Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.1 Bogotá Jan./Mar. 2019
https://doi.org/10.22516/25007440.215
Case report
A Case of Dermatomyositis and Ulcerative Colitis
1Hospital Provincial Docente Manuel Ascunce Domenech. Camagüey, Cuba
Introduction:
The incidence of idiopathic inflammatory myopathy ranges from 4 to 15 cases per million inhabitants while its prevalence is 60 cases per million inhabitants. Given the identification of clinical forms, it is possible that these figures will increase in the coming years. Incidence and prevalence of ulcerative colitis have been increasing, and it now affects 2% of the world population. Symptoms are determined by the extent and severity of lesions. It is chronic with recurring outbreaks, and there is no medical cure. Dermatomyositis in association with ulcerative colitis occurs extremely infrequently.
Objective:
This study presents the case of a patient diagnosed with dermatomyositis associated with ulcerative colitis.
Clinical Case:
The patient was a 70 years white woman, a housewife with no family or epidemiological history of interest. She reported that she had had diarrhea accompanied by abdominal pain, mucus and pus when she was fifty years old. About one year prior to diagnosis, she developed muscle weakness in her shoulders that made it difficult for her to lift her arms. Laboratory, imaging and histopathological tests showed dermatomyositis associated with ulcerative colitis. We point out clinical characteristics, diagnostic means and the therapy used to treat our patient.
Conclusions:
This case of a patient with clinical manifestations of the very infrequent combination of dermatomyositis and ulcerative colitis should be taken into account by doctors who care for these patients because both conditions have immunological bases and can be expressed in various ways.
Keywords: Dermatomyositis; ulcerative colitis
Introducción:
la incidencia de la miopatía inflamatoria idiopática es de 4 a 15 casos por millón de habitantes y su prevalencia es de 60 casos por cada millón de habitantes. Dada la identificación de formas clínicas es posible que estas cifras de incidencia y prevalencia aumenten en los próximos años. La colitis ulcerosa ha ido en aumento afectando al 2 % de la población mundial. Los síntomas están determinados por la extensión y gravedad de las lesiones, teniendo un curso crónico que puede evolucionar por brotes y no existe tratamiento médico curativo. La asociación de la dermatomiositis y la colitis ulcerativa es extremadamente infrecuente.
Caso clínico:
Paciente de 70 años, femenina, blanca, ama de casa, sin antecedentes familiares de interés ni epidemiológicos. Refiere que a los 50 años presentó cuadros diarreicos acompañados de dolor abdominal, moco y pus. Desde hace 1 año aproximadamente ha estado presentando debilidad muscular a nivel de los hombros, lo que le dificultaba levantar los brazos. Se realizaron exámenes de laboratorio, imagenológicos e histopatológicos que mostraron la presencia de una dermatomiositis asociada con colitis ulcerativa. Se señalan las características clínicas, medios diagnósticos y la terapia empleada en nuestra paciente.
Conclusiones:
se presentó el caso de una paciente con manifestaciones clínicas de dermatomiositis y colitis ulcerativa. Esta asociación es muy infrecuente y debe ser tenida en cuenta por los médicos que reciben consultas de estos pacientes, debido a que ambas entidades tienen una base inmunológica y pueden expresarse de variadas formas.
Palabras clave: Dermatomiositis; colitis ulcerosa
Introduction
Polymyositis was described by Wagner in 1882, and in 1887 Ulverricht invented the name dermatomyositis (DM) for the association of muscle pain and weakness with inflammatory skin lesions. Hachulla has noted that the Bohan and Peter diagnostic criteria for DM are useful for differentiating the pathogeneses of these myopathies. 1,2 These criteria include symmetric and progressive loss of proximal muscle strength of the waists with or without dysphagia or compromised respiratory muscles, elevation of musculoskeletal enzymes, muscle biopsy; electromyographic alterations and cutaneous exanthema.
DM most frequently occurs secondary to neoplasms located in the lung and digestive tract but is infrequently associated with ulcerative colitis (UC). This is the first case reported in our hospital in 55 years.
Clinical case
The patient was a white, 70 year old housewife with no family or epidemiological history of interest. She reported that at during her 50s she had had bouts of diarrhea accompanied by abdominal pain, mucus and pus with a frequency of 6 to 8 bowel movements daily and a duration of 5 to 7 days. Her condition had improved with diet. She was seen by doctors several times, but they were unable to make a diagnosis. This condition alternated with periods of clinical improvement for approximately 5 years. For approximately one year she had been suffering from weakness of her shoulders which made it difficult to raise her arms, comb her hair and perform daily household chores. In addition, she had noticed difficulty in getting up from a sitting position and could not climb stairs or swallow solid foods. All of this was associated with skin lesions around the eyes, and on her chest and both hands.
Clinical examination
Wet and colored mucous membranes and heliotrope rashes were found in both periorbital areas (Figure 1).

Figure 1 Heliotrope erythema, violet lesions distributed bilaterally and symmetrically around the eyes and eyelids, accompanied by a certain degree of edema.
Erythema affected several areas of the body but was most accentuated on the upper chest, arms and thighs (Figure 2).
In the physical examination, the patient presented the following characteristics:
Cardiorespiratory system: normal vesicular murmur, rhythmic heart tones, blood pressure: 120/80 mm Hg, heart rate: 80 beats per minute (bpm).
Abdomen: pain on deep palpation of left hemiabdomen but no visceromegaly.
Nervous system: Patient was well oriented in time, space and person. No focal signs
Musculoskeletal system: Patient suffered generalized joint pain especially in both hands and had Gottron’s sign of red-purple keratotic, atrophic erythema on the extensor surface of the backs of her hands and metacarpophalangeal and interphalangeal areas (Figure 3). This was accompanied by progressive myalgia which was most severe in the proximal regions of both arms. Muscular hypotrophy of several muscles was striking, osteotendinous reflexes and muscle strength were diminished in all four limbs.
Defecation was painful and produced stools containing mucous and blood.
Her vagina, the fundus of her uterus, and her breasts were without alterations.
In the analytical study the patient presented the characteristics described below:
Hemoglobin: 11 g/L, leukocytes: 10.3 x 109/L with normal differential, erythrocyte sedimentation rate: 70 mm/first hour. Blood sugar, creatinine, lipids, uric acid, Addis count and veneral disease research laboratory test (VDRL) are normals. Total proteins: albumin: 64,5%, α1:1.3%; α2:2.5%; β:4,4%; G protein: 12,6%. LE cells, IgM rheumatoid factor, antinuclear antibodies, cryoglobulins, complement and antiphospholipid antibodies, negative.
Enzymes: creatine-phosphokinase: 1250 IU, creatine kinase MM: elevated. Aspartate transaminase: 79 IU and alanine transaminase: 63 IU. Lactic dehydrogenase: 580 IU, at the expense of LDH 2 and LDH 3. Thyroid profile: normal. Colon and fecal cultures: negative for bacteria and parasites. Human immunodeficiency virus, hepatitis B antigens, antibodies against hepatitis C, slow serology in search of brucella and blood cultures, negative.
Chest x-ray: normal. X-rays of hands and joints: reduction of metacarpophalangeal and interphalangeal joint spaces with generalized degenerative changes. Abdominal and gynecological ultrasound: thickening of the mucous layer of the left colon, atrophy of internal genitalia. Electrocardiogram: normal. Upper digestive tract endoscopy: esophagus, stomach and duodenum without alterations. Computed tomography (CT) of the thorax, abdomen, retroperitoneum and mediastinum: accentuated degenerative changes of the dorsal and lumbar spine. No mediastinal, retroperitoneal or abdominal alterations. Spirometry: normal. Electroneurophysiology ulnar, middle and tibial posterior: normal. Electromyography of the tibialis anterior and left interosseous: spontaneous fibrillation at rest. Motor unit potential: small amplitude and short duration.
Skin and muscle biopsies (Figures 4 and 5): Perivascular infiltrate of lymphocytes in the deep plexus, predominantly lymphocytic inflammation of perimysial vessels, perifascicular atrophy.
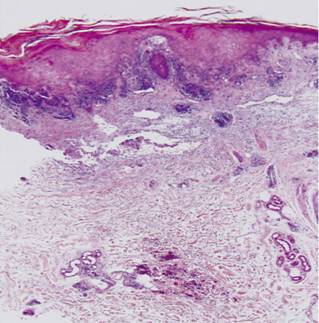
Figure 4 Panoramic histological skin section. Note the perivascular inflammatory infiltrate of the papillary dermis and deep dermis (H/E 20x).
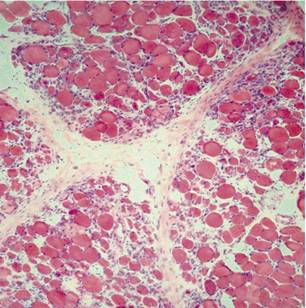
Figure 5 Histological field of the deltoid muscle showing predominantly lymphocytic inflammation of the endomysium and perimysium with necrosis and fiber atrophy (H/E 40x).
A colonoscopy was done because of the possibility that colon cancer was the cause of DM. It showed erythematous, friable mucosa on a granular surface with a normal vascular pattern. A sample was taken for histopathological study which found dispersed diffuse intraepithelial lymphocytes, apoptotic bodies in superficial epithelial cells, Paneth cell metaplasia, ands large numbers of mononuclear cells in the lamina propria. The immunohistochemical study found that more than 25% of the cells were positive for CD8. All these findings are compatible with UC (Figure 6A and B).
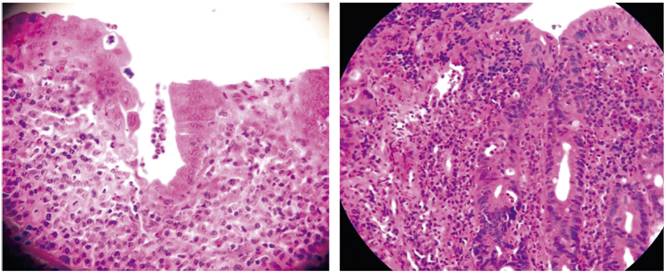
Figure 6 A and B. Histological micrograph of the colon biopsy showing severe chronic inflammation of the entire mucosa in which cryptitis typical of the disease is seen (H/E 40x).
Because it was difficult to reach the left colon to take a biopsy sample, an opaque enema was performed (Figure 7). The findings coincided with those reported by the colonoscopy, ruling out the possibility of a neoplasm.

Figure 7 Barium enema of colon. Note the loss of haustra and stiffening of the wall of the descending and sigmoid colon.
The patient was treated with 1 mg/kg/day of prednisone together with 500 mg of azulfidine every 6 hours for the first weeks followed by tablets every 12 hours after discharge. This treatment was effective, and the patient’s clinical condition improved significantly.
Discussion
The diagnosis of an inflammatory myopathy should be considered when patients present weakness of the upper and lower extremities without sensory symptoms and when rashes characteristic of DM are present. 1,2,3,4 Heliotrope, violet, periorbital rashes with macular edema rashes are pathognomonic. On other occasions, Gottron’s sign appears. This sign consists of violet papules on the backs of the joints of both hands, as observed in this patient. Similarly, the shawl sign may occur. It consists of periungual telangiectasias, capillary thrombosis, poikiloderma, and areas of photosensitivity in exposure zones.
Other symptoms and signs that may occur include interstitial pneumonitis, cardiac involvement and dysphagia, as observed in this patient. Enzymatic alterations characteristic of DM pose differential diagnoses with malignant diseases, hepatopathies and myocardial infarction. DM in association with malignant processes constitutes a paraneoplastic syndrome. Some authors indicate that its incidence is between 13% and 15% while others place it between 20% and 30%. 5,6 The data offered by skin and muscle biopsies show inflammation of the endomysium and perimysium. Perifascicular atrophy can occur, indicating the diagnosis.
UC occurs in most cases between the third and seventh decade of life. 7 This patient was 70 years old. It should be remembered that the cause and the mechanism by which tissue damage occurs is unknown. 8 This patient was diagnosed using the Mendeloff criteria of a history of diarrhea or rectal bleeding for 6 weeks or more, sigmoidoscopy revealing friability of the mucosa with contact bleeding or petechial hemorrhaging with inflammation of the mucosa, barium enema showing evidence of ulceration, narrowing of the colon, and characteristic macroscopic or microscopic alterations. 9 All of these alterations were present in this case.
The appearance of extracolonic complications is well-known with an incidence between 25% and 36%. 10 The most frequently affected organs are the joints, skin, eyes and hepatobiliary system. 7,10,11 As can be seen, involvement of DM with UC occurs very infrequently. No cases were found in our search of the medical literature. Musculoskeletal symptoms are the most frequent symptoms of this disease. 10 They include arthritis similar to rheumatoid arthritis, and ankylosing spondylitis and acute toxic arthritis have both been described. 11 Only generalized arthralgia was reported by this patient.
It is estimated that the risk of colorectal cancer in UC is 4 to 20 times higher than in the general population. 7 Taking this possibility into account, all studies necessary to rule out this disease were performed, and UC was diagnosed by endoscopic, imaging and histological studies.
Steroids are the treatment of choice for DM. 12 Prednisone at a dosage of 1 mg/kg/day after an initial dose of 60 mg is considered to be the most advisable. After 6 to 8 weeks of treatment the dose can be slowly reduced. Treatment should last from 12 to 18 months. For the treatment of UC, first generation aminosalicylates were used. The patient received 500 mg of azepidine in maintenance doses every 6 hours. Following discharge, she continued to take two tablets daily. With this treatment, a notable improvement was achieved both in clinical terms (serum enzyme levels) and in terms of systemic manifestations.
Conclusions
This is a case report of a patient with a previous history of gastrointestinal symptoms who came to our hospital with joint, muscular and dermatological manifestations. Physical examination and complementary examinations confirmed a diagnosis of DM associated with UC although the possibility of colon neoplasia had been suspected initially. This diagnosis must always be considered for timely treatment.
Referencias
1. Hachulla E. Dermatomyositis and polymyositis: clinical aspects and treatment. Ann Med Interne (Paris). 2001;152(7):455-64. [ Links ]
2. Bohan A, Peter JB. Polymyositis and dermatomyositis (first of two parts). N Engl J Med. 1975;292(7):344-7. doi: 10.1056/NEJM197502132920706. [ Links ]
3. García Gutiérrez A, Porro Novo N, Brito E. Colitis ulcerativa idiopática. En: Pardo Gómez G, García Gutiérrez A (editores). Temas de cirugía. La Habana: Ciencias Médicas; 2011. p. 797-817. [ Links ]
4. Miller F. Polimiositis y dermatomiositis. En: Goldman L, Schafer AI (editores). Cecil y Goldman tratado de medicina interna. 24.a edición. Madrid: Elsevier; 2013. p. 1720-5. [ Links ]
5. Miller M, Vleugels R. Clinical manifestations of Dermatomyositis and Polymyositis in adult. UpToDate [internet] 2013 [acceso el 5 de febrero de 2018]. Disponible en: Disponible en: https://www.uptodate.com/contents/clinical-manifestations-of-dermatomyositis-and-polymyositis-in-adults . [ Links ]
6. Zahr ZA, Baer AN. Malignancy in myositis. Curr Rheumatol Rep. 2011;13(3):208-15. doi: 10.1007/s11926-011-0169-7. [ Links ]
7. Hano García O, Andrade Gomes S, Villa Jiménez O, González Fabian L, Wood Rodríguez L. Caracterización de pacientes con colitis ulcerosa atendidos en centro de nivel terciario. Rev Cub Med [internet] 2016 [acceso el 20 de enero de 2018] 55(1). Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75232016000100005&lng=es . [ Links ]
8. Kelly S. Ulcerative colitis. BMJ. 2012;344:e2947. doi: 10.1136/bmj.e2947. [ Links ]
9. Mendeloff AI. Algunas características epidemiológicas de la colitis ulcerativa y enteritis regional. Gastroenterology. 1966;51:742. [ Links ]
10. Blumberg RS. Inflammatory bowel disease: Medical considerations. En: Greenberger NJ, Blumberg RS, Burakoff F (editores). Current diagnosis & treatment. Gastroenterology , hepatology & endoscopy. Boston: Mc Graw-Hill; 2009. p. 22-33. [ Links ]
11. Panés Díaz J. Enfermedad inflamatoria intestinal. En: Rozman C, Cardellach F (editores). Farreras Rozman. Medicina interna. Madrid: Elsevier ; 2016. p. 171-8. [ Links ]
12. Hengstman GJ, van den Hoogen FH, van Engelen BG. Treatment of the inflammatory myopathies: update and practical recommendations. Expert Opin Pharmacother. 2009;10(7):1183-90. doi: 10.1517/14656560902913815. [ Links ]
Received: February 22, 2018; Accepted: April 30, 2018











 text in
text in 




