Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.4 Bogotá oct./dic. 2018
https://doi.org/10.22516/25007440.170
Case report
Case report of perineal rectosigmoidectomy (Altemeier’s procedure) for incarcerated rectal prolapse
1Hospital Simón Bolívar. Bogotá D. C., Colombia
Reports of incarcerated rectal prolapse are rare and pose a challenge to the surgeon. For a incarcerated prolapse that is not strangulated, patients should be treated with analgesics and placed in the Trendelenburg position. Conservative measures should be applied to the prolapse with simultaneous manual pressure. If successful reduction is not achieved, then the patient usually requires rectosigmoidectomy with a perineal approach (Altemeier’s procedure).
Case:
The patient was a 57-year-old man with no previous history of symptoms or comorbidities that would predispose him to this pathology. He came to the emergency department with an incarcerated rectal prolapse after attempting to have a bowel movement five hours earlier. Conservative measures of placing the patient in the Trendelenburg placement and topical application of granulated sugar were used. These measures were unsuccessful, so the patient required a rectosigmoidectomy with a perineal approach and protective ileostomy. The patient’s postoperative recovery was without complications and had excellent results after the ileostomy was closed. There has been no recurrence.
Discussion:
Incarceration leads to strangulation over time, so surgery is usually indicated if conservative therapy fails. Although traditionally recommended for elderly patients and patients with comorbidities, perineal procedures are an option for all patients, and this is the best option for incarcerated rectal prolapse.
Keywords: Anorectal disease; rectal prolapsed; incarcerated; perineal rectosigmoidectomy; Altemeier’s procedure
Los reportes de prolapso rectal encarcelado son infrecuentes y suponen un reto para el cirujano. Para un prolapso encarcelado no estrangulado, los pacientes deben tratarse con analgésicos y colocarse en la posición de Trendelenburg; y deberían aplicarse medidas conservadoras al prolapso con presión manual simultánea. Si la reducción exitosa no se logra, entonces el paciente generalmente requiere una rectosigmoidectomía con abordaje perineal (procedimiento de Altemeier).
Caso clínico:
hombre de 57 años, sin una historia previa de síntomas o comorbilidades con predisposición para esta patología. Se presenta en el departamento de urgencias con un prolapso rectal encarcelado posterior a realización de esfuerzo 5 horas antes del ingreso. Se inician medidas conservadoras con colocación en Trendelenburg y aplicación de azúcar granulada tópica. Las medidas fueron infructuosas. El paciente requirió una rectosigmoidectomía con abordaje perineal e ileostomía de protección. El curso postoperatorio no tuvo complicaciones, hubo un excelente resultado después del cierre de la ileostomía y no hubo recurrencia.
Discusión:
el encarcelamiento conlleva a estrangulamiento a lo largo del tiempo, la cirugía generalmente está indicada si la terapia conservadora fracasa. Aunque tradicionalmente recomendada para los pacientes adultos mayores y pacientes con comorbilidades, los procedimientos perineales son una opción para todos los pacientes y la mejor opción para el prolapso rectal encarcelado.
Palabras clave: Enfermedad anorrectal; prolapso rectal; encarcelado; rectosigmoidectomía perineal; procedimiento de Altemeier
Introduction
Rectal prolapse, also called rectal procidentia, is the prolapse of the total thickness of the rectum which passes externally through the anal sphincters. Its first description dates back to Ebers Papyrus of Ancient Egypt (dating to 1500 BC), and the first report in the medical literature of mortality associated with prolapse is that of the exiled North African theologian, Arius of Alexandria (256 -336 AD) 1.
This condition is estimated to occurs in less than 0.5% of the population. It has a female: male ratio of 9:1, and its incidence increases with age (more than 50% of cases are women over 50). The categories in order of decreasing severity include rectal prolapse of the total thickness of the rectum, prolapse of the mucosa, and internal prolapse. The main clinical sign is protrusion itself with additional symptoms that include constipation, a sensation of incomplete evacuation, rectal bleeding, rectal pain, incontinence, urgency and tenesmus. 2
Patients with rectal prolapse usually have a medical history associated with various diseases that worsen their general condition and exclude them from general anesthetic treatment and surgical procedures that include intestinal resection and anastomosis. The choice of surgical procedure depends mainly on patient’s age, clinical condition, surgical risk, coexisting functional symptoms, and the familiarity of the surgeon with a particular surgical approach. Patients with acute complete rectal prolapse usually arrive in the emergency department. Every effort should be made to manually reduce a persistently prolapsed rectum, but in ways that avoid complications such as strangulation, ulceration, bleeding and perforation. 1 The development of progressive edema can make manual reduction attempts difficult or unsuccessful. Edema is a progressive process that leads to strangulation. Vessels in the prolapsed mesentery may also become compromised and ischemia may occur over time, so surgery is indicated if conservative therapy fails. 1,2,3
Clinical case
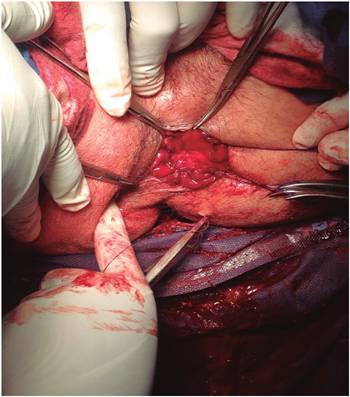
The patient was a 57-year-old man with arterial hypertension and type 2 diabetes mellitus who had not had any previous surgery. He was admitted to the emergency department with an incarcerated rectal prolapse after five hours of efforts to defecate before admission (Figure 1). There were no previous episodes of rectal prolapse recorded in the patient’s medical history. No other background was mentioned. On admission, the patient presented vital signs within normal limits and was hemodynamically stable. His abdomen was depressible but not painful and had no signs of peritoneal irritation. Paraclinical tests showed minor leukocytosis with displacement to the left but no other findings. The intestine was prolapsed and hypoperfused but not necrotic. Conservative measures to allow the intestine to rest and to decrease edema were begun.
Unfortunately, the patient’s placement in the Trendelenburg position and application of topical sucrose with simultaneous manual pressure were unsuccessful, so the patient was taken to the operating room five hours after the start of conservative measures.
With the patient in lithotomy position and under general anesthesia, a circumferential incision was made with electrocautery on the entire rectal wall two cm from the dentate line (Figure 2). Following ligature of the mesorectum and the mesosigmoid, the prolapsed rectosigmoid was resected and an anastomosis, interrupted by hand in two planes, was created (Figure 3).
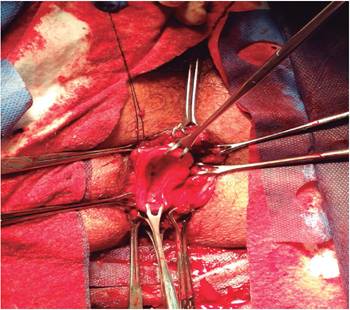
Figure 2 Excision of the full thickness of the external prolapse cylinder with mesenteric vessels attached.
A double-mouth ileostomy was constructed to protect the anastomosis. The patient’s postoperative development was uncomplicated, so he was discharged ten days after surgery. Pathology of the surgical piece revealed intestinal mucosa with areas of necrosis but without ulceration. Anal manometry showed the hypotonic anal sphincter at rest. During voluntary contraction, it retained the ability to sustain voluntary contraction, normal rectal sensitivity and manometric response to normal tone cough. The patient had five biofeedback sessions after which anal manometry showed that the anal sphincter had normal tone at rest and during voluntary contraction and had the ability for sustained contraction. Patient was readmitted 11 months following surgery. A barium enema showed that he was within the normal limits for the closure of the protective ileostomy. Since then, the patient’s condition has been, ileostomy was closed, and there has been no recurrence.
Discussion
Cases of completely incarcerated rectal prolapse are infrequent, and their causes are not clearly understood. Laxity of the pelvic floor with associated pelvic neuropathy, persistent exertion, chronic constipation, rectal tumors and anal sphincter dysfunction have been implicated. Two theories have been proposed to explain rectal prolapse as a sliding hernia or intussusception. Contrary to popular belief, the number of childbirths and the trauma of childbirth do not seem to be predisposing factors for women, and women without children account for 40% to 60% of patients in most studies. 4 In the case of our patient, a man with no previous history of rectal prolapse, his diabetes mellitus may have been related to a neuropathy associated with the development of this condition.
A true complete rectal prolapse presents as a large rectal mass or protuberance whose size may or may not spontaneously decrease. It is necessary to recognize conditions that are often associated with rectal prolapses including hemorrhoid prolapse, prolapsed tumors or polyps and abnormal perineal descent (which includes uterine prolapse). In the case of our patient, rectal prolapse it presented without other associated conditions. Incarcerated rectal prolapses present with nonspecific symptoms, but the most common are feelings of fullness, sensations of a mass inside the rectum, constipation, fecal incontinence, obstructed defecation, mucous drainage and bleeding. Rectal incarceration and also strangulation often presents as a large, painful and immobile rectal mass. 5
Once in the emergency room, everything possible must be done to manually reduce a prolapsed non-reducible persistent incarcerated rectum in order to avoid complications such as strangulation, ulceration, bleeding and perforation secondary to ischemia. 6 Several methods have been described in the literature to reduce an imprisoned rectal prolapse:
Adrenaline injections
Submucosal infiltration of hyaluronidase (hyaluronoglucosidase), which is an endoglucosidase. It acts by depolymerizing hyaluronic acid with resulting decomposition of the extracellular matrix. This mechanism allows the edema fluid to drain through the microscopic spaces created in the extracellular compartment thereby decreasing edema. 7
Topical application of granulated sugar. Reduction is achieved quickly and easily using sugar as a means to reduce tissue edema. This is due to the hyperosmolarity of the molecule with which extraction of water from the intestine is achieved. 8 This was the technique used for our patient.
Hypertonic solutions of sugar consisting of 50% dextrose or 70% mannitol applied directly to the rectal mucosa. These have also been used to reduce edema and facilitate manual reduction of prolapse.
An elastic compression band that uses increased pressure to force the edema fluid out of the prolapse. The elasticity of the sheath allows continuous compression of the prolapse. This type of elastic band is often stored in operating rooms for use in orthopedic procedures and is easily accessible. 9
All of these techniques should be performed after administration of analgesia and with the patient in the Trendelenburg position.
Immediate surgical intervention is reserved for those rare cases in which the patient has late complications such as ischemia or ulceration. Surgery should also be performed when conservative measures and manual reduction have not been successful (as was the case of our patient). 10 Jeopardizing the viability of the intestine should be avoided since gangrene significantly increases morbidity and mortality. There are a large number of perineal and abdominal approaches that have been useful in treating rectal prolapse in elderly and high-risk patients, but perineal rectosigmoidectomy (Altemeier’s procedure) with or without a protective stoma is favored because it is simple, recurrence is infrequent, and morbidity and mortality rates are low. 11
Some authors believe that perineal rectosigmoidectomy is indicated for patients who have suffered an early recurrence in the first years after other perineal repair, for elderly patients, for patients with multiple medical problems and incontinence who do not tolerate general anesthesia, for male patients because of higher rates of impotence resulting from abdominal approaches, and for patients with an imprisoned or strangulated rectal prolapse. Without a doubt, the choice of surgical approach must be defined according to the surgical experience of the surgeon.11,12 In addition, in this case a transabdominal construction of a sigmoid colostomy or double-mouth ileostomy was performed in order to protect the anastomosis from the fecal stream. 13
Surgical options are more challenging in cases of incarceration due to the increased risk of surgical anastomosis resulting from increased edema and hypoperfusion. The rate of anastomotic leakage ranges from 2% to 6% for elective perineal rectosigmoidectomy in contrast to 25% for incarcerated or strangulated rectal prolapse. Perineal rectosigmoidectomy together with protective loop colostomy or ileostomy through an incision is a less invasive surgical option which has less risk of contamination than does open surgery. The length of hospital stay is also shorter for perineal approaches than for abdominal procedures. 14 Although reports by Fei and colleagues suggest surgery in two sessions, a first time with a circumferential incision of the prolapsed segment and a second surgery two weeks later for the resection and anastomosis. They completed this procedure successfully in three patients. The two-stage approach has been tried in order to reduce the leak rate, but the most common ways to reduce complications are ileostomies and protective colostomies. 15
Patients’ postoperative development following perineal rectosigmoidectomy is usually very favorable. Patients have minimal pain, oral intake can begin after 24 to 48 hours and bowel functioning returns within a few days of surgery. Most patients are ready for discharge within 10 days of surgery. Recurrence probably reflects inadequate resection, so care should be taken to mobilize the entire redundant rectum and perform the anastomosis inside the pelvis. 11 In conclusion, we have described a rare case of incarcerated rectal prolapse in a male adult treated with a rectosigmoidectomy with a perineal approach. This case highlights the importance of Altemeier’s procedure in the face of a incarcerated or strangulated rectal prolapse in an emergency situation.
Conclusion
The type of surgery for patients with rectal prolapse should be selected after taking the patient’s general condition and the surgeon’s experience into account. Because it has lower recurrence, morbidity and mortality rates than does abdominal surgery, Altemeier’s procedure is the preferred surgical option for incarcerated rectal prolapse especially for patients who require resection, for debilitated elderly patients with comorbidities, and for patients under 50 years of age to reduce the risk of postoperative sexual impotence.
REFERENCES
1. Barfield LR. Perineal Approaches to Rectal Prolapse. Clin Colon Rectal Surg. 2017;30(1):12-15. [ Links ]
2. Cannon JA. Evaluation, Diagnosis, and Medical Management of Rectal Prolapse. Clin Colon Rectal Surg. 2017;30(1):16-21. [ Links ]
3. Yuzbasioglu MF, Bulbuloglu E, Ozkaya M, Oksuz H.A different approach to incarcerated and complicated rectal prolapse. Med Sci Monit. 2008;14(7):CS60-3. [ Links ]
4. Coburn WM 3rd, Russell MA, Hofstetter WL. Sucrose as an aid to manual reduction of incarcerated rectal prolapse. Ann Emerg Med. 1997;30(3):347-9. doi: 10.1016/S0196-0644(97)70174-4. [ Links ]
5. Bordeianou L, Hicks CW, Kaiser AM, Alavi K, Sudan R, Wise PE. Rectal prolapse: an overview of clinical features, diagnosis, and patient-specific management strategies. J Gastrointest Surg. 2014;18(5):1059-69. doi: 10.1007/s11605-013-2427-7. [ Links ]
6. Sakaguchi D, Ishida H, Yamada H, Tsuzuki S, Hayashi Y, Yokoyama M, et al. Incarcerated recurrent rectal prolapse with ileal strangulation: report of a case. Surg Today. 2005;35(5):415-7. doi: 10.1007/s00595-004-2930-2. [ Links ]
7. Chaudhuri A. Hyaluronidase in the reduction of incarcerated rectal prolapse: a novel use. Int J Colorectal Dis. 1999;14(4-5):264. doi: 10.1007/s003840050223. [ Links ]
8. Shapiro R, Chin EH, Steinhagen RM. Reduction of an incarcerated, prolapsed ileostomy with the assistance of sugar as a desiccant. Tech Coloproctol. 2010;14(3):269-71. doi: 10.1007/s10151-009-0507-1. [ Links ]
9. Sarpel U, Jacob BP, Steinhagen RM. Reduction of a large incarcerated rectal prolapse by use of an elastic compressionwrap. Dis Colon Rectum. 2005;48(6):1320-2. doi: 10.1007/s10350-004-0913-4. [ Links ]
10. Ben Ameur H, Rejab H, Beyrouti MI. Altemeier operation for recurred and strangulated rectal prolapse. Indian J Surg. 2013;75(Suppl 1):224-6. doi: 10.1007/s12262-012-0656-8. [ Links ]
11. Takesue Y, Yokoyama T, Murakami Y, Akagi S, Ohge H, Yokoyama Y, et al. The effectiveness of perineal rectosigmoidectomy for the treatment of rectalprolapse in elderly and high-risk patients. Surg Today. 1999;29(3):290-3. doi: 10.1007/BF02483026. [ Links ]
12. Yildirim S, Köksal HM, Baykan A. Incarcerated and strangulated rectal prolapse. Int J Colorectal Dis. 2001;16(1):60-1. doi: 10.1007/s003840000264. [ Links ]
13. Voulimeneas I, Antonopoulos C, Alifierakis E, Ioannides P. Perineal rectosigmoidectomy for gangrenous rectal prolapse. World J Gastroenterol. 2010;16(21):2689-91. doi: 10.3748/wjg.v16.i21.2689. [ Links ]
14. Sipahi M, Arslan E, Börekçi H, Aytekin FÖ, Külah B, Banlı O. Perineal rectosigmoidectomy for incarcerated rectal prolapse (Altemeier’s procedure). Ulus Cerrahi Derg. 2015;32(3):217-20. [ Links ]
15. Fei R, Chen W, Xiang T, Sheng Q, Wang J, Liu F. A modified two-stage perineal rectosigmoidectomy for incarcerated rectal prolapse. Tech Coloproctol. 2014;18(5):513-4. doi: 10.1007/s10151-013-0996-9. [ Links ]
Received: October 23, 2017; Accepted: December 04, 2017











 texto en
texto en