Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.33 no.4 Bogotá oct./dic. 2018
https://doi.org/10.22516/25007440.186
Case report
Symptomatic rectal diverticulum
1Médico internista y gastroenterólogo. Instituto Gastroclínico. Medellín, Colombia
Rectal diverticula are unusual findings during colonoscopy and radiological studies of the colon. Prevalence is estimated to be approximately 1%, and they occur more frequently in men between the 6th and 9th decade of life. Most patients are asymptomatic, although some may present symptoms or related complications. We report the case of a patient with a large rectal diverticulum with abdominal pain and constipation.
Keywords: Rectum; diverticulum; constipation; abdominal pain.
Los divertículos rectales son hallazgos inusuales durante la colonoscopia o estudios radiológicos del colon. Se estima una prevalencia aproximada del 1 % y se presenta con mayor frecuencia en hombres entre la sexta y novena década de la vida. En la mayoría de pacientes son asintomáticos, aunque algunos pueden cursar con síntomas o complicaciones relacionadas. Se reporta el caso de una paciente con divertículo rectal grande con dolor abdominal y estreñimiento.
Palabras clave: Recto; divertículo; estreñimiento; dolor abdominal
Introduction
Rectal diverticula are not found frequently, are asymptomatic in most patients, and diagnosis is usually incidental. They can be related to colonic diverticulosis or to complications of surgery in the rectum. We present the case of a patient with a large rectal diverticulum with abdominal-pelvic pain and incomplete rectal evacuation.
Case presentation
The patient was a 53-year-old woman with no pathological or surgical history who had had recurrent colicky abdominal pain for the previous two years. Pain was located predominantly in the left iliac fossa and radiated to the hypogastrium. Pain worsened after consuming food and was associated with constipation and stools between 1 and 2 on the Bristol scale. She highlighted a sensation of incomplete evacuation, tenesmus, a need for pushing and marked improvement of abdominal and pelvic pain after defecation but said she had suffered no rectal bleeding or weight loss. A physical examination including digital rectal examination was normal.
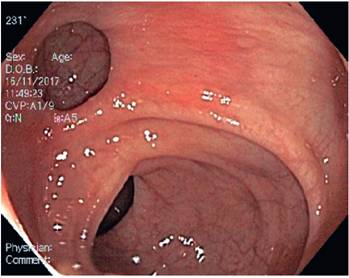
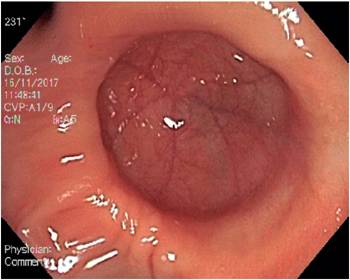
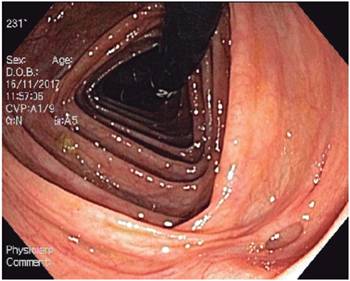
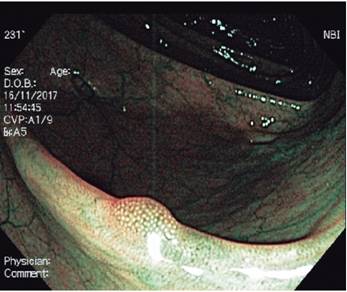
Based on her age and symptoms, a colonoscopy was performed to rule out structural organic pathology. We observed a round diverticulum that was about 3 cm in diameter and was located in the lateral wall of the middle rectum at 6 cm from the dentate line. There were no inflammatory changes nor lesions in the mucosa around it, and there were no fecoliths. The diverticulum changed shape in response to insufflation/air suction (Figures 1 and 2). During exploration of other parts of the colon, multiple diverticula without complications whose diameters were between 5 and 10 mm were observed (Figure 3). In addition, a tiny adenomatous polyp in the transverse colon was resected with a clamp (Figure 4). Considering that the symptoms of the patient (especially those suggestive of an evacuation disorder) could be explained by the diverticula of the colon, management with Psyllium fiber supplement and antispasmodics was begun and led to significant improvement of the clinical picture and the patient’s quality of life.
Discussion
Unlike diverticula in the colon, diverticula in the rectum contain all the layers of the wall and are considered to be true diverticula. 1 The true prevalence of rectal diverticula is difficult to establish since the majority of cases they are asymptomatic and diagnosis is usually incidental. It is estimated that approximately 80 cases have been published in the literature. In Colombia, only one case had been reported: an incidental finding in colonoscopy of a male patient. 2 A series of 4,854 patients based on studies of the colon by enema found a prevalence of 0.08%. 3 Another similar, but more recent study published in 2013, found a prevalence of 1.5% in 2,877 patients. 4 A series of cases of patients who had undergone colonoscopies found an overall 10-year prevalence of 0.15% while in patients with colonic diverticulosis it was 0.75%. 5 In most reports, the greatest number of cases occurs in men between 55 and 85 years of age. 6
Three theories explain the low prevalence of this finding. The anatomical disposition of the muscle fibers of the Tenia libera and Tenia omentalis in the anterior and posterior walls of the rectum lead to reinforcement of the rectal structure causing greater resistance to intraluminal variations. This also explains why the majority of cases have been documented in the lateral wall. 7 Similarly, pressure is lower and there are less peristaltic movements in the rectum than in the sigmoid colon explaining why the diverticula rate is much lower than that of this colonic segment. Finally, given the report of a case of rectal diverticulum in a pediatric patient, congenital origins have not been ruled out. 8
Although the majority of diverticula occur in the other colon tracts where the risk is highest, a group of cases with iatrogenic origins have been reported following surgery such as those performed for prolapsed hemorrhoids, Longo’s procedure for hemorrhoidectomy, and rectal transanal resections due to mucosal prolapse. 9,10,11 Other associated risk factors include obesity, constipation, episodes of recurrent fecal impaction, absence of pelvic support such as coccyx, rectal infections, trauma and degenerative muscle diseases. 5. In most cases, the diameters of rectal diverticula are 2 cm and larger. 12 Although they generally do not cause symptoms, some cases have included all complications including bleeding, diverticulitis and perforation. They have also been described in association with evacuation disorders, formation of with fistulas, ulcerated surfaces, rectal prolapse, and a sensation of perineal mass. Adenocarcinoma has even been described inside a rectal diverticulum. 13,14 For this reason, periodic follow-ups are recommended given the apparently increased risk of cancer.
Perforation entails a lower degree of complications than it does in a colonic diverticulum, given the anatomical location of the rectum below the peritoneal reflection. 5 Documentation of diverticula can be done by colonoscopy or radiological studies by barium enema, computerized axial tomography, (CAT) or magnetic resonance imaging (MRI). Caution should be exercised In with endoscopic studies given the risk of perforation. 15 In one of the cases reported, conventional anorectal manometry was performed without finding abnormalities of rectal pressure, rectal sensitivity or anal sphincter pressure. 16
Management depends on the intensity of symptoms and associated complications. For patients with mild to moderate symptoms, a diet rich in fiber is suggested together with antispasmodics. For cases with symptoms that alter the quality of life of the patient and are refractory to medical management or have related complications such as bleeding, diverticulitis or perforation, surgery is suggested. Surgical procedures range from diverticulectomy to more complex procedures such as rectosigmoidectomy or abdominal-perineal resection. 17,18
The case of this patient demonstrates that there may be symptoms associated with large rectal diverticula, especially symptoms related to inadequate anorectal evacuation. Anorectal manometry was not performed in this case since the patient improved with a high-fiber diet. Nevertheless, it is an option in refractory patients given that this pathology can be related to defecation disorders, and biofeedback therapy can have a role to play in treatment.
Conclusions
Rectal diverticula are an uncommon finding during colonoscopy and radiological studies of the colon. They should be suspected in patients with evacuation disorders, as in the case of our patient, and in patients with histories of rectal surgery. They may also be found as the result of complications of a diverticulum such as bleeding, diverticulitis or perforation. Management depends on the severity of the symptoms and any complications that present.
Referencias
1. Halpert RD, Crnkovich FM, Schreiber MH. Rectal diverticulosis: a case report and review of the literature. Gastrointest Radiol. 1989;14:274-6. doi: 10.1007/BF01889215. [ Links ]
2. Ángel A, Cardona D. Divertículo rectal. Reporte de un caso. Biosalud. 2017;16(2):119-22. [ Links ]
3. Walstad PM, Sahibzada AR. Diverticula of the rectum. Am J Surg. 1968;116:937-9. doi: 10.1016/0002-9610(68)90471-6. [ Links ]
4. Lohsiriwat V, Suthikeeree W. Pattern and distribution of colonic diverticulosis: Analysis of 2877 barium enemas in Thailand. World J Gastroenterol. 2013;19(46):8709. doi: 10.3748/wjg.v19.i46.8709. [ Links ]
5. Fagundes RB, Motta GL, Fontana K, Fonseca CB, Binato M. Rectal diverticulum. ABCD Arq Bras Cir Dig. 2011;24(4):339-41. doi: 10.1590/S0102-67202011000400018. [ Links ]
6. Damron JR, Lieber A, Truman S. Rectal diverticula. Radiology. 1975;115:599-601. doi: 10.1148/15.3.599. [ Links ]
7. Abrisqueta J , Frutos MD, Lujan J, Abellan I, ParrillaP. Divertículo rectal solitario. Presentacion de un caso. Cir Esp. 2013;91(2):122-31. doi: 10.1016/j.ciresp.2011.09.006. [ Links ]
8. Kumar R, Shun A, Arbuckle S, Gaskin K. Diverticular rectal duplication with heterotopic gastric mucosa in a child: a rare cause of rectal bleeding. J Paediatr Child Health. 2000;36:191-2. doi: 10.1046/j.1440-1754.2000.00482.x. [ Links ]
9. Alabiso ME, Grassi R, Fioroni C, Marano I. Iatrogenic rectal diverticulum in patients treated with transanal stapled techniques. Radiol Med. 2008;113:887-94. doi: 10.1007/s11547-008-300-7. [ Links ]
10. Pellino G. Rectal diverticulum after stapled transanal procedures: surgery encouraged. Am Surg. 2013;79(12):1320. [ Links ]
11. Boffi F, Podzemny V. Obstructed defecation, rectocele, recurrent hemorrhoids, and rectal diverticulum following the PPH. Tech Coloproctol. 2011;15:255-6. doi: 10.1007/s10151-011-0691-7. [ Links ]
12. Piercy KT, Timaran C, Akin H. Rectal diverticula. Dis Colon Rectum. 2002;45:1116-7. doi: 10.1007/s10350-004-6371-1. [ Links ]
13. Jung SH, Kim JH. A case of solitary rectal diverticulum presenting with a retrorectal mass. Gut Liver. 2010;4:394-7. doi: 10.5009/gnl.2010.4.3.394. [ Links ]
14. Kwon JH, Han KH, Chang WS, Nam KH, Han MS, Ahn JH, et al. A Case of a Mucinous Adenocarcinoma Arising from a Rectal Diverticulum. J Korean Soc Coloproctol 2012;28(4):222-4. doi: 10.3393/jksc.2012.28.4.222. [ Links ]
15. Hong KD, Lee S Il, Moon HY. Rectal diverticular perforation complicating diagnostic colonoscopy: a case report and review of the literature. J Laparoendosc Adv Surg Tech A. 2011;21(8):745-8. doi: 10.1089/lap.2011.0210. [ Links ]
16. Martinez CAR, Priolli DG, Palma RT, Waisberg J. Divertículo do reto: relato de caso. Rev Bras Coloproct. 2003;23(4):296-30. [ Links ]
17. Binda GA, Cuomo R, Laghi A, Nascimbeni R, Serventi A, Bellini D, et al. Practice parameters for the treatment of colonic diverticular disease: Italian Society of Colon and Rectal Surgery (SICCR) guidelines. Tech Coloproctol. 2015;19(10):615-26. doi: 10.1007/s10151-015-1370-x. [ Links ]
18. Frangi A, Gomez MA, Moya P, Arroyo A, Lopez A. Rectal diverticulum resection by stapler device Tech Coloproctol. 2014;18:403-4. doi: 10.1007/s10151-012-0957-8. [ Links ]
Received: December 12, 2017; Accepted: February 06, 2018











 texto en
texto en