de cirugía. El puntaje Child-Turcott-Pugh (CTP) y el puntaje MELD pueden ser usados para determinar la severidad de la enfermedad hepática y estratificar el riesgo. Se considera que la cirugía electiva se tolera bien en pacientes con CTP A, es permisible con una buena preparación preoperatoria en pacientes con CTP B o MELD <14 y está contraindicada en pacientes con CTP C o MELD >15 con albúmina <2,5 g/dL. Lo ideal son procedimientos electivos, mínimamente invasivos y que sean realizados en centros especializados y con médicos entrenados en el cuidado de este tipo de pacientes. La optimización preoperatoria después de la estratificación del riesgo y un cuidadoso manejo son obligatorios antes y después de la cirugía. Una aproximación multidisciplinaria, individualizada y especializada puede mejorar los resultados.
Palabras clave: Riesgo quirúrgico; cirrosis; cirugía; resultados; Child; MELD
Introduction
Surgical procedures in patients with liver disease carry significant risks of complications that can be serious and can generate high rates of morbidity and mortality. The magnitude of the surgical risk depends on factors that include severity of the liver disease, type and location of surgical procedure, the degree of urgency, the type of anesthesia, and comorbidities. 1 Although hepatic resection of tumors and liver transplantation are the main types of surgery for cirrhotic patients, these patients frequently need other types of surgical procedures. In addition, the number of patients diagnosed with cirrhosis has been increasing in recent years.
Classically, the the Child-Turcott-Pugh score (CTP) has been used to evaluate surgical risk facing these patients. The average risk of death of a cirrhotic patient who undergoes abdominal surgery is said to be from 11% to 28% compared to 1% for non-cirrhotic patients. 2,3 However, depending on patients’ CTP scores, 30-day mortality rates can be as high as 80%. 4,5 These percentages remain high despite improvement in recent years. In addition, most studies of this topic have limitations. They are either retrospective, have few patients, and/or the majority of patients are CTP A cirrhotic patients for whom results and application of evidence must be taken with caution.
The objective of this article is to review strategies for assessing surgical risk and management of cirrhotic patients who face non-hepatic surgical procedures.
Effects of anesthesia and surgery on the liver
Liver disease can significantly alter the distribution, metabolism and excretion of anesthetics and some medications used during surgery. The hepatotoxic potential of halothane, which can generate acute immunoallergic hepatitis which can become acute hepatic failure, is widely known. 6 Other anesthetic agents such as isoflurane, desflurane and sevoflurane which have minimal hepatic effects on patients with liver disease should be chosen. The use of propofol is also possible because of its short half-life. Caution should also be exercised with opiates and benzodiazepines such as morphine, oxycodone, diazepam and midazolam, since they are metabolized very slowly in patients with liver disease which carries the consequent risk of prolonged neurological depression and precipitation of hepatic encephalopathy. If the use of this type of agents is necessary, remifentanil and oxazepam are recommended. Among the muscle relaxants, atracurium and cisatracurium are preferred because elimination does not depend on the liver or the kidneys.
When possible, regional anesthesia should be chosen. Slight changes in liver biochemical tests are frequent after surgery but have no impact on residual liver function. 7
Cirrhotic patients are characterized by hyperdynamic circulation with increased cardiac output and decreased systemic vascular resistance. During surgery, anesthetic agents can reduce hepatic blood flow by 30% to 50% after induction. Episodes of hypotension and hemorrhaging occur frequently, so the use of vasoactive drugs is also frequent. These lead to significant decreases in hepatic perfusion and make the cirrhotic liver more susceptible to hypoxic-ischemic injury. In addition, patients with advanced liver disease may have severe ascites, hepatic hydrothorax, portopulmonary hypertension, and hepatopulmonary syndrome. All of these factors are relevant to hypoxemia and difficulty in mechanical ventilation of these individuals.
Surgical risk evaluation
Evaluation of surgical risk for patients with liver cirrhosis is based on three main factors: liver function, urgency of the procedure, and type of procedure. Cirrhotic patients’ high surgical risk are not only due to cirrhosis itself, but also to coagulopathy, malnutrition, immune dysfunction, cardiomyopathy of cirrhosis, pulmonary alterations, and renal alterations. In addition, the most important American study of surgical risk in elective procedures determined that clinically significant portal hypertension including esophageal varices, ascites, and encephalopathy is the main factor related to mortality, morbidity, length of hospital stays and costs. 8
Contraindications for surgery are considered to be acute hepatitis, especially if it is severe (international normalized index INR >1,5); alcoholic hepatitis; and acute liver failure for which mortality of 10% to 50% has been described. It has been determined that when major emergency surgery (ASA V) is necessary, mortality is 50% to 100%. Since mortality rates are so much higher than for elective procedures, major emergency surgery must be discussed with the patient, the family and the surgical team. When a patient’s CTP score is C, it is a contraindication for all major surgical procedures.
The presurgical evaluation must include the classification of the American Society of Anesthesiology (ASA). Compensated cirrhosis is classified as ASA III while decompensated cirrhosis is classified as ASA IV, so from the beginning the surgical risk is considerable. A Mayo Clinic study found that the ASA classification was the best predictor of 7-day postoperative mortality especially it is combined with age (> 70 years) and MELD score. 9 The results of that study have been used to create an online tool to help clinicians more precisely determine the risk of postoperative mortality in major abdominal, cardiac, vascular and orthopedic surgery. It can be accessed at the following link: https://www.mayoclinic.org/medical-professionals/model-end-stage-liver-disease/medical-professionals/transplant-medicine/calculators/post-operative-mortality-risk-in-patients-with-cirrhosis/itt-20434721
The CTP and MELD scores are prognostic models used to assess liver disease severity and stratify risk. In studies up to the 1990s, postoperative mortality rates were 10%, 30%, and 76% to 82% for CTP A, B, and C patients, respectively. 4,5 Nevertheless, the accuracy of the CTP score is not the best because it includes subjective variables such as ascites and hepatic encephalopathy. In recent years, better results have been reported. One recent study reported 2% mortality in CTP A patients and 12% in CTP B and C patients for abdominal surgery such as cholecystectomy, herniorrhaphy and colectomy. Still, it should be noted that the patients were carefully selected, and procedures were performed by surgeons who are trained for interventions in patients with portal hypertension. 10 According to these results, patients with CTP A have no problem with elective surgery, CTP C patients have contraindications for surgical procedures and CTP B patients may undergo surgery, but they require rigorous pre-surgical evaluations and better decision-making tools.
The MELD score is a statistical model that was created to evaluate mortality related to placement of transjugular intrahepatic portosystemic shunts (TIPS). Subsequently, it has been applied to prioritize patients on the liver transplantation waiting list. 11 In recent years it has become a fundamental tool for stratification of patients with liver diseases in various scenarios. Studies comparing MELD scores with CTP scores have found that MELD predicts unfavorable outcomes with significant risk starting with MELD scores over 10 better than does CTP, and that MELD cutoffs of 14 or 15 are more specific. 10,12 A recent study found that patients with MELD scores over 15 and albumin levels less than 2.5 g/L had a mortality rate of 60% versus 14% for other patients. Accuracy of predication of this combination of indicators was superior to the CTP score. 10 In addition, MELD has been the best predictor of postoperative mortality at 30 and 90 days (Table 1). 9 According to these studies, it is considered that patients with MELD <10 can undergo surgical procedures without major problems, surgery is contraindicated for those with MELD> 15 and albumin <2.5 g/L, and patients with MELD scores from 10 to 15 may undergo surgery in specialized centers after strict evaluation.
Table 1 Relationship between MELD score and postoperative mortality
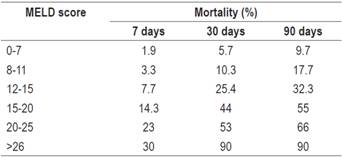
Taken from: Teh SH et al. Gastroenterology 2007; 132 (4): 1261-9.
Comorbidities are important, especially kidney failure, cardiovascular disease and diabetes mellitus.
Type of procedure
Minimally invasive procedures should be used for cirrhotic patients who need surgery. In the past it was considered that laparoscopy was contraindicated for cirrhotic patients, but this has been reevaluated, and this approach should be considered whenever possible. Some authors have modified the technique to avoid complications. An example is changing the location of the trocar to avoid inadvertent perforation of varicose veins in the abdominal wall. Sufficient experience and studies now exist in laparoscopic cholecystectomy, 13,14, herniorrhaphy, splenectomies, colectomies, gastric bypasses and appendectomies, among others. 15 In any case, it should be recognized that laparoscopic procedures have greater possibilities of becoming open surgery in cirrhotic patients, and when it does it requires more surgical time and has more bleeding than do procedures on patients without cirrhosis.
Abdominal surgery
More information is available the most frequent types of surgery which, in the case of patients with cirrhosis, are abdominal operations. Laparoscopic procedures and instruments that facilitate coagulation such as the harmonic scalpel are preferred. Minimally invasive procedures decrease mortality and morbidity rates, and the frequency of infections, wound dehiscence, and bleeding while shortening surgical time and hospital stays.
Cirrhotic patients have a higher incidence of cholelithiasis than does the general population; Fortunately, most cases remain asymptomatic and do not need surgical management. For CTP A and B cirrhotic patients who undergo laparoscopic cholecystectomies, morbidity is 5% to 10% and mortality is less than 2%. Coexistence of cardiovascular disease is the main risk factor associated with mortality. 16 In contrast, CTP C cirrhotic patients have a prohibitive mortality rate, so management with antibiotics is recommended in cases of acute cholecystitis. In cases of empyema of the gallbladder, a percutaneous cholecystectomy may be required. 17
Abdominal wall hernias are four times more frequent in cirrhotic patients than in the general population, and occur even more often in patients who have ascites. In a study of more than 900 CPT A and B cirrhotic patients, the overall mortality rate was 5.7% for surgical management of inguinal hernia, with acceptable morbidity and a recurrence rates of 8%. 18 The results for umbilical hernias were similar, but in the case of urgent procedures, the mortality rate was five times higher than that of the elective procedure. In recent reports, mortality has been 0% in referral centers with great experience and well selected patients. Umbilical herniorrhaphy frequently requires the use of meshes, but it must be taken into account some studies have found them to be associated with higher infection rates.
A mortality rate of 13% to 35% with a morbidity rate of 50% has been reported for colorectal surgery. Factors related to poor prognosis are CTP B and C scores and urgent surgery due to intestinal obstruction, bleeding or perforation. 19 For urgent treatment of intestinal obstruction, a colonic stent might be the best choice while endoscopic management of bleeding due to an ulcer or tumor should be considered. In the case of gastrectomy, the mortality rate is 14% to 29% with a morbidity rate of 53% for CTP A cirrhotic patients and 68% for CTP B patients. 8
Cardiac and vascular surgery
The mortality rate for elective cardiac surgery for CTP A cirrhotic patients is 0% -11%, for CTP B it is 18% -67%, and for CTP C it is 67% -100%. The respective morbidity rates are 25% -50%, 50% -100% and 100%. 20 Accordingly, well selected CTP A cirrhotic patients can be considered for elective surgery even procedures which use cardiopulmonary bypass, but the surgical risk for CTP B and C patients is prohibitive. Other predictors of mortality are age> 60 years, female sex, ascites and congestive heart failure. The mortality rate is over 50% for patients with two or more of these factors.
Repairing aneurysms of the abdominal aorta is possible in CTP A cirrhotic patients, but these patients have greater need for transfusions, longer surgical time, longer hospital stays and higher costs than do patients without cirrhosis. 21 Cirrhotic patients with CTP B or MELD> have high risks of morbidity and mortality.
Orthopedic surgery and trauma
Cirrhotic patients who undergo major elective orthopedic hip or knee surgery have a morbidity rate of over 25% and mortality rates of 4%, 14% and 100% for CTP A, B and C patients, respectively. Nevertheless, the results are significantly better than results for emergency procedures whose morbidity rate is over 80% and whose mortality rate can reach 60%. 22
Cirrhotic patients with trauma have twice the mortality rate as do non-cirrhotic patients with trauma. In addition, patients with closed abdominal trauma requiring emergency laparotomy and whose MELD scores are over 17 have a postoperative mortality rate of 85%. 23
Perioperative care
Cirrhotic patients are a special group of patients that require preoperative, intraoperative and postoperative care in order for surgical procedures to achieve favorable results. The preoperative assessment is essential for identifying whether a patient has had complications in the past, treatment received in the past, and whether the patient is currently suffering from decompensation.
Management of all cirrhotic patients who undergo surgery must be optimized, and complications must be controlled effectively (Table 2).
Although cirrhotic patients’ traditional coagulation tests often have abnormal results, it has been demonstrated that the balance of coagulation is rebalanced in these patients. This explains the fact that they even have thrombotic events. This type of alteration should not be a contraindication for surgery. The ideal evaluation of platelet function and coagulation in cirrhotic patients is the use of dynamic and global tests such as thromboelastography (TEG). A recent study that valuated TEG to define a transfusion strategy guided for invasive procedures determined that the use of TEG reduced the need for transfusions by 90% without increasing the number or frequency of bleeding complications. 24 Additional studies are expected to validate this information.
Thrombocytopenia is almost universal in patients with liver cirrhosis. Presurgical transfusions are indicated when the platelet count is <50,000 platelets/μL and can be considered for high risk surgery with high risks of bleeding when a patient’s count is between 50,000 and 80,000 platelets/μL. In cirrhotic patients with renal insufficiency, the presurgical administration of desmopressin should be considered. Eltrombopag, which is related to increased platelet counts and decreased need for transfusions, has been associated with portal thrombotic events so is not recommended. 25 There are no appropriate studies that evaluate the results of transfusions of fresh frozen plasma in cirrhotic patients prior to surgery. In general terms it is transfused when the INR is over 1.5. An economical and safe strategy is administration of 10 mg/day of vitamin K for three days to correct vitamin K deficiency which is common among cirrhotic patients. Although there is no specific hemoglobin goal for cirrhotic patients prior to surgery, a restrictive strategy that avoids excess transfusions is recommended because they are related to increased portal pressure and greater bleeding.
TIPS can control portal hypertension thereby improving postsurgical results for cirrhotic patients. The main indication is the presence of ascites or esophageal varices in patients who require abdominal surgery and whose MELD scores are below fifteen. Studies have shown that patients can undergo major surgery such as oncological resections with curative intent and have had less bleeding, transfusions and postoperative ascites with acceptable survival rates at medium-term follow-up. 26
Both the excesses and the deficits of intravenous fluids should be avoided in the postoperative period since excesses are related to edema and ascites, and deficits are related to renal failure. Ascites in cirrhotic patients recurs almost universally following abdominal surgery, fistulas of ascitic fluid are not rare, and there is a high risk of surgical wound dehiscence. Consequently, the early use of diuretics is recommended, paracentesis should be performed as needed, and prolonged use of abdominal drains should be avoided to reduce the risk of infections, hypovolemia and malnutrition. In these cases, albumin is very useful because of its oncotic, immunoregulatory, and antioxidant properties as well as its capacity to transport substances and drugs. The use of opiates and benzodiazepines should be avoided in order to reduce the risk of encephalopathy. Together with the use of lactulose, it can help guarantee a sufficient number of stools. Polyethylene glycol can be used in patients who are intolerant to lactulose. Infections frequently develop in cirrhotic patients following surgery, so it is necessary for medical staff to be hyper-vigilant in monitor for them and diagnosing them. The most frequent foci of infections are in the abdominal cavity, the urinary tract and lungs. Spontaneous bacteremia is also common.
Cirrhotic patients are often malnourished and require nutritional support before and after surgery. Oral feeding should be started as soon as possible. A low sodium diet with a caloric requirement of 30-35 kcal/kg/day and a protein intake of 1.2-1.5 g/kg/day is recommended. In addition, early mobilization, respiratory incentive therapy and early initiation of prophylaxis against deep vein thrombosis should be promoted.
Conclusions
Patients with liver cirrhosis, especially those with portal hypertension, have higher surgical risks than those of the general population. When a cirrhotic patient requires surgery, a thorough evaluation by the clinician is necessary to determine liver function, urgency of treatment, and type of procedure. With this knowledge a decision can be made about how to proceed. If surgery is chosen, this knowledge can be used guarantee the necessary perioperative measures to increase the success of surgical procedures.
REFERENCES
1. Friedman LS. The risk of surgery in patients with liver disease. Hepatology. 1999;29(6):1617-23. doi: 10.1002/hep.510290639. [ Links ]
2. Neeff H, Mariaskin D, Spangenberg HC, Hopt UT, Makowiec F. Perioperative mortality after non-hepatic general surgery in patients with liver cirrhosis: an analysis of 138 operations in the 2000s using Child and MELD scores. J Gastrointest Surg. 2011;15(1):1-11. doi: 10.1007/s11605-010-1366-9. [ Links ]
3. Aranha GV, Sontag SJ, Greenlee HB. Cholecystectomy in cirrhotic patients: a formidable operation. Am J Surg. 1982;143(1):55-60. [ Links ]
4. Garrison RN, Cryer HM, Howard DA, Polk HC Jr. Clarification of risk factors for abdominal operations in patients with hepatic cirrhosis. Ann Surg. 1984;199(6):648-55. [ Links ]
5. Mansour A, Watson W, Shayani V, Pickleman J. Abdominal operations in patients with cirrhosis: still a major surgical challenge. Surgery. 1997;122(4):730-5. [ Links ]
6. Walton B, Simpson BR, Strunin L, Doniach D, Perrin J, Appleyard AJ. Unexplained hepatitis following halothane. Br Med J. 1976;1(6019):1171-6. [ Links ]
7. O’Leary JG, Yachimski PS, Friedman LS. Surgery in the patient with liver disease. Clin Liver Dis. 2009;13(2):211-31. doi: 10.1016/j.cld.2009.02.002. [ Links ]
8. Csikesz NG, Nguyen LN, Tseng JF, Shah SA. Nationwide volume and mortality after elective surgery in cirrhotic patients. J Am Coll Surg. 2009;208(1):96-103. doi: 10.1016/j.jamcollsurg.2008.09.006. [ Links ]
9. Teh SH, Nagorney DM, Stevens SR, Offord KP, Therneau TM, Plevak DJ, et al. Risk factors for mortality after surgery in patients with cirrhosis. Gastroenterology. 2007;132(4):1261-9. doi: 10.1053/j.gastro.2007.01.040. [ Links ]
10. Telem DA, Schiano T, Goldstone R, Han DK, Buch KE, Chin EH, et al. Factors that predict outcome of abdominal operations in patients with advanced cirrhosis. Clin Gastroenterol Hepatol. 2010;8(5):451-7, quiz e58. doi: 10.1016/j.cgh.2009.12.015. [ Links ]
11. Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31(4):864-71. doi: 10.1053/he.2000.5852. [ Links ]
12. Befeler AS, Palmer DE, Hoffman M, Longo W, Solomon H, Di Bisceglie AM. The safety of intra-abdominal surgery in patients with cirrhosis: model for end-stage liver disease score is superior to Child-Turcotte-Pugh classification in predicting outcome. Arch Surg. 2005;140(7):650-4. doi: 10.1001/archsurg.140.7.650. [ Links ]
13. Yeh CN, Chen MF, Jan YY. Laparoscopic cholecystectomy in 226 cirrhotic patients. Experience of a single center in Taiwan. Surg Endosc. 2002;16(11):1583-7. doi: 10.1007/s00464-002-9026-0. [ Links ]
14. Cucinotta E, Lazzara S, Melita G. Laparoscopic cholecystectomy in cirrhotic patients. Surg Endosc. 2003;17(12):1958-60. doi: 10.1007/s00464-002-8852-4. [ Links ]
15. Cobb WS, Heniford BT, Burns JM, Carbonell AM, Matthews BD, Kercher KW. Cirrhosis is not a contraindication to laparoscopic surgery. Surg Endosc. 2005;19(3):418-23. doi: 10.1007/s00464-004-8722-3. [ Links ]
16. Bloch RS, Allaben RD, Walt AJ. Cholecystectomy in patients with cirrhosis. A surgical challenge. Arch Surg. 1985;120(6):669-72. [ Links ]
17. Byrne MF, Suhocki P, Mitchell RM, Pappas TN, Stiffler HL, Jowell PS, et al. Percutaneous cholecystostomy in patients with acute cholecystitis: experience of 45 patients at a US referral center. J Am Coll Surg. 2003;197(2):206-11. [ Links ]
18. Hurst RD, Butler BN, Soybel DI, Wright HK. Management of groin hernias in patients with ascites. Ann Surg. 1992;216(6):696-700. [ Links ]
19. Gervaz P, Pak-art R, Nivatvongs S, Wolff BG, Larson D, Ringel S. Colorectal adenocarcinoma in cirrhotic patients. J Am Coll Surg. 2003;196(6):874-9. doi: 10.1016/S1072-7515(03)00117-0. [ Links ]
20. Modi A, Vohra HA, Barlow CW. Do patients with liver cirrhosis undergoing cardiac surgery have acceptable outcomes? Interact Cardiovasc Thorac Surg. 2010;11(5):630-4. doi: 10.1510/icvts.2010.241190. [ Links ]
21. Marrocco-Trischitta MM, Kahlberg A, Astore D, Tshiombo G, Mascia D, Chiesa R. Outcome in cirrhotic patients after elective surgical repair of infrarenal aortic aneurysm. J Vasc Surg. 2011;53(4):906-11. doi: 10.1016/j.jvs.2010.10.095. [ Links ]
22. Cohen SM, Te HS, Levitsky J. Operative risk of total hip and knee arthroplasty in cirrhotic patients. J Arthroplasty. 2005;20(4):460-6. doi: 10.1016/j.arth.2004.05.004. [ Links ]
23. Lin BC, Fang JF, Wong YC, Hwang TL, Hsu YP. Management of cirrhotic patients with blunt abdominal trauma: analysis of risk factor of postoperative death with the Model for End-Stage Liver Disease score. Injury. 2012;43(9):1457-61. doi: 10.1016/j.injury.2011.03.057. [ Links ]
24. De Pietri L, Bianchini M, Montalti R, De Maria N, Di Maira T, Begliomini B, et al. Thrombelastography-guided blood product use before invasive procedures in cirrhosis with severe coagulopathy: A randomized, controlled trial. Hepatology. 2016;63(2):566-73. doi: 10.1002/hep.28148. [ Links ]
25. Afdhal NH, Giannini EG, Tayyab G, Mohsin A, Lee JW, Andriulli A, et al. Eltrombopag before procedures in patients with cirrhosis and thrombocytopenia. N Engl J Med. 2012;367(8):716-24. doi: 10.1056/NEJMoa1110709. [ Links ]
26. Lahat E, Lim C, Bhangui P, Fuentes L, Osseis M, Moussallem T, et al. Transjugular intrahepatic portosystemic shunt as a bridge to non-hepatic surgery in cirrhotic patients with severe portal hypertension: a systematic review. HPB (Oxford). 2018;20(2):101-109. doi: 10.1016/j.hpb.2017.09.006. [ Links ]
Received: January 29, 2018; Accepted: November 06, 2018











 texto en
texto en 



