Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.1 Bogotá Jan./Mar. 2019
https://doi.org/10.22516/25007440.267
Original articles
Endoscopic and Histopathological Characteristics of Colorectal Polyps Resected Endoscopically at a University Institution in Bogotá D. C.
1Clínica Universitaria Colombia. Bogotá D. C., Colombia
2Organización Sánitas. Bogotá D. C., Colombia
Colorectal cancer is one of the most important causes of death in Western countries. Since the progression from adenoma to carcinoma was established, it has been considered that colon polyps are an important risk factor for development of colorectal cancer, hence the importance of knowledge and research about them as well as their detection and resection. In our country there had been no prospective evaluations of the characteristics of colorectal polyps, so we considered this study to determine the endoscopic and histopathological characteristics of colonic polyps found and resected through colonoscopy to be of great importance.
This descriptive and observational study includes analysis of polyps resected from patients inthe Gastroenterology and Digestive Endoscopy service of the Clínica Universitaria Colombia. Sample size was calculated probabilistically (n = 306 resected polyps). Contrary to reports in the literature, most of the polyps detected in our study (170) were adenomatous (55.6%). The highest percentage (86%) were tubular which is consistent with the literature. Most of them had low grade dysplasia. Only two of our patients had polyps found whose histology indicated adenocarcinoma.
Keywords: Polyps; colorectal cancer; resection; histopathology
El cáncer colorrectal es una de las causas de mortalidad más importantes en los países occidentales. Desde cuando se estableció la progresión de adenoma a carcinoma, se ha considerado que los pólipos del colon son un factor de riesgo importante para desarrollar el cáncer colorrectal, por esta razón es importante el conocimiento, detección y resección, e investigación del tema. En Colombia no se han realizado estudios prospectivos que evalúen las características de los pólipos colorrectales, razón por la cual se considera de gran importancia la realización de este estudio con el objetivo de determinar las características endoscópicas e histopatológicas de los pólipos colónicos encontrados y resecados mediante colonoscopia.
Se realizó un estudio observacional descriptivo, mediante el análisis de los pólipos resecados en pacientes del servicio de gastroenterología y endoscopia digestiva de la Clínica Universitaria Colombia. Se calculó un tamaño de muestra de forma probabilística (n = 306 pólipos resecados). En cuanto a la histología, y contrario a lo informado en la literatura, la mayoría de los pólipos detectados en nuestro estudio (170) fue de tipo adenomatoso (55,6 %). El mayor porcentaje de ellos (86 %) correspondió al tipo tubular, hallazgo acorde con lo mencionado en la literatura, la mayoría de ellos con displasia de bajo grado. Solo en 2 de nuestros pacientes se realizó el hallazgo de pólipos cuya histología diagnosticó la presencia de adenocarcinoma.
Palabras clave: Pólipos; cáncer colorrectal; resección; histopatología
Introduction
Worldwide, colorectal cancer is one of the most important causes of morbidity and mortality, and its incidence is constantly increasing. Progression from adenoma to carcinoma has been clearly established, and it is thought that colon polyps are an important risk factor for development of colorectal cancer. For this reason, knowledge, detection, resection and histopathological analysis are important. 1 Polyps are mucosa-dependent masses that protrude towards open space (in this case intestinal) and that can be characterized by their macroscopic appearance, size, number and by whether or not they have a pedicle. They can be divided into neoplastic and non-neoplastic. Depending upon whether a diagnosis is histologically confirmed, either surgery should be performed or the patient should be monitored. 2
In developed countries, colorectal cancer is the third most common cancer and is the second leading cause of cancer death. A 5-year survival rate of 90% has been established when it is diagnosed as localized disease, but this drops to 68% when there is nodal involvement, and drops all the way to 10% when there is metastasis. Based on these considerations and the knowledge that 90% of cases of sporadic colorectal cancer are generated in the adenoma-carcinoma sequence, screening programs, early detection of adenomatous lesions, and prevention through polypectomy implemented in recent years have caused mortality from colorectal cancer to decrease. 3,4,5
Adenomatous polyps are common in adults over 50 years of age, but only a few will become adenocarcinomas. Polyp histology and size determine their clinical importance. Neoplastic high-risk adenomas with tubular histology that measure more than 10 mm in size, those with hairy histology independent of size, and those with high-grade dysplasia are considered to be high risk. Also, whenever there are three or more adenomas, the risk is considered to be high. 6,7
Polyps measuring less than 5 mm in diameter have classically been considered to be non-neoplastic lesions, but some studies have shown that 30% to 50% of them may be adenomas and that up to 4.4% of these may present high risk characteristics. 8,9
Based on these data, the universally adopted strategy until now has been resection and histopathological study of all polyps. However, since 40% to 50% of colonoscopies find polyps, resection and study of all polyps is very costly for health care systems. In order to reduce costs without increasing risks to patients, a search for strategies to identify which lesions must be analyzed histologically, and which do not need to be analyzed, has been conducted. 10. For this reason, the resect and discard strategy has arisen. It proposes the possibility of differentiating between hyperplastic and adenomatous histology of small polyps based on the use of endoscopic technologies to determine whether there is a need to send a specimen to pathology. Although this strategy seems promising, up to now there has not been enough data in the literature to make a any formal recommendation. 11,12
Justification
In our environment, morphological characteristics of polyps including size, number, and correlation with histopathological findings were unknown. This prospective study shows characteristics of colorectal polyps in our population.
Objectives
The objective of this study was to determine endoscopic and histopathological characteristics of colon polyps found and resected by colonoscopy in patients treated in our institution. We have evaluated the frequency and location of polyps in the study population and described the incidence of malignant pathology patients who underwent polypectomies.
Patients and method
Study Design
This descriptive observational study was performed through analysis of colonoscopy and histopathology reports of polyps completely resected with endoscopic polypectomy loops or forceps from patients of the gastroenterology service of the Clínica Universitaria Colombia between January and March 2016. The colonoscopies and resection of the polyps were performed by gastroenterologists and resident physicians of the gastroenterology service according to the protocols of the institution.
Population
The sampling frame consisted of all the polyps resected in the service and study histopathologically. Polyps were extracted from adult patients 18 years or older who had been referred to the service for outpatient endoscopy. A sample size of n = 306 resected polyps was calculated probabilistically, and samples without pathology reports or clinical data were excluded.
Statistical Analysis
Measures of frequency and central tendency were analyzed, and the distribution of normality of variables of interest was evaluated using P-P and Q-Q charts and the Shapiro-Wilk test. Categorical data were analyzed using the nonparametric Mann-Whitney U test, the chi squared (χ2) test, and Fisher’s exact test. The nonparametric χ2 test was used to identify the relationship between macroscopic findings, relevant clinical history, and findings of dysplasia in the histopathology study provided that the Cochrane assumptions for the test were met (Less than 20% of the cells must have expected values of less than 5 and no cell should have an expected value of less than one.). 95% confidence intervals (CI) were calculated for each estimator. P values for hypothesis testing were considered significant when p <0.05. The data was analyzed with STATA 13.0.
Results
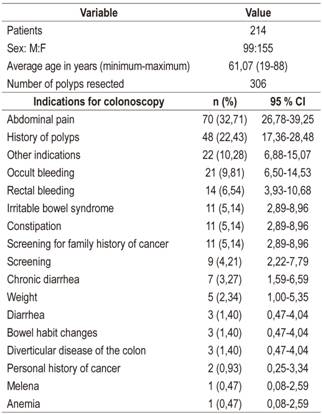
The sample size was completed after 2 months and 7 days during which time 1,808 colonoscopies were performed in our institution. In total, 306 polyps resected by endoscopic polypectomy of the colon and rectum were included in the study. Each polyp was completely resected with either biopsy forceps or with a polypectomy loop in procedures performed on 214 patients (115 women and 99 men). The average age of the patients was 61.07 years (range: 19 to 88). The mean number of polyps resected per patient was 1.4 (minimum 1 and maximum 8). Abdominal pain (32.71%) and a history of polyps were the main indications for performance of colonoscopy for the patients included in the study (Table 1).
Macroscopic findings from colonoscopy showed that the resected polyps were mostly located in the sigmoid colon (n = 89, 29.08%, 95% CI: 24.28-34.41), followed by the rectum (n = 67, 21.90%; 95% CI: 17.63-26.86). They were less frequently resected in the cecum (n = 16, 5.23%, 95% CI: 3.24-8.32). The most frequent morphology of the resected polyps was sessile (n = 245, 80.07%, 95% CI: 75.23-84.16). Most of the polyps measured less than 5 mm (n = 222, 72.55%, 95% CI: 67.29-77.25), and most were adenomatous (n = 169, 55.23%, 95% CI: 49.63-60.70) (Figure 1).
The great majority of polyps were resected using biopsy forceps (n = 255, 83.33%, 95% CI: 78.75-87.09). Some indicators of the quality of the conditions under which colonoscopies were performed in these 214 patients show that 3.74% of them were incomplete. Most of these were due to technical problems or stenoses which occurred in 2.8% of the patients. Other factors related to the quality of the procedure did not exceed 1%. Adenomatous histology was found in 169 polyps, mixed histology in 11, low-grade dysplasia in 173 (96.11%; 95% CI: 92.19-98.10) and tubular type polyps in 148 (82.22%, 95% CI: 75.98-87.12) (Table 2).
Table 2 Characteristics of colonoscopy and histopathology reports
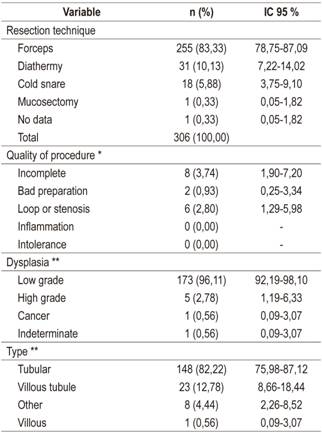
* 214 colonoscopy procedures were performed of which 8 were incomplete. ** These were the degrees of dysplasia and the type of adenoma found in the 180 polyps with adenomatous or mixed histology.
The clinical conditions most frequently found in this group of patients who had undergone endoscopic polypectomies were internal hemorrhoids (37.85%), diverticula in the rectum and sigmoid (24.30%), external hemorrhoids (20.09%) and diverticulosis (11.21%).
Bivariate analysis using the χ2 and Fisher’s exact test allowed identification of the relationship of a number of demographic and clinical characteristics with varying degrees of dysplasia. Statistically significant differences were found for the location of the polyp (p = 0.000), size of the polyp (p = 0.002), personal history of polyps (p = 0.004), history of irritable bowel syndrome (p = 0.001) and rectal bleeding (p = 0.013). Other variables of interest did not show any statistically significant associations.
Discussion
The number of cases of colorectal cancer, already one of the most important causes of death in Western countries, has increased in recent decades. Since progression from adenoma to carcinoma was established more than 70 years ago, colon polyps have been considered to be important risk factors for colorectal cancer. This makes knowledge and research about this topic, especially about detection and resection an important subject of study. 13
Gastrointestinal polyps can be characterized macroscopically by size and number and by the presence or absence of a pedicle. Colorectal polyps can be divided into neoplastic and non-neoplastic polyps. 14
Hyperplastic polyps are the most common non-neoplastic lesions of the colon. Histologically they have normal cellular components but have not advanced to dysplasia. They are usually smaller than 5 mm across, and mostly innocuous, and can be found throughout the colon although they occur most frequently in the rectum and the sigmoid colon. Their prevalence increases with age and can be as high as 30% in people over 50 years old. Since they usually have no symptoms, they are most often found incidentally in colonoscopies. 15
Inflammatory pseudopolyps correspond to inflamed areas of the mucosa that project into the adjacent mucosa. They usually result from a localized or diffuse inflammatory response such as inflammatory bowel disease. These polyps are not considered precursors of colorectal cancer. 2,15
Adenomatous polyps are benign epithelial neoplastic tumors which are almost always asymptomatic. Morphologically they are classified as sessile, pedunculated and flat. The clinical importance of adenomatous polyps lies in their variable potential for malignancy. They manifest as obvious digestive bleeding in some cases but manifest in others as occult blood in the stool. The adenoma-carcinoma sequence is well known, and it is accepted that 80% to 90% of all colorectal cancers originate as adenomas. 16
The prevalence of colon adenomas increases in direct proportion to age. According to the literature, approximately 12% to 30% of people have adenomas from the fifth decade of life. Of these adenomas, close to 25% are considered to have high risks of becoming malignant. 17 The World Health Organization (WHO) classifies adenomas as
Tubular (less than 25% villous architecture): 80% -86%.
Tubulovillous (between 25% and 75% villous architecture): 8% -16%.
Villous (at least 75% villous architecture): 3% -16%. 18
By definition, all adenomas have some degree of dysplasia, although it is often low grade. Dysplasia of adenomas is classified as low-grade (mild to moderate) or high-grade (severe, includes carcinoma in situ). 18
Only 5% of adenomas are at risk of malignant transformation. The probability of high grade dysplasia and carcinomatous transformation increases as the size of the polyp increases, and is especially high for polyps that measure more than one cm across. This probability also increases when for partially and completely villous adenomas, multiple adenomas, and when a patient’s age at diagnosis is over 60 years. A polyp is considered to have advanced histology when it is larger than 10 mm, when its villous component is greater than 25%, and when high-grade dysplasia is present. 19
In contrast to reports in the literature, most of the polyps detected in our study (170) were adenomatous (55.6%). The highest percentage (86%) were tubular, which is in accordance with the literature, and most had low grade dysplasia.
Serrated adenomas are a subtype of adenomatous polyps whose dysplastic epithelia have growth patterns similar to those of hyperplastic polyps. They are slightly more common in the left colon. 20,21 In our study, three serrated polyps (0.98% of the sample) were found.
Polyp size has been shown to be related to potential for malignancy. Some studies have shown that 30% to 50% of polyps that measure less than 5 mm have adenomatous structures, and that only 1.3% of adenomas measuring less than 10 mm develop into malignancy. This rate increases up to 10% when there is a villous component and increases up to 27% when there is significant dysplasia. Adenomas that are between 10 mm and 2 cm have a 5% risk of developing into carcinoma by the time resection. The risk is between 10% and 20% for those that measure more than 2 cm. The degree of dysplasia is a risk factor for malignancy, regardless of size. 22
Early detection of colorectal cancer is essential for improving treatment options and reducing mortality. In terms of secondary prevention, endoscopic resection of adenomatous polyps reduces the incidence of colorectal cancer. For this reason, the accepted treatment for colorectal polyps, regardless of size, architecture or degree of dysplasia, is complete resection. 1,23
Colonoscopy is the preferred screening strategy for colorectal cancer. The incidence of this disease has been reduced by up to 90% in patients who have undergone polypectomies compared to patients in three reference groups: two cohorts in which colorectal polyps were not resected and a record of the general population. Colonoscopy can be completed with minimal risk in more than 95% of cases. Colonoscopic screening has been shown to be cost-effective. 24
Recently, strategies intended to predict the potential for malignancy of a polyp have been described. The intention is to way determine whether a polyp can be resected and discarded. The strategy is called “predict, resect, and discard.” This type of strategy is used especially for polyps measuring less than 5 mm, and less frequently for polyps measuring between 6 and 9 mm. Nevertheless, this is still a source of intense debate. 25,26
We only found two polyps whose histology diagnosed adenocarcinoma. One was a 20 mm polyp taken from a 43 year old woman, and the other was a polyp that measured less than 5 mm taken from a 77 year old woman.
This study has identified characteristics of polyps resected from our patients and highlights our finding that more than 50% of the polyps resected in our institution were adenomatous. In one case, histopathological report for a resected polyp measuring only 5 mm showed neoplastic pathology. For this reason, we the resection of the polyps found during colonoscopies to be of great importance in our population. Resected polyps should be sent for histopathological study and should not be discarded.
Referencias
1. Zauber AG, Winawer SJ, O’Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366(8):687-96. doi: 10.1056/NEJMoa1100370. [ Links ]
2. IJspeert JE, Medema JP, Dekker E. Colorectal neoplasia pathways: state of the art. Gastrointest Endosc Clin N Am. 2015;25(2):169-82. doi: 10.1016/j.giec.2014.11.004. [ Links ]
3. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893-917. doi: 10.1002/ijc.25516. [ Links ]
4. Piñeros M, Murillo RH, Instituto Nacional de Cancerología, Bogotá, D. C . Incidencia de cáncer en Colombia: importancia de las fuentes de información en la obtención de cifras estimativas. Rev Colomb Cancerol. 2004;8(1):5-14. [ Links ]
5. Rex DK, Lehman GA, Hawes RH, Ulbright TM, Smith JJ. Screening colonoscopy in asymptomatic average-risk persons with negative fecal occult blood tests. Gastroenterology. 1991;100(1):64-7. [ Links ]
6. Winawer SJ, Zauber AG, Fletcher RH, Stillman JS, O’Brien MJ, Levin B, et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. Gastroenterology. 2006;130(6):1872-85. doi: 10.1053/j.gastro.2006.03.012. [ Links ]
7. Paggi S, Rondonotti E, Amato A, Terruzzi V, Imperiali G, Mandelli G, et al. Resect and discard strategy in clinical practice: a prospective cohort study. Endoscopy. 2012;44(10):899-904. doi: 10.1055/s-0032-1309891. [ Links ]
8. Fossi S, Bazzoli F, Ricciardiello L, Nicolini G, Zagari RM, Pozzato P, et al. Incidence and recurrence rates of colorectal adenomas in first-degree asymptomatic relatives of patients with colon cancer. Am J Gastroenterol. 2001;96(5):1601-4. doi: 10.1111/j.1572-0241.2001.03784.x. [ Links ]
9. Rex DK, Khan AM, Shah P, Newton J, Cummings OW. Screening colonoscopy in asymptomatic average-risk African Americans. Gastrointest Endosc. 2000;51(5):524-7. [ Links ]
10. Rex DK, Lehman GA, Ulbright TM, Smith JJ, Pound DC, Hawes RH, et al. Colonic neoplasia in asymptomatic persons with negative fecal occult blood tests: influence of age, gender, and family history. Am J Gastroenterol. 1993;88(6):825-31. [ Links ]
11. Vu HT, Sayuk GS, Gupta N, Hollander T, Kim A, Early DS. Patient preferences of a resect and discard paradigm. Gastrointest Endosc. 2015;82(2):381-384.e1. doi: 10.1016/j.gie.2015.01.042. [ Links ]
12. Wilson AI, Saunders BP. New paradigms in polypectomy: resect and discard, diagnose and disregard. Gastrointest Endosc Clin N Am. 2015;25(2):287-302. doi: 10.1016/j.giec.2014.12.001. [ Links ]
13. Mandel JS, Church TR, Bond JH, Ederer F, Geisser MS, Mongin SJ, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343(22):1603-7. doi: 10.1056/NEJM200011303432203. [ Links ]
14. Heitman SJ, Ronksley PE, Hilsden RJ, Manns BJ, Rostom A, Hemmelgarn BR. Prevalence of adenomas and colorectal cancer in average risk individuals: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2009;7(12):1272-8. doi: 10.1016/j.cgh.2009.05.032. [ Links ]
15. Kronborg O, Fenger C, Olsen J, Jørgensen OD, Søndergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348(9040):1467-71. doi: 10.1016/S0140-6736(96)03430-7. [ Links ]
16. Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M, et al. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988;319(9):525-32. doi: 10.1056/NEJM198809013190901. [ Links ]
17. Citarda F, Tomaselli G, Capocaccia R, Barcherini S, Crespi M; Italian Multicentre Study Group. Efficacy in standard clinical practice of colonoscopic polypectomy in reducing colorectal cancer incidence. Gut. 2001;48(6):812-5. [ Links ]
18. Bujanda L, Cosme A, Gil I, Arenas-Mirave JI. Malignant colorectal polyps. World J Gastroenterol. 2010;16(25):3103-11. [ Links ]
19. Richter JM, Campbell EJ, Chung DC. Interval colorectal cancer after colonoscopy. Clin Colorectal Cancer. 2015;14(1):46-51. doi: 10.1016/j.clcc.2014.11.001. [ Links ]
20. Bordaçahar B, Barret M, Terris B, Dhooge M, Dreanic J, Prat F, et al. Sessile serrated adenoma: from identification to resection. Dig Liver Dis. 2015;47(2):95-102. doi: 10.1016/j.dld.2014.09.006. [ Links ]
21. Abdeljawad K, Vemulapalli KC, Kahi CJ, Cummings OW, Snover DC, Rex DK. Sessile serrated polyp prevalence determined by a colonoscopist with a high lesion detection rate and an experienced pathologist. Gastrointest Endosc. 2015;81(3):517-24. doi: 10.1016/j.gie.2014.04.064. [ Links ]
22. Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson DA, Levin TR. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143(3):844-857. doi: 10.1053/j.gastro.2012.06.001. [ Links ]
23. Winawer SJ, Zauber AG, Ho MN, O’Brien MJ, Gottlieb LS, Sternberg SS, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329(27):1977-81. doi: 10.1056/NEJM199312303292701. [ Links ]
24. Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011;154(1):22-30. doi: 10.7326/0003-4819-154-1-201101040-00004. [ Links ]
25. Kessler WR, Imperiale TF, Klein RW, Wielage RC, Rex DK. A quantitative assessment of the risks and cost savings of forgoing histologic examination of diminutive polyps. Endoscopy. 2011;43(8):683-91. doi: 10.1055/s-0030-1256381. [ Links ]
26. Hassan C, Pickhardt PJ, Rex DK. A resect and discard strategy would improve cost-effectiveness of colorectal cancer screening. Clin Gastroenterol Hepatol. 2010;8(10):865-869.e1-3. doi: 10.1016/j.cgh.2010.05.018. [ Links ]
Received: July 18, 2018; Accepted: September 12, 2018











 text in
text in