Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.4 Bogotá oct./dic. 2018
https://doi.org/10.22516/25007440.169
Case reports
Case report of robot-assisted esophageal enucleation of leiomyoma and literature review
1Cirujano de tórax, Clínica Marly y Universidad El Bosque. Bogotá D. C., Colombia
2Fellow de cirugía de tórax, Universidad El Bosque. Bogotá D. C., Colombia
3Residente de cirugía general, Universidad El Bosque. Bogotá D. C., Colombia
Introduction:
Esophageal leiomyomas are benign tumors which are resected by esophageal enucleation when they are symptomatic, suspected of malignancy, or larger than 5 cm. Traditional resection uses the open enucleation technique, but minimally invasive surgery has emerged as a technique that has great advantages, especially when combined with robotic technology.
Case report:
We report a case of leiomyoma of the middle esophagus with treated with enucleation using a robotic-assisted thoracoscopic technique. Intraoperative esophagoscopy and transillumination were useful for identifying the esophagus and developing a plan of safe extra mucosal dissection. Together with robotic assistance this seems to minimize intraoperative risks including that of mucosal injury while also improving postoperative recovery time.
K Esophageal leiomyoma; benign tumor; robotics; enucleation; minimally invasive surgery
Introducción:
los leiomiomas esofágicos son tumores benignos, que son resecados por enucleación esofágica cuando son mayores de 5 cm o en lesiones de cualquier tamaño que sean sintomáticos o sospechosos de malignidad. Tradicionalmente, se ha realizado la resección por técnica de enucleación abierta; sin embargo, la cirugía mínimamente invasiva ha surgido como una técnica con grandes ventajas y, en especial, la tecnología robótica parece ofrecer ventajas.
Caso clínico:
se reporta un caso de leiomioma esofágico del esófago medio con enucleación mediante el uso de una técnica toracoscópica asistida por robot. La esofagoscopia intraoperatoria y la transiluminación fueron complementos útiles para identificar el esófago y desarrollar un plano de disección extramucosa seguro, que junto con la asistencia robótica parecen minimizar los riesgos intraoperatorios, entre ellos, potencialmente la probabilidad de lesión mucosa, y mejoran el tiempo de recuperación postoperatoria.
Palabras clave: Leiomioma esofágico; tumor benigno; robótica; enucleación; cirugía mínimamente invasiva
Introduction
All gastrointestinal stromal tumors (GISTs) should be considered potentially malignant. 1 Leiomyomata account for more than 80% of the seldom seen benign tumors of the esophagus. 2. They originate in the circular muscle layer of the distal esophagus, middle esophagus and, most commonly, of the gastroesophageal junction. Dimensions that have been reported in the literature range from 1 cm to 29 cm, and they are ideal for organ preservation surgery. Esophageal leiomyomata have been conventionally resected by open thoracotomy, but emergent techniques including robot-assisted procedures are becoming more and more common. Robot-assisted procedures have the benefit of 3D imaging which can reduce the risk of perforating the esophageal mucosa and improve dissection of structures. These advantages will no doubt become even more important in the future. 3 We present a case of enucleation of an esophageal leiomyoma by robot-assisted surgery with intraoperative transillumination with esophagoscopy which facilitated safe dissection of the extramucosal plane and achieved organ preservation.
Clinical case
The patient was 41-year-old woman who had suffered from dysphagia since 2013. A chest CT scan revealed a 4.1 cm esophageal lesion (Figures 1A and 1B). In 2013, an attempt had been made to resect this lesion by thoracoscopy in another institution. However, it became a thoracotomy due to a mediastinal tumor that compromised the wall of the thoracic esophagus. Biopsies compatible with smooth muscle fascicles were taken without finding nuclear pleomorphism or mitosis. Necrosis was histopathologically compatible with a benign leiomyoma of the esophagus but there was no immunohistochemistry confirmation. In 2017, due to the persistence of dysphagia, an esophagogram registered a 4.1 cm lesion that altered esophageal transit (Figure 1C). Presence of a submucosal mass was confirmed by endoscopic ultrasonography (Figure 1D). It measured approximately 3.6 cm on its major axis along the anterior wall of the esophagus in the upper thorax inferior to the azygos vein and appeared to be a hypovascular mass without paraesophageal adenopathies. Resection of the tumor was considered necessary due to its size.
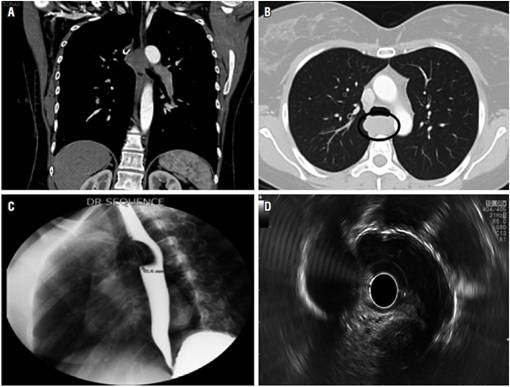
Figure 1 A and 1B. Chest tomography with contrast showing a 4.1 centimeter heterogeneous esophageal. 1C. Esophagogram showing a filling defect in the esophagus with an intact smooth mucosal surface. 1D. Endoscopic ultrasonography of the esophagus showing a well-circumscribed hypoechoic mass originating in the muscularis propria.
With the patient under general anesthesia and in left lateral decubitus position, a double lumen tube was used to isolate the right lung. Then, an 8-mm robot trocar was placed into the middle axillary line above the fifth rib, and a camera was placed into this trocar while other ports were placed under direct view. Next, an 8 mm robot trocar was placed 1 cm lateral to the spinal column at the eighth rib. A third 8-mm robot trocar was placed 8 cm from the last trocar on the eighth rib. A 12 mm port was then placed 8 cm from the last trocar on the eighth rib near the posterior axillary line. Finally, a 12 mm trocar was placed 8 cm below the chamber port on the diaphragm. The robot was then coupled with robot arms connected to wrist-type articulation instruments which allow freedom of movement for surgical instruments with more than 3 axes. We used grasper forceps, curved dissectors, blunt tip dissectors and anvil forceps for resection.
The tumor was identified on the side of the head of the azygos arch through the mediastinal pleura (Figure 2A). The mediastinal pleura, the adventitia of the esophagus and the muscularis propria were sectioned longitudinally to expose the tumor capsule (Figure 2B). The tumor appeared to arise mainly from the muscular lamina of the mucosa. A round, hard, elastic tumor was successfully enucleated by nearly blunt dissection without damaging the mucosa (Figure 2C). After enucleation of the tumor, the mediastinal pleura, the adventitia of the esophagus and the muscularis propria of the esophagus were closed with continuous sutures (Figure 2D). Then a chest tube was placed.
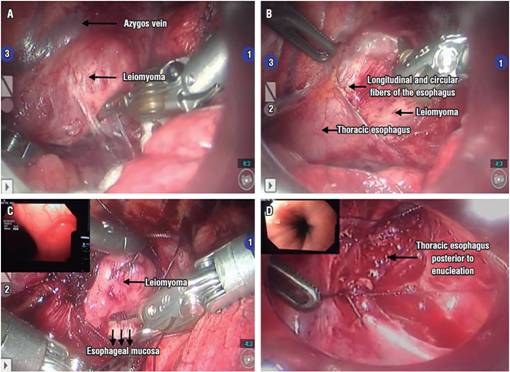
Figure 2A Image of the leiomyoma covered by mediastinal pleura of the esophagus before dissection. 2B and 2C. View of the leiomyoma after dissection with esophagoscopic inspection during surgery, ensuring complete excision of the tumor and D. mucosal integrity after enucleation with endoscopic guidance.
On the day after surgery, the chest tube was removed, an esophagogram showed intact smooth esophageal mucosa without leakage or stenosis (Figure 3A), and the patient started oral food intake. The patient’s development was favorable, and was she discharged 24 hours after surgery. Histopathological examination of the resected specimen (Figures 3B and C) showed spindle-shaped tumor cells which were positive for diffuse desmin but negative for DOG-1, c-KIT, CD34 and S100. The final pathological diagnosis was leiomyoma of the esophagus without evidence of malignancy.

Figure 3A Postoperative esophagogram with evidence of integrity of the thoracic esophagus, without evidence of stenosis, and without evidence of fistulas. 3B. Surgical part of the leiomyoma after enucleation revealing a 4 cm mass with an intact pseudocapsule. 3C. Microscopic view of the tumor (insertion H/E x 200).
Discussion
All GISTs are potentially malignant, 1 and leiomyomata are the most common benign mesenchymal tumors. They account for more than 80% of benign esophageal tumors and can occur at any age. Their peak incidence occurs between the third and fifth decade of life. Usually located in the middle or lower third of the esophagus, 2 they are intramural, slow-growing tumor, and usually measure less than 5 cm. 3 Half of those affected are asymptomatic, the most frequent symptoms are dysphagia and epigastric discomfort, 4 but regurgitation, upper gastrointestinal bleeding and weight loss can also occur. 5
Once a leiomyoma is suspected, esophagogastroscopy combined with endoscopic ultrasonography of the tumor is mandatory to exclude esophageal cancer. Typically, GISTs and leiomyomata are homogeneous and hypoechoic lesions with clear margins that originate in the lamina propria or mucosa. They can be easily differentiated from other benign lesions of the esophagus such as hyperechoic lipomas. 6-16 Some reports identify calcifications in 1.8% of the tumors because this characteristic seems to be exclusive to esophageal leiomyomata. 7. In addition, computerized axial tomography (CAT) gives characteristics of possible benignity or malignancy but does not exclude the possibility of malignancy which requires histological and immunohistochemical assessment. 8
A biopsy of the esophageal mass must be performed preoperatively to distinguish between GIST and esophageal leiomyoma, although the guidelines of the National Comprehensive Cancer Network (NCCN) do not suggest preoperative biopsy of resectable masses. GISTs can be soft and fragile, and a biopsy can cause hemorrhaging which increases the risk of dissemination of the tumor following rupture of the pseudocapsule. Even submucosal localization and fine needle aspiration (FNA) may be insufficient to differentiate between the leiomyoma and the malignant variant of GIST. 1 Management options are based on the size of the lesions. For lesions measuring less than 2 cm and for asymptomatic lesions, no consensus has yet been established regarding surgery or the best treatment method.
Some researchers recommend evaluation by endoscopic ultrasound every one or two years. The reasons for this approach are that leiomyomata are slow-growing tumors, malignant transformation is extremely rare, and surgical trauma can be more damaging to the patient. 9 Nevertheless, when lesions are larger than five cm or have become symptomatic regardless of size, the tumor should be resected, and surgical enucleation should be considered. 10 Our patient’s lesion measured only 4.1 cm lesion, but it was symptomatic. Management options for esophageal leiomyomata include thoracotomy enucleation, endoscopic enucleation, alcohol injection, video-assisted thoracoscopic enucleation, and robotic-assisted enucleation. Endoscopic submucosal tunnel dissection (ESTD) has also been developed for resection of submucosal tumors of the esophagus. 11 Nevertheless, the choice of tumor resection procedure depends on the skills of the surgeon, and there are no formal criteria for selecting the surgical approach. Even in cases of diffuse esophageal leiomyomata or giant esophageal leiomyomata, esophagectomy is often required. 6
Esophageal enucleation of open-ended leiomyomata was standard for benign tumors for a long time, but the appearance of minimally invasive approaches has reduced the occurrence of adverse effects such as pain and length of hospital stay. 7 These minimally invasive techniques are more demanding than open surgery due to two-dimensional vision, decreased coordination between the eyes and hands, and reduction of the degree of freedom for performing maneuvers. 5 For this reason, robot-assisted systems represent an improvement in minimally invasive thoracoscopic resection procedures for esophageal tumors. Dissection along vital structures such as the pulmonary vein, azygos vein, aorta or trachea can now be achieved with three-dimensional vision and improved coordination of the surgeon’s eyes and hands. These improvements reduce the risk of perforation of the esophageal mucosa. 8
In addition, intraoperative endoscopic guidance has become a useful tool for checking the integrity of the mucosa during enucleation which is important because the most frequent postoperative complication is laceration of the mucosa. Evidence of an intact mucosa allows an earlier start of oral feeding which is why some authors suggest that intraoperative esophagoscopy is essential for enucleation of benign submucosal tumors of the esophagus. It is a safe and accurate procedure which decreases risk of postoperative complications. 12-20
For all of these reasons, we decided to perform a robot-assisted procedure with intraoperative endoscopic guidance. Nevertheless, the disadvantage of this procedure is that it special equipment and a well-trained physician.
The robot-assisted approach has been associated with a lower incidence of mucosal injury. Robotic assisted thoracoscopy, particularly enucleation of benign esophageal tumors, can provide clearer distinctions between anatomical layers due to enlarged superior stereoscopic 3D vision which minimizes chances of a perforation of the esophageal mucosa and the mediastinum better than does videothoracoscopy (VATS). This helps eliminate surgical mortality and intraoperative blood loss thereby decreasing postoperative pain and leakage due to laceration of the mucosa leading to shorter hospital stays and faster reincorporation into daily activities. 14,18,19 The advantages become more pronounced when the lesion is towards the end of the upper thoracic esophagus towards the hiatus where vital structures are found. 13,14
Robot assisted esophageal surgery may revolutionize the field, but there studies and evidence supporting robotic approaches over other approaches are scarce. Of course, long surgical times and high costs of the this surgical approach are obstacles to wider acceptance. Additional research in the field of robotic enucleation of esophageal lesions is required before this technique can became the first line of approach instead of other minimally invasive techniques. 14,15,16,17,18 In our case, the patient was offered a robot-assisted approach due to the location of the lesion and the patient’s surgical history. There were no intraoperative or postoperative complications.
Preoperative differentiation between leiomyoma and GIST is difficult, as we have mentioned. Therefore, the evaluation of the postoperative surgical piece with hematoxylin eosin and postoperative immunohistochemistry is the gold standard for the diagnosis of all leiomyomata. These lesions are CD34 and CD117 negative, do not have c-KIT mutations, and are positive for desmin and smooth muscle actin (SMA) whereas GISTs are usually (though not always) negative. 6-17 GISTs present a different immunohistochemical pattern, and about 95% of GISTs are positive for c-KIT (CD117), 60% -70% for CD34, 30% -40% for SMA and 5% for S-100 protein. 1-15
To conclude, no clear method of patient follow-up after enucleation of benign esophageal tumors has yet been established. In some cases of GISTs, regular follow-up has been recommended based on the probability of recurrence due to findings from the surgical specimen. Unlike GISTs, other types of esophageal tumors such as leiomyoma recur very rarely, so periodic clinical follow-up rather than oncological follow-up may be sufficient. 11-21
Conclusions
Enucleation of esophageal leiomyomata with robotic assistance not only allows complete resection of a lesion, it also offers better exposure of structures, 3D vision, magnified images, and better coordination of the eyes and hands of the surgeon. Nevertheless, studies of the video-assisted thoracoscopy approach are lacking even though it has been established that this approach is feasible and effective for surgical treatment of leiomyomata of the esophagus.
REFERENCES
1. Jiang P, Jiao Z, Han B, Zhang X, Sun X, Su J, et al. Clinical characteristics and surgical treatment of oesophageal gastrointestinal stromal tumours. Eur J Cardiothorac Surg. 2010;38(2):223-7. doi: 10.1016/j.ejcts.2010.01.040. [ Links ]
2. Kernstine KH, Andersen ES, Falabella A, Ramirez NA, Anderson CA, Beblawi I. Robotic fourth-arm enucleation of an esophageal leiomyoma and review of literature. Innovations (Phila). 2009;4(6):354-7. doi: 10.1097/IMI.0b013e3181c46218. [ Links ]
3. DeUgarte DA, Teitelbaum D, Hirschl RB, Geiger JD. Robotic extirpation of complex massive esophageal leiomyoma. J Laparoendosc Adv Surg Tech A. 2008;18(2):286-9. doi: 10.1089/lap.2007.0067. [ Links ]
4. Choi SH, Kim YT, Han KN, Ra YJ, Kang CH, Sung SW, et al. Surgical management of the esophageal leiomyoma: lessons from a retrospective review. Dis Esophagus. 2011;24(5):325-9. doi: 10.1111/j.1442-2050.2010.01144.x. [ Links ]
5. Iscan Y, Tunca F, Senyurek YG, Tezelman S, Terzioglu T. Thoracoscopic enucleation of a giant leiomyoma of the esophagus. Surg Laparosc Endosc Percutan Tech. 2013;23(1):e32-4. doi: 10.1097/SLE.0b013e318275b2a3. [ Links ]
6. Markakis CG, Spartalis ED, Liarmakopoulos E, Kavoura EG, Tomos P. Esophageal gastrointestinal stromal tumor: diagnostic complexity and management pitfalls. Case Rep Surg. 2013;2013:968394. doi: 10.1155/2013/968394. [ Links ]
7. Macke RA, Luketich JD, Nason KS, Schuchert MJ. Minimally invasive enucleation of a large, extensively calcified esophageal leiomyoma. J Thorac Cardiovasc Surg. 2014;147(4):e52-4. doi: 10.1016/j.jtcvs.2013.12.054. [ Links ]
8. Elli E, Espat NJ, Berger R, Jacobsen G, Knoblock L, Horgan S. Robotic-assisted thoracoscopic resection of esophageal leiomyoma. Surg Endosc. 2004;18:713-6. doi: 10.1007/s00464-003-8829-y. [ Links ]
9. Luh SP, Hou SM, Fang CC, Chen CY. Video-thoracoscopic enucleation of esophageal leiomyoma. World J Surg Oncol. 2012;10:52. doi: 10.1186/1477-7819-10-52. [ Links ]
10. Khalaileh A, Savetsky I, Adileh M, Elazary R, Abu-Gazala M, Abu Gazala S, et al. Robotic-assisted enucleation of a large lower esophageal leiomyoma and review of literature. Int J Med Robot. 2013;9(3):253-7. doi: 10.1002/rcs.1484. [ Links ]
11. Li QY, Meng Y, Xu YY, Zhang Q, Cai JQ, Zheng HX, et al. Comparison of endoscopic submucosal tunneling dissection and thoracoscopic enucleation for the treatment of esophageal submucosal tumors. Gastrointest Endosc. 2017;86(3):485-491. doi: 10.1016/j.gie.2016.11.023. [ Links ]
12. Shin S, Choi YS, Shim YM, Kim HK, Kim K, Kim J. Enucleation of esophageal submucosal tumors: a single institution’s experience. Ann Thorac Surg. 2014;97(2):454-9. doi: 10.1016/j.athoracsur.2013.10.030. [ Links ]
13. Chen X, Xi Y, Wang H, Tan L. Minimally invasive surgery for giant esophageal leiomyoma: a case report & review of the literatures. J Thorac Dis. 2017;9(1):E26-E31. doi: 10.21037/jtd.2017.01.34. [ Links ]
14. Kumar A, Asaf BB. Robotic thoracic surgery: The state of the art. J Minim Access Surg. 2015;11(1):60-7. doi: 10.4103/0972-9941.147693. [ Links ]
15. Cho SY, Moon HJ, Kim JW, Cho SK, Kim BG, Joo SK, et al. Clinicopathologic feature of esophageal submucosal tumors treated by surgical approach. Korean J Gastroenterol. 2013;61(2):71-4. doi: 10.4166/kjg.2013.61.2.71. [ Links ]
16. How CH, Lee JM. The robotic approach for enucleation of a giant esophageal lipoma. J Robot Surg. 2017;11(2):267-269. doi: 10.1007/s11701-016-0668-7. [ Links ]
17. Robb WB, Bruyere E, Amielh D, Vinatier E, Mabrut JY, Perniceni T, et al. Esophageal gastrointestinal stromal tumor: is tumoral enucleation a viable therapeutic option? Ann Surg. 2015;261(1):117-24. doi: 10.1097/SLA.0000000000000505. [ Links ]
18. Kocher GJ. Robotic-assisted thoracoscopic surgery: state of the art and future perspectives. J Thorac Dis. 2017;9(7):1855-7. doi: 10.21037/jtd.2017.06.139. [ Links ]
19. Compean S, Gaur P, Kim M. Robot assisted thoracoscopic resection of giant esophageal leiomyoma. Int J Surg Case Rep. 2014;5(12):1132-4. doi: 10.1016/j.ijscr.2014.11.003. [ Links ]
20. Jeon HW, Choi MG, Lim CH, Park JK, Sung SW. Intraoperative esophagoscopy provides accuracy and safety in video-assisted thoracoscopic enucleation of benign esophageal submucosal tumors. Dis Esophagus. 2015;28(5):437-41. doi: 10.1111/dote.12220. [ Links ]
21. Ben-David K, Alvarez J, Rossidis G, Desart K, Caranasos T, Hochwald S. Thoracoscopic and Laparoscopic Enucleation of Esophageal Leiomyomas. J Gastrointest Surg. 2015;19(7):1350-4. doi: 10.1007/s11605-015-2817-0. [ Links ]
Received: October 23, 2017; Accepted: March 04, 2018











 texto en
texto en 


