Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.1 Bogotá Jan./Mar. 2019
https://doi.org/10.22516/25007440.203
Case report
Case Report of Vedolizumab Treatment of Refractory Ulcerative Colitis Associated with Psoriasis
1Especialista en medicina interna, gastroenterología y endoscopia digestiva, Unidad de Gastroenterología, Hospital Pablo Tobón Uribe. Medellín, Colombia
2Médica, Pontificia Universidad Javeriana de Cali. Cali, Colombia
The patient had a long history of difficult to control psoriasis and ulcerative colitis and was dependent on corticosteroids. Multiple treatment schemes including several attempts with tumor necrosis factor (anti-TNF) antagonists had had acceptable clinical responses but subsequently lost effectiveness. During acute exacerbation of colitis, vedolizumab was used and achieved remarkable clinical improvement. During maintenance, deep healing was achieved (endoscopic and histological normalization). In addition, there was significant improvement of psoriasis lesions during follow-up.
This is the first case to be published of the use of Vedolizumab to treat this condition in Colombia.
Keywords: Biological therapy; psoriasis; ulcerative colitis; vedolizumab
Paciente con historia de psoriasis de difícil control y colitis ulcerativa de larga evolución, corticodependiente, requirió múltiples esquemas de tratamientos incluidos varios antagonistas de factor de necrosis tumoral (anti-TNF), con lo cual tuvo respuesta clínica aceptable y posterior pérdida de efectividad. En una exacerbación aguda de la colitis se utilizó vedolizumab, con lo cual se logró una notable mejoría clínica, y en el mantenimiento se llegó a cicatrización profunda (normalización endoscópica e histológica), además de mejoría significativa de las lesiones de psoriasis en el seguimiento a 12 meses.
En lo conocido hasta ahora, es el primer caso con el uso de vedolizumab en esta indicación publicado en Colombia.
Palabras clave: Terapia biológica; psoriasis; colitis ulcerativa; vedolizumab
Introduction
Inflammatory bowel disease (IBD) includes Crohn’s disease (CD), ulcerative colitis (UC) and indeterminate colitis. The latter term is currently used by pathologists to categorize colectomy specimens which either have superimposed findings or cannot be defined as either CD or UC. 1
IBD’s etiology and exact pathogenesis are still unknown, but the current hypothesis relates to dysregulation of the gastrointestinal immune system in genetically predisposed individuals. 2 Some authors mention the importance of pathogenic pathways. These include interleukin 23 (IL-23), which mediates microbial defense and intestinal inflammation, and two genes, IL-23 receptor (IL-23R) and interleukin 12B (IL-12B). 3,4 These genes and others such as protein tyrosine kinase 2 (TYK2), Janus 2 kinase (JAK2), the signal transducer, and transcription activator 3 (STAT3) are also associated with psoriasis. 2
The incidence of CD and UC is 3.8 to 7.5 times higher in patients with psoriasis than in the general population. 5 The hypothesis that there are inflammatory pathways common to both the skin and the intestine is supported by the fact that anti-tumor necrosis factor alpha (anti-TNFα) monoclonal antibodies such as infliximab and adalimumab have a beneficial effect on both pathologies. IBD and psoriasis may overlap, even if psoriasis can paradoxically occur in people who have received anti-TNF for IBD. It is estimated that psoriasiform lesions on the skin can occur in 1.62% -8.8% of patients with IBD who are treated with anti-TNF. 6,7 The appearance of psoriasiform lesions is not associated with sex, duration of treatment or activity of IBD. 8,9,10 In many individuals, controlling IBD could have a positive impact on psoriasis lesions leading to improvement or resolution.
UC is the most common form of IBD. A study conducted at Hospital Pablo Tobón Uribe (HPTU) in Medellin, Colombia found that the relationship between UC and CD was 4.9 to 1: UC occurred in in 80.7% of the IBD patients while CD was found in only 15.8%. 11 The incidence of UC varies between 1.2 and 20.3 cases per 100,000 people/year depending on the population studied. 7 Its etiology is unknown and multifactorial. Family history of IBD is reported to increase the risk of IBD while appendectomies in young people and smoking may be protective factors. 1,12 UC is characterized by of chronic and diffuse inflammation in the rectal and colonic mucosa. 1 In the natural course of the disease, there are frequent outbreaks of inflammatory activity with periods of remission, and the disease tends to recur. 13
Clinical case
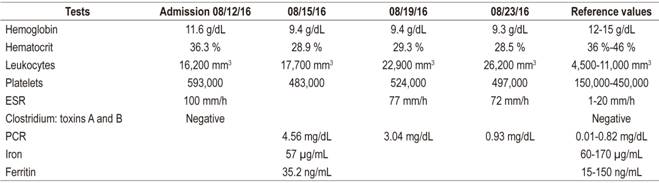
The patient was a 50 year old woman who had been diagnosed with UC in 2009 and had been diagnosed with psoriasis in 1996. She came to the HPTU in August 2016 after suffering anal pain, dyschezia and watery bloody diarrhea for at least two months. In the last week before coming to the hospital, her symptoms became exacerbated to the point of 10-12 stools per day and colicky abdominal pain daily. She reported intense pruritus and frequent scratching of skin lesions. Physical examination showed mucocutaneous pallor; dehydration, fever, with abdominal pain without peritoneal irritation, multiple active scaly plaques on her face, trunk and extremities, multiple hyperpigmented macules and erosions on the skin which had been scratched (Figures 1A and 1B). She was hospitalized and laboratory tests done upon admission (Table 1) showed mild anemia and marked elevation of acute phase reactants. A colonoscopy was only able to reach the splenic angle due to severe inflammation, easy bleeding in response to friction of the equipment, and a high risk of perforation. It was decided to suspend the colonoscopy at that point (Figure 2). Tests for infections including tests for Clostridium toxins A and B for negative and cytomegalovirus [CMV] were negative. Initially, 100 mg of hydrocortisone was administered every 8 hours for 5 days with 1 g granules of mesalazine administered orally every 8 hours, and an additional 4 g of mesalazine administered by enema once a day.
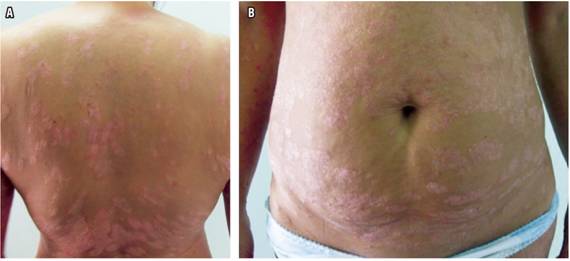
Figure 1 A. Photograph of the back of the patient showing multiple scaly, erythematous-edematous lesions with scratchy erosions. B. Photo of the skin of the abdomen showing multiple scaly erythematous plaques, with scratchy erosions.
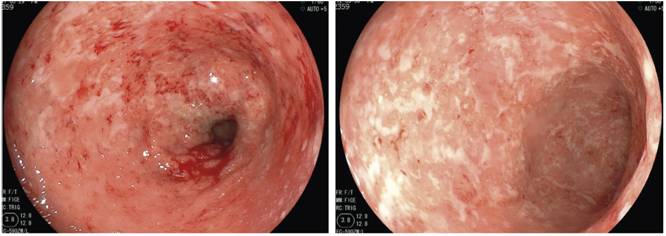
Figure 2 Colonoscopy showing severe inflammatory changes due to loss of normal vascular pattern. Marked edema, erythema, homogeneous multiple erosions and mucosa friable due to touch.
The patient’s clinical history prior to hospitalization was reviewed for details of previous treatment. Multiple schemes were described including 3 g of mesalazine granules per day, 100 mg of azathioprine/day, fortnightly parenteral iron for anemia, and 5 mg/kg of infliximab for 5 years. Infliximab had lost its effectiveness in the year prior to hospitalization and the dosage had been increased to 10 mg/kg without adequate response. The patient had then been switched to 40 mg of adalimumab every two weeks (2014-2015).
Adalimumab had maintained an average defecation frequency of between 3 and 6 stools per day without bleeding, but at the end of 2015 it the patient’s condition including her skin lesions worsened. Adalimumab was replaced 45 mg of ustekinumab administered subcutaneously every 2 months (2015-2016). Minimal improvement in digestive symptoms occurred, but skin lesions were very poorly controlled. On the recommendation of the dermatology department, her medication was changed to secukinumab in March 2016. She continued taking it together with mesalazine and azathioprine until the date of admission to our institution. The poor response of her gastrointestinal manifestations led to her hospitalization.
During hospitalization, high fecal output with six to seven bloody stools between 6-7 daily was observed. She had progressive anemia and persistently high levels of acute phase reactants (Table 1). A gastroenterology staff meeting decided to start vedolizumab with 300 mg at week 0, week 2, week 6 and then every 8 weeks.
During outpatient follow-up, the patient reported marked improvement and become asymptomatic three months after starting treatment. Normalization of acute phase reactants and normalization of hemoglobin were observed without requiring parenteral iron administration. In addition, azathioprine was discontinued. Methotrexate was added at 12.5 mg/week because its profile is better for dermatological symptoms.
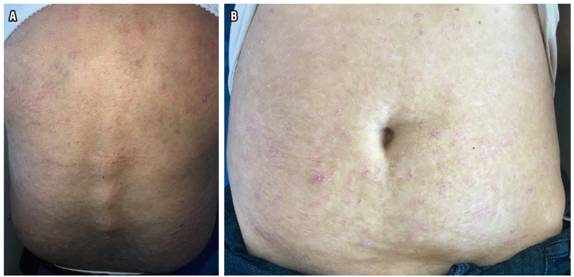
Endoscopic follow-up showed normalization of the mucosa with histologically normal biopsies. The patient said that complete control of pruritus had been achieved and that she no longer required use of topical steroids.
At the 12-month follow-up, the patient had no digestive symptoms which were in deep remission and had no evidence of activity of her psoriasis lesions. She is scheduled for follow-up examinations every 6 months and clinical evaluations between 3 and 6 months.
Discussion
Treatment of IBD has mainly been based on the step-up strategy. For mild UC, initial management with 5-aminosalicylates (5-ASA) is considered appropriate both for induction of remission and for maintenance. Short, 2 to 4 month, courses of steroids are indicated for patients who fail initial treatment with 5-ASA and for those with moderate to severe disease. Corticosteroid dependent patients, patients who have recurrences, and patients who experience loss of efficacy of glucocorticoids are candidates for immunomodulators such as thiopurine (azathioprine, 6-mercaptopurine) and methotrexate. 14 Anti-TNFs such as infliximab, adalimumab, golimumab and certolizumab are indicated for corticosteroid-resistant (non-steroid-responsive) and corticosteroid dependent individuals. 15. Primary failure of treatment, absence of any significant clinical response, occurs in 10% to 40% of CD cases and in almost 50% of UC patients. (15- 18) In addition, secondary failure of treatment (lack of sustained response during 12 months of continuous treatment) has been described in up to two thirds of CD patients. 14,19,20 Persistent inflammation despite optimal treatment using the standard dosage of anti-TNF and other drugs is a clear indication for increasing the dosage or shortening the intervals between administration of anti-TNF, as was done with this patient. 15
New treatment schemes are currently being used for CU. These schemes have different mechanisms of action that seem promising for patients who are refractory to anti-TNF. There is a growing body of evidence supporting usage of vedolizumab, a selective anti-integrin α4β7 antibody in the gastrointestinal tract, for treatment of patients with IBD, especially for UC. 1,12,21,22 It has even been used in cases of psoriasiform rashes associated with the use of anti-TNF. 23 This medication has been approved by the National Institute for Food and Drug Surveillance (INVIMA) in February 2016 for treatment of IBD in Colombia for adult patients with moderate-severe active disease whose response has been inadequate, who present progressive losses, or who are intolerant to steroids, immunomodulators or anti-TNFα.
Despite inadequate scientific evidence about vedolizumab’s impact on psoriasis, we decided to use it in this patient since there was a clear predominance of gastrointestinal manifestations which could have led to major complications such as severe bleeding, anemia, need for transfusions of blood products, toxic megacolon, perforations and even death. In addition, other forms of medical management available had already been exhausted. With this intervention we achieved the control of both pathologies as shown by the evidence of deep healing of the colonic mucosa and control of psoriasis at the 12-month follow-up (Figures 3A and 3B). The notable improvement of our patient’s skin lesions was an additional clinical gain that has had a very positive impact on her quality of life. We consider that case series and controlled studies are required to evaluate the impact of this medication on psoriasis lesions. This is the first published case of the use of vedolizumab in a Colombian patient with refractory UC and psoriasis.
Referencias
1. Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders. J Crohns Colitis. 2017;11(6):649-670. doi: 10.1093/ecco-jcc/jjx008. [ Links ]
2. Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361(21):2066-78. doi: 10.1056/NEJMra0804647. [ Links ]
3. Duerr RH, Taylor KD, Brant SR, Rioux JD, Silverberg MS, Daly MJ, et al. A genome-wide association study identifies IL23R as an inflammatory bowel disease gene. Science. 2006;314(5804):1461-1463. Doi:10.1126/science.1135245. [ Links ]
4. Ellinghaus D, Ellinghaus E, Nair RP, Stuart PE, Esko T, Metspalu A, et al. Combined analysis of genome-wide association studies for Crohn disease and psoriasis identifies seven shared susceptibility loci. Am J Hum Genet. 2012;90(4):636-47. doi: 10.1016/j.ajhg.2012.02.020. [ Links ]
5. Najarian DJ, Gottlieb AB. Connections between psoriasis and Crohn’s disease. J Am Acad Dermatol. 2003;48(6):805-824. Doi: 10.1067/mjd.2003.540. [ Links ]
6. Cleynen I, Van Moekercke W, Juergens M, Ballet V, Drobne D, Vandecandelaere P, et al. Anti-TNF induced cutaneous lesions in IBD patients: Characterization and search for predisposing factors. Gut. 2010;59(suppl 3):A1. [ Links ]
7. Afzali A, Wheat CL, Hu JK, Olerud JE, Lee SD. The association of psoriasiform rash with anti-tumor necrosis factor (anti-TNF) therapy in inflammatory bowel disease: a single academic center case series. J Crohns Colitis. 2014;8(6):480-8. doi: 10.1016/j.crohns.2013.10.013. [ Links ]
8. Cullen G, Kroshinsky D, Cheifetz AS, Korzenik JR. Psoriasis associated with anti-tumour necrosis factor therapy in inflammatory bowel disease: a new series and a review of 120 cases from the literature. Aliment Pharmacol Ther. 2011;34(11-12):1318-27. doi: 10.1111/j.1365-2036.2011.04866.x. [ Links ]
9. Fiorino G, Allez M, Malesci A, Danese S. Review article: anti TNF-alpha induced psoriasis in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2009;29(9):921-7. doi: 10.1111/j.1365-2036.2009.03955.x. [ Links ]
10. Rahier JF, Buche S, Peyrin-Biroulet L, Bouhnik Y, Duclos B, Louis E, et al. Severe skin lesions cause patients with inflammatory bowel disease to discontinue anti-tumor necrosis factor therapy. Clin Gastroenterol Hepatol. 2010;8(12):1048-55. doi: 10.1016/j.cgh.2010.07.022. [ Links ]
11. Juliao F, Ruiz M, Flórez J, Donado J, Marín J, Arango C, et al. Fenotipo e historia natural de la enfermedad inflamatoria intestinal en un centro de referencia en Medellín-Colombia. Rev Col Gastroenterol. 2010;25(3):240-51. [ Links ]
12. Yamamoto-Furusho JK, Bosques-Padilla F, de-Paula J, Galiano MT, Ibañez P, Juliao F, et al. Diagnosis and treatment of inflammatory bowel disease: First Latin American Consensus of the Pan American Crohn’s and Colitis Organisation. Rev Gastroenterol Mex. 2017;82(1):46-84. doi: 10.1016/j.rgmx.2016.07.003. [ Links ]
13. Marín-Jiménez I, Menchén-Viso L, Gomollón-García F. Diagnóstico diferencial de la enfermedad inflamatoria intestinal. Elsevier; 2012. [ Links ]
14. Nielsen OH, Bjerrum JT, Herfarth H, Rogler G. Recent advances using immunomodulators for inflammatory bowel disease. J Clin Pharmacol. 2013;53(6):575-88. doi: 10.1002/jcph.2. [ Links ]
15. Nielsen OH, Ainsworth MA. Tumor necrosis factor inhibitors for inflammatory bowel disease. N Engl J Med. 2013;369(8):754-62. doi: 10.1056/NEJMct1209614. [ Links ]
16. Rutgeerts P, Sandborn WJ, Feagan BG, Reinisch W, Olson A, Johanns J, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med . 2005;353(23):2462-76. doi: 10.1056/NEJMoa050516. [ Links ]
17. Reinisch W, Sandborn WJ, Hommes DW, D’Haens G, Hanauer S, Schreiber S, et al. Adalimumab for induction of clinical remission in moderately to severely active ulcerative colitis: results of a randomised controlled trial. Gut . 2011;60(6):780-7. doi: 10.1136/gut.2010.221127. [ Links ]
18. Sandborn WJ, van Assche G, Reinisch W, Colombel JF, D’Haens G, Wolf DC, et al. Adalimumab induces and maintains clinical remission in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2012;142(2):257-65.e1-3. doi: 10.1053/j.gastro.2011.10.032. [ Links ]
19. Colombel JF, Sandborn WJ, Rutgeerts P, Enns R, Hanauer SB, Panaccione R, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn’s disease: the CHARM trial. Gastroenterology. 2007;132(1):52-65. doi: 10.1053/j.gastro.2006.11.041. [ Links ]
20. Sands BE, Anderson FH, Bernstein CN, Chey WY, Feagan BG, Fedorak RN, et al. Infliximab maintenance therapy for fistulizing Crohn’s disease. N Engl J Med . 2004;350(9):876-85. doi: 10.1056/NEJMoa030815. [ Links ]
21. Garnock-Jones KP. Vedolizumab: a review of its use in adult patients with moderately to severely active ulcerative colitis or Crohn’s disease. BioDrugs. 2015;29(1):57-67. doi: 10.1007/s40259-014-0113-2. [ Links ]
22. Colombel JF, Sands BE, Rutgeerts P, Sandborn W, Danese S, D’Haens G, et al. The safety of vedolizumab for ulcerative colitis and Crohn’s disease. Gut . 2017;66(5):839-851. doi: 10.1136/gutjnl-2015-311079. [ Links ]
23. Hirsch A, Colman RJ, Lang GD, Rubin DT. Successful Treatment of Ulcerative Colitis With Vedolizumab in a Patient With an Infliximab-Associated Psoriasiform Rash. ACG Case Rep J. 2015;2(4):236-8. doi: 10.14309/crj.2015.70. [ Links ]
Received: January 30, 2018; Accepted: March 25, 2018











 text in
text in