Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.1 Bogotá jan./mar. 2019
https://doi.org/10.22516/25007440.243
Original articles
Outcomes of Three Years of Experience Managing Acute Pancreatitis at a Fourth Level Hospital in Huila, Colombia
1Hospital Universitario Hernando Moncaleano Perdomo de Neiva. Neiva, Colombia
2Hospital San José. Bogotá D. C., Colombia
3Hospital San Juan de Dios. Ituango, Antioquia, Colombia
4Hospital El Tunal. Bogotá D. C., Colombia
Objective:
Our objective was to describe the clinical and surgical behavior of patients with acute pancreatitis managed at a fourth level hospital center.
Method:
This is a descriptive, retrospective and analytical study of patients diagnosed with acute pancreatitis who entered the University Hospital of Neiva in the period from January 1, 2015 to July 31, 2017.
Results:
We identified 138 patients who had been admitted with a diagnosis of acute pancreatitis. Of these, the diagnosis was confirmed for 130 patients, but 21 patients were excluded because they did not meet the inclusion criteria. According to the 2012 Atlanta classification, 73 (67%) patients had mild pancreatitis, 17 (16%) had moderately severe pancreatitis, and 19 (17%) had severe pancreatitis. The main cause of pancreatitis was biliary. The chi-square test showed statistical significance for age as a risk factor for severe pancreatitis (p = 0.04). Pancreatic necrosis was documented in 8 patients, five of whom were managed surgically. This included three laparotomies and two laparoscopic operations. The mortality rate for patients with surgically managed pancreatic necrosis was 37.5%. Of the 109 patients included in the study, the resolved their pancreatitis of 100 patients (91.74%) was resolved and they left the institution alive. Nine patients (8.25%), all of whom had severe acute pancreatitis, died.
Conclusion:
This descriptive study established the demographic characteristics and clinical course of patients with acute pancreatitis including complications and management of complications. This study is not intended to standardize causality or management of acute pancreatitis, but rather only describes the experience of a fourth level hospital in order to contribute to the development of cohort studies and clinical trials that will allow establishment of management guidelines to improve the outcomes of patients with acute pancreatitis.
Keywords: Acute pancreatitis; pancreatic necrosis; severe acute pancreatitis
Objetivo:
describir el comportamiento clínico y quirúrgico de los pacientes con pancreatitis aguda manejados en un centro hospitalario de cuarto nivel.
Método:
se realizó un estudio descriptivo retrospectivo analítico de los pacientes con diagnóstico de pancreatitis aguda que ingresaron al Hospital Universitario de Neiva en el período comprendido entre el 1 de enero del 2015 al 31 de julio del 2017.
Resultados:
se identificaron 138 pacientes que ingresaron con impresión diagnóstica de pancreatitis aguda, de los cuales se confirmó el diagnóstico en 130 pacientes y se excluyeron 21 pacientes por no cumplir con los criterios de inclusión. Según la clasificación de Atlanta 2012, 73 (67 %) pacientes cursaban con una pancreatitis leve, 17 (16 %) con pancreatitis moderadamente severa y 19 (17 %) con pancreatitis severa. La principal causa de pancreatitis encontrada fue la biliar. La prueba de chi cuadrado (χ2) mostró una significancia estadística para la edad como factor de riesgo para pancreatitis severa (p = 0,04). De la totalidad de pacientes, en 8 pacientes se documentó necrosis pancreática, de los cuales 5 fueron manejados quirúrgicamente, con un abordaje por laparotomía en 3 pacientes y 2 por laparoscopia, con una mortalidad del 37,5 % en los pacientes con necrosis pancreática manejados quirúrgicamente. De los 109 pacientes incluidos en el estudio, 100 pacientes (91,74 %) resolvieron su cuadro de pancreatitis y egresaron vivos de la institución, para una mortalidad reportada en 9 pacientes (8,25 %), quienes cursaron con pancreatitis aguda severa.
Conclusión:
el estudio presentado es de tipo descriptivo estableciendo las características demográficas y el curso de la enfermedad de los pacientes con pancreatitis aguda incluidos las complicaciones y el manejo de estas. Con este estudio no se pretende estandarizar causalidad ni manejo de la patología descrita, solo se describe la experiencia realizada en un hospital de cuarto nivel tratando de contribuir con el desarrollo de estudios de cohortes y ensayos clínicos que permitan establecer guías de manejo con el fin de mejorar los desenlaces de los pacientes con pancreatitis aguda.
Palabras clave: Pancreatitis aguda; necrosis pancreática; pancreatitis aguda severa
Introduction
Acute pancreatitis is an inflammatory disease of the pancreas that causes a large number of admissions to emergency departments around the world. It is characterized by a wide spectrum of clinical manifestations, ranging from mild self-limiting symptoms to processes with shock and multiple organ failure. 1 Its annual incidence is between 13 to 45 individuals per 100,000 inhabitants, 2 and the main causes of acute pancreatitis are associated with biliary pathology and alcohol consumption followed by comorbidities such as dyslipidemias, some drugs and infectious processes.
Despite improvements in access to care, imaging and intervention techniques, acute pancreatitis continues to be associated with significant morbidity and mortality. These depend on the patient’s comorbidities and the severity of the clinical picture. Morbidity and mortality rate ranges are between 7% and 40% in the worst cases. 3 For this reason, multiple efforts have been made to characterize and epidemiologically define guidelines and recommendations for management of these patients. At least 14 sets of guidelines were issued between 2004 and 2014. 4 In spite of this, throughout the world it is common to find both unclear criteria for treatment at various degrees of severity of this pathology and failure to adhere in clinical practice of any recommendations.
This underlines the importance of continued study of this disease and the results obtained by the various treatment groups. Additional study should allow consolidation of clear recommendations applicable to the different levels of hospital care which will thereby improve results and the prognosis of the affected population.
This is a study of patients who were diagnosed with, and treated for mild, moderately severe and severe pancreatitis at a third level hospital in Neiva, Colombia. It presents patients’ sociodemographic and clinical characteristics, the pathology’s clinical behavior, and results of treatment.
Materials and method
This is a descriptive, retrospective and analytical study of patients diagnosed with acute pancreatitis who entered the Hospital Universitario de Neiva (HUN) from January 1, 2015 to July 31, 2017. Data was collected from HUN’s medical records. The data were organized into tables and included description of the population studied, classification, complications, morbidity and mortality, as well as relations with patients’ clinical variables.
Results
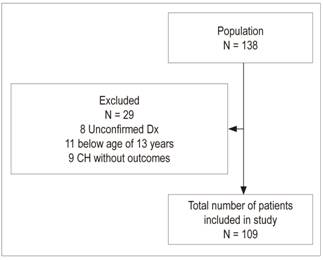
We found 138 patients admitted to the university hospital of Neiva who were initially diagnosed with acute pancreatitis. The diagnosis was confirmed in 130 patients of whom 21 patients were excluded because they did not meet the inclusion criteria (Figure 1).
The total number of patients studied was 109. Forty-three were male, and 68 were female. Patients’ ages ranged from 13 to 94 years: eight patients were under 25 years of age, 58 patients were between 25 and 59 years old, and 43 were over 60 years of age. The average body mass index (BMI) of these patients was 26.7 kg/m2, 43 patients were overweight (39.8%), and 24 patients were obese (22%). The rest of patients were within the range of normal weight (Table 1).
Table 1 General characteristics of patients
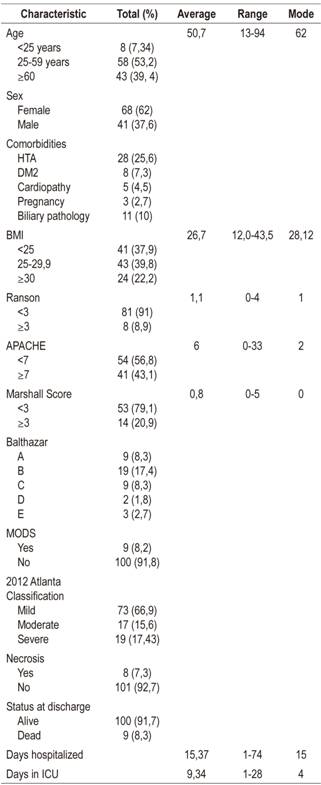
APACHE: Acute Physiology and Chronic Health Evaluation; DM2: diabetes mellitus type 2; HT: arterial hypertension; MODS: multiple organ dysfunction syndrome; ICU: intensive care unit.
High blood pressure was the comorbidity found most frequently (28 patients, 25.6%). It was followed by biliary pathologies (11 patients, 10.09%), diabetes mellitus (8 patients, 7.33%), heart disease (5 patients, 4.58%), and pregnancy (3 patients, 2.75%). Forty-two patients had no comorbidities. Ninety-three patients (85.3%), eleven patients (10.09%) tested negative, and there were no data for five patients (4.58%). The average level of amylase was 1,900 (Table 1).
Three scales for measuring severity were used. The Ranson scale was calculated upon admission and had an average value of 1.14 although no data were found for 20 patients (18.3%). It was calculated to be less than 3.0 for 81 patients (74.3%) and greater than 3.0 for eight patients (7.3%). It was difficult to calculate the Ranson at 48 hours given the absence of data in the clinical histories. At 48 hours, we found it to be less than three for 27 patients (24.7%) and greater than three for 10 patients (9.1%). On average, its value was 1.54. There were not enough data to calculate it for 72 patients (66%). It was possible to calculate Marshall Score values for fifty- three patients (48.6%) 14 (12.8%) of whom had values of two or more. There were no data available to make this calculation for 52 patients (47.7%). At admission, 54 patients (49.5%) had APACHE II measurements of less than eight while 41 patients had measurements of more than eight. The average APACHE II measurement at admission was 7.49. There were no data for 14 patients. At 48 hours, thirteen patients (11.9%) had APACHE II measurements of less than eight, thirteen patients (11.9%) had APACHE II measurements of more than eight, and the average measurement was 9.76. There were no data to calculate it for 83 patients (76.1%) (Table 1).
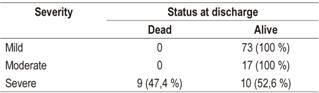
According to the 2012 revised Atlanta classification, 73 patients (67%) had mild pancreatitis, 17 patients (16%) had moderate pancreatitis, and 19 patients (17%) had severe pancreatitis (Table 1).
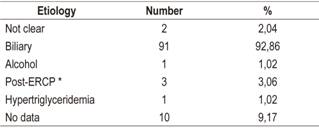
The principal cause of pancreatitis was biliary (91 patients, 83.2%), four patients presented pancreatitis after endoscopic retrograde cholangiopancreatography (ERCP), one patient developed it as the result of alcohol consumption, another patient developed it as the result of hypertriglyceridemia, and there were no data found for the other ten patients (Table 2).
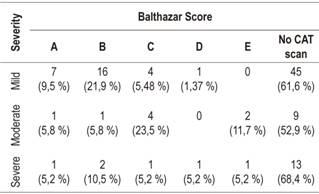
Computerized axial tomography (CAT) scans were made for 42 patients included in this study. Of these, nine patients (8.26%) were reported to be Balthazar A, 19 patients (17.4%) were reported to be Balthazar B, nine patients (8.26%) were reported to be Balthazar C, two patients (1.83%) were reported to be Balthazar D, and three patients (2.75%) were reported to be Balthazar E. Sixty-seven patients (61%) had no relevant records. Of the 19 patients with severe pancreatitis, thirteen did not have any imaging study done (Table 3).
The average hospital stay was 15.23 days. Thirty-five patients were admitted to the ICU and had average stays of 9.34 days.
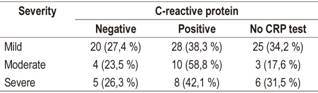
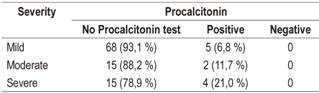
Relevant laboratory test results included positive tests for C-reactive protein (CRP) for 46 patients (42.2%) and negative CRP rests for 29 patients (26.6%). Only eight of the patients (42%) with severe pancreatitis tested positive for CRP (Table 4). Procalcitonin was found in eleven of the patients who had tested positive. Of these, four had severe pancreatitis (Table 5).
Antibiotics were administered to 59 patients of whom five had had some kind of bacteria isolated. The other 54 patients were given antibiotics because of clinical indications. Ampicillin sulbactam was administered to 35 patients (32.1%), carbapenems were given to 14 patients (12.8%), and piperacillin tazobactam was given to ten patients (9.17%). Antibiotics were taken for an average of 9.87 days.
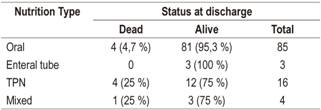
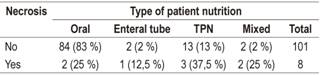
On average, patients went 3.65 days without oral nutrition. Oral therapy was initiated in 85 patients (77.98%), enteral feeding tubes in four patients (3.66%), parenteral nutrition in 16 patients (14.6%) and mixed nutrition in four patients (3.66%) (Tables 6 and 7).
Table 6 Nutritional support received according to Atlanta severity classification, 2012
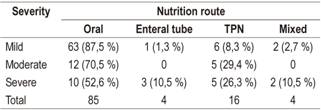
TPN: total parenteral nutrition.
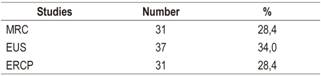
Eighty-two patients (75.22%) had diagnostic studies of their bile ducts: 37 patients (33.94%) with endoscopic ultrasonography (EUS), 31 patients (28.44%) with magnetic resonance cholangiopancreatography (MRC), and 31 patients (28.44%) with ERCP (Table 8). Choledocholithiasis was diagnosed in 24 patients (22.01%), and pancreatic lithiasis was diagnosed in two patients (1.83%). Of the 109 study patients, cholelithiasis was found in 81 patients (74.31%), and biliary sludge was found in 16 patients (14.67%). Cholecystectomies were performed in 55 patients (50.45%): forty-four laparoscopic and nine were open. Eleven patients had previous histories of cholecystectomies.
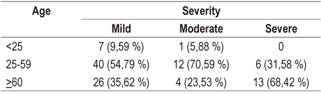
We found that 68% of patients with severe pancreatitis were older than 60 years of age and that no patients under 25 years of age had severe pancreatitis. The chi-squared test (χ2) showed statistical significance for age as a risk factor for severe pancreatitis (p = 0.04) (Table 9).
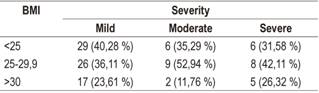
The BMI did not show statistical significance as a risk factor for the severity of pancreatitis (p = 0.8) (Table 10).
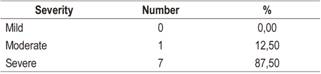
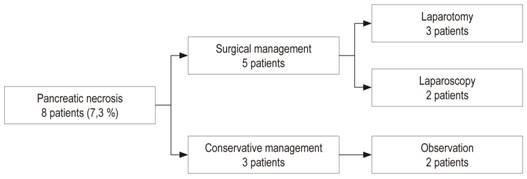
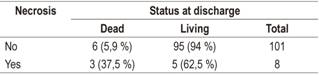
Pancreatic necrosis was documented in eight of the 109 patients included in the study, none of whom had had any previous comorbidity (e.g., hypertension, DM, heart disease, and alcoholism). Most had severe pancreatitis at admission (87%) while one had moderate pancreatitis. The majority of patients with necrosis were male (7 cases), and the majority of these patients (5 patients) were between 25 and 59 years of age. Three patients were over 60 years of age, and none were younger than 25 years. Fifty percent of these patients’ BMIs indicated that they were overweight. Marshall Scores could only be calculated for 5 patients due to lack of data for the others. Three had Marshall Scores less than three. According to the 2012 revised Atlanta classification, seven of the eight patients who had pancreatic necrosis at patients had severe pancreatitis, and one patient had moderate pancreatitis (Table 11).
Of the eight patients who had pancreatic necrosis, five underwent surgery, three by laparotomy and two by laparoscopy-On average, 32.5% of the pancreas was resected. One of the other three patients underwent minimally invasive percutaneous drainage and the other two were treated with conservative management (Figure 2). Of the patients who underwent surgery, two underwent cholecystectomies at the same time.
Enteral tube nutrition was received by one patient (12.5%), parenteral nutrition by three patients (37.5%), mixed nutrition by two patients (25%) and oral nutrition by two patients (25%) (Table 12).
Three of the eight patients (37.5%) who had developed pancreatic necrosis died. All had undergone surgery, two laparoscopic procedures and one open procedure. Two of the three patients (12%) who died had Marshall Scores that were over four at admission and an APACHE II average of 16 (Table 13).
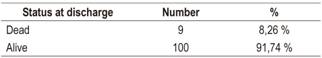
Of the 109 patients included in the study, 100 patients (91.74%) resolved their pancreatitis and left the institution alive. All of the nine patients (8.25%) had severe acute pancreatitis (Tables 14 and 15).
Discussion
Our analysis of the patients included in this found that being over the age of 60 was a risk factor for severity with statistical significance (p = 0.04). An article by Bechien U. Wu et al. that was published in Gastroenterology in 2013 described age as a risk factor for mortality in severe pancreatitis but did not find it to be statistically significant. 5
We found no statistically significant relationship between obesity and severity of pancreatitis (p = 0.8), in contrast to what has been described in the literature. A systematic review published in October 2014 by Rakesh Premkumar et al. found clinical relevance of obesity to acute pancreatitis in 24 studies with evidence level 1A. This indicates that obesity is associated with increased risks of severe acute pancreatitis. The review found only two studies that reported it to be an independent prognostic factor. 6
The Japanese guidelines for management of acute pancreatitis published in 2015 recommend using contrast tomography to identify and diagnose complications such as necrotizing pancreatitis and extension of inflammatory changes. This allows for timely treatment of these patients and improves their prognoses. 7 Nineteen of the patients in our study had severe acute pancreatitis. Of these, only six patients (31.6%) had had CAT scans, and of these four had pancreatic necrosis. Clinical histories contained only inadequate reports of the percentage of patients who had developed necrosis. Of the other four patients with pancreatic necrosis, diagnoses of three were made intraoperatively while one was made by MRC. In addition, it is inferred that the reason many patients did not undergo CT scans was that transferring them was impossible due to the severity of their clinical conditions.
Evidence regarding antibiotic prophylaxis is controversial: multiple controlled clinical trials that compare broad spectrum antibiotics to placebos have not shown statistically significant differences in the incidence of infectious complications, organ dysfunction and mortality. Even though, the incidence of these complications in patients who have received this type of prophylaxis has decreased this practice is not standard even for patients with severe pancreatitis. 4,8
Multiple studies and clinical practice guidelines recommend carbapenems as the best therapeutic broad spectrum antibiotics for treatment of pancreatitis because of their ability to penetrate into pancreatic tissue and proven reductions of mortality. In addition, guidelines propose that indications for administration of antibiotics include pancreatic necrosis of more than 30% to 40% as measured by CAT scan, microbiological isolation of pancreatic collection, and poor clinical response in patients with severe pancreatitis. In this study, the incidence of severe pancreatitis was 17%, but 63% of the patients received antibiotic treatment. Ampicillin sulbactam was used in most cases, followed by carbapenems. This can be explained by the fact that in our environment acute cholecystitis grades II and III is very frequent associated with episodes of pancreatitis. Depending on the institutional protocol, this warrants initiation of antibiotic coverage. 8
Severe pancreatitis associated with complications such as pancreatic necrosis occurs relatively frequently within the natural course of the disease. We found that 8 patients had this complication and that five of these patients (4.6%) developed hemodynamic instability due to poor response to medical treatment. In two cases hemoperitoneum was confirmed, and the patients underwent surgery. The other three were managed medically at the direction of the treating surgeon. Following this sequence, the highest mortality occurred in the group treated surgically with 37.5% (3 patients). This result supports descriptions in a number of series of international cases that indicate that better results are achieved with conservative management. One of these articles is a metaanalysis published by Dr. Venigalla Pratap et al. which reports a statistically significant success rate of 64% for conservative management of pancreatic necrosis (relative risk [RR]: 0.64; 95% confidence interval [CI]: 0.51 to 0.68). The mortality rate of 12% was without statistical significance. 9
Conclusions
This descriptive study establishes patients’ demographic characteristics and development of acute including complications and their handling. It neither intends to standardize causality or management of the pathology described but only documents the experience of a fourth level hospital in order to contribute to the development of randomized studies that will allow establishment of management guidelines. In this way, we hoped to contribute to improving the prognoses of patients who develop acute pancreatitis
Referencias
1. Lankisch PG, Apte M, Banks PA. Acute pancreatitis. Lancet. 2016;386(9988):85-96. doi: 10.1016/S0140-6736(14)60649-8. [ Links ]
2. Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144(6):1252-61. doi: 10.1053/j.gastro.2013.01.068. [ Links ]
3. Haney JC, Pappas TN. Necrotizing pancreatitis: diagnosis and management. Surg Clin North Am. 2007;87(6):1431-46. doi: 10.1016/j.suc.2007.08.013. [ Links ]
4. Loveday BPT, Srinivasa S, Vather R, Mittal A, Petrov MS, Phillips ARJ, et al. High quantity and variable quality of guidelines for acute pancreatitis: a systematic review. Am J Gastroenterol. 2010;105(7):1466-76. doi: 10.1038/ajg.2010.137. [ Links ]
5. Wu BU, Johannes RS, Sun X, Tabak Y, Conwell DL, Banks PA. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57(12):1698-703. doi: 10.1136/gut.2008.152702. [ Links ]
6. Premkumar R, Phillips ARJ, Petrov MS, Windsor JA. The clinical relevance of obesity in acute pancreatitis: Targeted systematic reviews. Pancreatology. 2016;15(1):25-33. doi: 10.1016/j.pan.2014.10.007. [ Links ]
7. Yokoe M, Takada T, Mayumi T, Yoshida M, Isaji S, Wada K, et al. Japanese guidelines for the management of acute pancreatitis: Japanese Guidelines 2015. J Hepatobiliary Pancreat Sci. 2015;22(6):405-32. doi: 10.1002/jhbp.259. [ Links ]
8. Serrablo A, Tejedor L, Martínez J. Antibiotics in severe acute pancreatitis. Cent Eur J Med. 2014;9(4):565-73. doi: 10.2478/s11536-013-0281-3. [ Links ]
9. Mouli VP, Sreenivas V, Garg PK. Efficacy of conservative treatment, without necrosectomy, for infected pancreatic necrosis: a systematic review and meta-analysis. Gastroenterology. 2013;144(2):333-340.e2. doi: 10.1053/j.gastro.2012.10.004. [ Links ]
Received: April 06, 2018; Accepted: June 15, 2018











 texto em
texto em