Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.2 Bogotá Apr./June 2019
https://doi.org/10.22516/25007440.291
Original articles
Differential characteristics of autoimmune hepatitis in Colombian older adults: a cohort study
1Hepatología clínica, Universidad de Antioquia, Medellín, Colombia
2Grupo Gastro-hepatología, Universidad de Antioquia. Unidad de hepatología y trasplante hepático, Hospital Pablo Tobón Uribe. Medellín, Colombia
3Grupo Gastro-hepatología, Universidad de Antioquia. Unidad de epidemiología, Hospital Pablo Tobón Uribe. Medellín, Colombia
Introduction:
Elderly patients with autoimmune hepatitis (AIH) are a special population because of predisposition mediated by the human leukocyte antigen (HLA) system. An indolent and progressive course of the disease has been described. No data are known for the Latin American population.
Objectives:
This study compares clinical presentations, diagnoses, treatments, responses to treatment and course of disease for AIH patients who are over 65 years of age with those of AIH patients who are under 65.
Methods:
This is a retrospective cohort study of patients with HAI evaluated between January 2010 and December 2016. Statistical analyses used SPSS version 20.1.
Results:
Two hundred fourteen patients were included. Elderly patients had hypertension (34.5% vs 15.1%, p = 0.011), dyslipidemia (20.7% vs 5.9%, p = 0.006) and cardiovascular disease (17.2% vs 2.7%, p = 0.001) more frequently than did the younger patients. In addition, the elderly had a higher frequency of cirrhosis confirmed histologically and radiologically (55.1% vs. 33.5%, p = 0.024) at the time of diagnosis. Older patients had a higher rate of biochemical remission resulting from treatment (100% vs 83.9%, p = 0.022). There were no differences in hepatic analyses, autoantibodies, type of pharmacological treatment received, relapses, adverse effects related to treatment, requirements for liver transplantation and deaths.
Conclusion:
AIH affects the Colombian adult population at all ages and should be considered in the diagnostic approach of elderly patients who have liver disease because this group has a higher frequency of cirrhosis at the time of diagnosis. Early diagnosis is important because treatment is effective and well tolerated.
Keywords: Autoimmune hepatitis; Latin America; elderly patients
Introducción:
en la hepatitis autoinmune (HAI), los ancianos representan una población especial debido a que, según se ha descrito, poseen una predisposición mediada por el antígeno leucocitario humano (Human Leukocyte Antigen, HLA) y padecen un curso indolente y progresivo de la enfermedad. No se conocen datos en la población latinoamericana.
Objetivos:
Analizar comparativamente las características de los pacientes con HAI mayores y menores de 65 años en cuanto a su presentación clínica, diagnóstico, tratamiento, respuesta al tratamiento y curso de la enfermedad.
Métodos:
estudio de cohorte retrospectiva de pacientes con HAI evaluados entre enero de 2010 y diciembre de 2016. Se realizó un análisis estadístico utilizando el programa SPSS versión 20.1.
Resultados:
se incluyeron 214 pacientes. Los pacientes ancianos tuvieron, en su mayoría, hipertensión arterial (34,5 % frente a 15,1 %, p = 0,011), dislipidemia (20,7 % frente a 5,9 %, p = 0,006) y enfermedad cardiovascular (17,2 % frente a 2,7 %, p = 0,001). Además, al momento del diagnóstico, los pacientes ancianos tuvieron una mayor frecuencia de cirrosis evaluada histológica y radiológicamente (55,1 % frente a 33,5 %, p = 0,024). Los pacientes mayores tuvieron una mayor remisión bioquímica con el tratamiento (100 % frente a 83,9 %, p = 0,022). No hubo diferencias en la analítica hepática, autoanticuerpos, tipo de tratamiento farmacológico recibido, recaídas, efectos adversos relacionados con el tratamiento, requerimiento de trasplante hepático y muerte.
Conclusión:
La HAI afecta a población colombiana adulta de todas las edades y debe ser considerada en el abordaje diagnóstico de los ancianos con enfermedad hepática, debido a que este grupo de pacientes tiene una mayor frecuencia de cirrosis al momento del diagnóstico. Un diagnóstico temprano es importante debido a que el tratamiento es efectivo y bien tolerado.
Palabras clave: Hepatitis autoinmune; Latinoamérica; ancianos
Introduction
Since its first description in 1950, autoimmune hepatitis (AIH) has been considered to be a disease of young women. 1 Recent subsequent studies have found a bimodal behavior with peaks of occurrence between 10 and 30 years and between 40 and 50 years although it can affect people of all age groups. 2-5 AIH is an important cause of acute liver failure, liver cirrhosis, and morbidity and mortality. It can require liver transplantation and result in post-transplantation liver dysfunction. 6
Older AIH patients are a special population for several reasons. 7 First, studies differ about whether the cut-off age for considering patients as older adults should be 60 or 65 years old. Second, there may be genetic predisposition in this age group due to higher prevalences of HLA-DR4 and HLA-DRB1*04. 5,8 Third, these patients are a diagnostic challenge because the condition is diagnosed later than in the younger population, and because there is a higher frequency of asymptomatic and cirrhotic patients at the time of diagnosis 5,8,9,10 Similar remission rates in response to immunosuppressive treatment have been reported with fewer relapses after treatment ends but with a greater frequency of intolerance and related adverse effects. 5,10,11 The course of AIH in the older population is usually indolent and progressive and can be masked by the presence of other diseases, especially autoimmune diseases. 11
The existing information on the differential behavior of AIH in older adults comes from retrospective studies conducted in the North American 8, European 4,10,12,13,14 and Asian populations as well as from systematic reviews of the literature. 5,15 Prior to this study, there had been no published data on this group of patients in Latin America.
The objective of this study is to compare differences in the clinical and diagnostic characteristics, treatments, and responses to treatments, course of disease, and prognoses of two groups of AIH patients, those younger than 65 years and those older than 65.
Materials and methods
Design and Sample
Sampling for this retrospective study of a historical cohort was based on diagnoses of AIH (International Classification of Diseases 10 code K75.4) in the records of the medical histories of patients treated in the emergency, hospital inpatient, and outpatient services of Hospital Pablo Tobón Uribe (HPTU) in Medellín, Colombia from January 2010 to December 2016. A sample size was not estimated because all patients diagnosed with AIH and treated during the study period were included.
Population
Patients were included if they were 16 years or older and had been diagnosed with AIH according to the simplified diagnostic criteria published in 2008 by the International Autoimmune Hepatitis Group (IAIHG) and had a score of less than six for which the response to drug treatment could help confirm the diagnosis. 2,17
Patients diagnosed before age 16, those with overlap syndromes of AIH with either primary biliary cholangitis (AIH-PBC) or primary sclerosing cholangitis (AIH-PSC), patients with acute liver failure due to AIH and those with drug induced AIH were excluded. Similarly, patients with absence of clinical, biochemical or histological data were excluded if lack of data preventeed adequate diagnosis.
Variables
Data were collected from the diagnosis of AIH to the last clinical follow-up review in the electronic records of the hospital’s medical history and using a previously designed collection form.
Sociodemographic variables collected included age at the time of diagnosis of AIH, sex, and race. Comorbidities including other autoimmune diseases and clinical variables such as the form of presentation were registered. Presentations were classified as follows:
Asymptomatic: those with a biochemical alteration liver without symptoms
Non-specific symptoms: those with biochemical alteration of the liver
Specific symptoms such as asthenia, hyporexia and fever, acute hepatitis
Acute hepatitis: those with abdominal pain, nausea, fever and jaundice associated with transaminases at least 3 times the upper limit of normal but without meeting the criteria of acute liver failure
Liver cirrhosis (those diagnosed by biopsy, clinically or through imagining.
Laboratory variables recorded were measured at the time of diagnosis and during follow-up to evaluate the response to treatment. They included aspartate aminotransferase (AST), alanine aminotransferase (ALT), total bilirubin, alkaline phosphatase, serum albumin, and serum immunoglobulin G (IgG) levels plus prothrombin time and the International Normalized Ratios (INR). In addition, the titers of antinuclear autoantibodies (ANAs), anti-smooth muscle antibodies (ASMAs) and antimitochondrial antibodies (AMAs) were registered.
Histological characteristics were classified according to the recommendations for AIH diagnosis of the IAIHG as either Typical of AIH: interface hepatitis, lymphocytic or plasmocytic infiltrates in portal spaces with extension to the lobule, emperipolesis and formation of rosettes, or Compatible with AIH: chronic hepatitis with lymphocytic infiltrate without the other typical findings of autoimmune hepatitis. 16 The degree of liver fibrosis was evaluated according to the METAVIR scale of grades F0 to F4, where F0 represents the absence of fibrosis and F4 represents advanced fibrosis with cirrhosis.
The induction and maintenance pharmacological treatment scheme used by the hepatology group was evaluated. During the induction phase of the scheme patients receive 0.5-1 mg/kg/day of prednisolone and 1 mg/kg/day of azathioprine. Subsequently, the dose of prednisolone is gradually decreased over three months, and the dose of azathioprine is progressively increased up to 2 mg/kg/day, depending on tolerance and response to treatment during the maintenance phase. The following categories were established for evaluation of treatment response:
Biochemical remission: normalization of transaminases and IgG
Partial clinical improvement and transaminase response but without normalization
Therapeutic failure: failure to achieve at least a 25% decrease of transaminase levels below start of treatment level
Relapse: reelevation of ALT to more than three times the upper limit of normal according to the IAIHG criteria, an increase in IgG levels, or a worsening of histological findings after having achieved remission through drug treatment. 2
Follow-up was carried out until the last clinical evaluation. During this period complications were encountered. They included the development of cirrhosis in patients who had not previously had cirrhosis, requirement of liver transplantation (Our group considers this option in patients 65 and younger and in selected cases over 65.), post-transplant recurrences, liver retransplantation and death.
Ethical Issues
The study is within the parameters of the Helsinki Declaration of 2013 for studies with human beings and within the regulation on clinical research in Colombia (Resolution 008430 of 1993). In addition, it was approved by the HPTU ethics committee. Finally, the final manuscript adhered to the recommendations Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) for reporting observational studies. 18
Statistical Analysis
Statistical analysis was performed with SPSS version 20.1 (SPSS Inc.). Categorical variables are presented as absolute and relative frequencies. Continuous variables are presented as means and standard deviations for normal distributions and as interquartile ranges (IQR) for distributions that are abnormal according to the Kolmogorov-Smirnov test. The differences between groups were established with the χ² test for categorical variables and the Mann-Whitney U test for differences of medians. Values of p were calculated in two tails, where p <0.05 represents a statistical significance.
Results
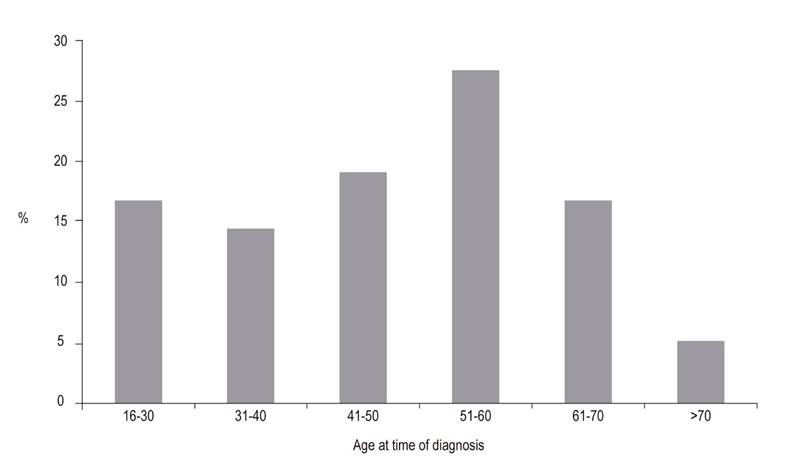
A total of 214 patients met the inclusion criteria. Of these, 185 were diagnosed with AIH before the age of 65, and 29 were diagnosed with AIH at or after the age of 65. Eighty-three patients were excluded for a variety of causes (Figure 1). The age distribution at the time of AIH diagnosis is shown in Figure 2.
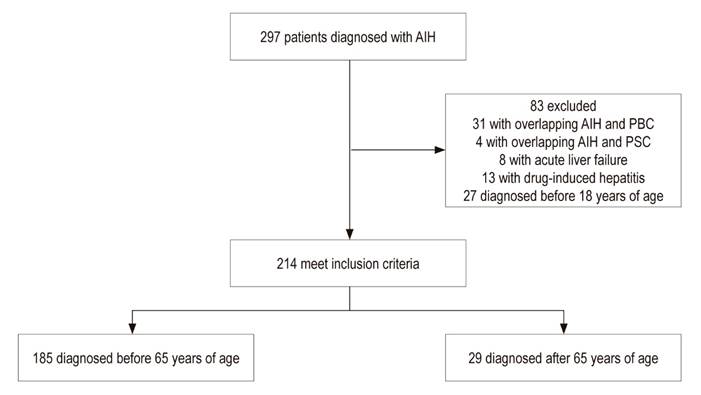
Figure 1 Study flow chart. AIH: autoimmune hepatitis; AIH-PBC: autoimmune hepatitis- primary biliary cholangitis; AIH-PSC: autoimmune hepatitis-primary sclerosing cholangitis.
Most patients in both groups were women. There was a statistically significant difference in the median follow-up time after diagnosis of AIH. It was 50 months for the under-65 group but only 19 for the over-65 group (p <0.001) (Table 1).
Table 1 Demographic, clinical, serological and histological characteristics of patients with AIH according to age.

ALT: alanine aminotransferase; AMA: antimitochondrial antibodies; ANA: antinuclear antibodies; ASMA: anti-smooth muscle antibody; AST: aspartate aminotransferase; AIH: autoimmune hepatitis; IgG: immunoglobulin G; IQR: interquartile range
* Ischemic heart disease, heart failure, peripheral arterial disease, stroke.
¶ Percentage calculated on patients with liver biopsy in each group.
£ According to IAIHG recommendations in Hennes EM et al. Hepatology 2008 Jul; 48 (1): 169-76.
Clinical Issues
In both groups, the most frequent comorbidity was hypothyroidism. There were no differences in other autoimmune diseases. Differences with statistical significance were found for arterial hypertension (15.1% vs. 34.5%, p = 0.011), dyslipidemia (5.9% vs. 20.7%, p = 0.006) and cardiovascular disease (2.7% versus 17.2%, p = 0.001). These comorbidities were frequent in patients diagnosed with AIH at or after 65 years of age. The main form of clinical presentation in both groups was acute hepatitis. Of the patients with acute hepatitis 27.5% were already cirrhotic (acute hepatitis on cirrhotic liver). For under-65 patients this proportion was 26.6% while in the older group it was 33.3%.
In total, 21% of the younger group and 31% of the older group were clinically cirrhotic at the time of diagnosis, but this difference was not significant. Nevertheless, evaluation if the degree of fibrosis by imaging and liver biopsies found a higher frequency of cirrhosis at the time of diagnosis in older patients (33.5% vs. 55.1%, p = 0.024).
Laboratory Findings
There were no differences in the biochemical parameters or autoantibody profiles between the two groups (Table 1). Diagnose of 82% of the patients in both groups were histologically confirmed. More than 95% of cases were either typical of AIH or compatible with AIH, and there were simplified scores of probable or definitive AIH in more than 80% of the patients. There were no significant differences in the distribution of the degree of hepatic fibrosis on the METAVIR scale, but there was a higher frequency of F4 fibrosis in the group of older patients (39.9% versus 58.3%, p = 0.089).
Treatment, Response and Evolution
The combination of a steroid and an immunomodulator was the most frequently administered treatment in both groups. As shown in Table 2, there were no significant differences between the groups. The group of older patients had a higher frequency of biochemical remission with treatment (83.9% versus 100%, p = 0.022) which allowed more frequent suspension of steroid treatment, although this was not statistically significant. Similarly, older patients had a lower, but not statistically significant, frequency of relapses during treatment. In 3.2% of the younger group, immunosuppressive therapy was completely discontinued. In both groups, there were no differences regarding the development of AIH during follow-up among patients who were not cirrhotic at the time of diagnosis. In total, 13 patients underwent transplantation. Of these, only one was from the group of older patients. She was diagnosed with cirrhosis at age 66. Liver transplantation was indicated due to complications related to portal hypertension. There were no differences in requirements of liver transplantation, recurrence of AIH post-transplant, liver retransplantation or mortality.
Table 2 Treatment characteristics, response to treatment and evolution over time.
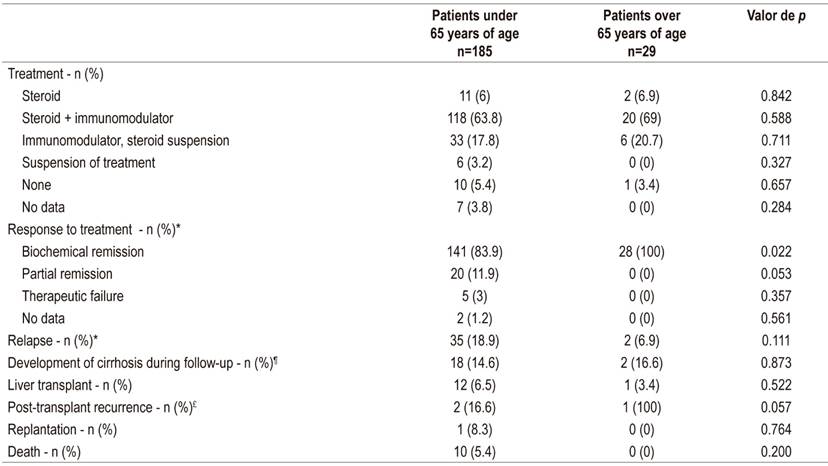
* Percentage calculated on the total of patients who received treatment in each group.
¶ Percentage calculated on the total of non-cirrhotic patients at the time of diagnosis of AIH in each group.
£ Percentage calculated on the total number of patients with liver transplantation in each group.
Discussion
Globally, reports on the differential characteristics of AIH in older patients are scarce, retrospective and heterogeneous. Two different cut-off ages, 60 and 65, have been used to define older patients. The North American, European and Asian patient populations have received the most study, 5 but no data on the Latin American population has been published.
In total, there are 10 studies that evaluate the behavior of AIH in this group of patients. These have recently been analyzed in a systematic review of the literature. 5 Our study is the first that describes the differential behavior of AIH in older Latin American adults who constitute a non-negligible percentage of the total number of patients with AIH: 12.9% (29 of 224) in this study and 10.4 % (29 of 278) of the population of patients with AIH recently published by our group. 19 Both percentages are much lower than those reported globally (24.8%). 5 However, these differences may have several explanations. First, there is the small number of patients reported worldwide: in total 264 older patients with AIH. Second, the heterogeneity of the populations studied, different inclusion criteria, and different cut-off ages. Three studies had a cut-off age of 60 years and seven studies had a cut-off age of 65 years. 5 We used the 65-year-old cut-off age since it was used in most of the reported studies. Third, this definition plus our study’s exclusion of patients under 18 years of age may affect our comparisons. Moreover, we included some patients who had not had liver biopsies (20.9 %), and we used simplified AIH scores of less than six points (17.4%) with the response to treatment confirming the diagnosis of AIH. 2,17 We also excluded patients with AIH-PBC and AIH-PSCE overlap syndromes, medication-induced AIH and acute liver failure due to AIH for which different courses and prognoses have been described. 3,20,21,22
The predominance of women in both age groups and bimodal behavior of AIH in terms of age was corroborated by this study. 2 It should be noted that 22% of the patients were diagnosed after the age of 60 which reinforces the importance of taking into account AIH as a cause of liver disease in this age group. This percentage was similar to that reported in other studies (20%). 4,8,9
Although there were no differences of clinical presentation between the groups, it is important to highlight that almost one fifth of the patients were asymptomatic, since it has been found that up to 26% of patients who do not have symptoms are cirrhotic at moment of diagnosis of AIH. 23 AIH should be considered in differential diagnosis whenever alteration of the biochemical-hepatic profile is found in adults, regardless of the patient’s age. 2,11
A relevant finding of this study is that older adults had a greater degree of liver fibrosis at the time of the diagnosis of AIH than did younger AIH patients, although this difference was not significant in terms of F4 fibrosis found by liver biopsy (58.3% versus 39.9%, p = 0.089). It was significant when cirrhosis was assessed by clinical symptoms of ascites, collateral circulation, encephalopathy, gynecomastia, and telangiectasias combined with analytical tests (hypoalbuminemia, thrombocytopenia, prolonged coagulation times), imaging and biopsies (55.1% versus 33.5%, p = 0.0024). This is consistent with reports from other populations elsewhere in the world. 5 This suggests an indolent course of AIH in older people which could be explained by several reasons. According to Czaja, 7 the subclinical course of the disease can lead to delayed diagnosis and greater prevalence of comorbidities such as arterial hypertension, cardiovascular disease, osteoporosis and neoplasms. 10,11 This suggest an alternative diagnosis that conditions the use of corticosteroids for treating AIH. In addition, there is greater frequency of autoimmune comorbidities in patients with HLA-DRB1*04 which can mask liver manifestations. 8 In this study, there were significant differences found in presence of arterial hypertension, dyslipidemia and cardiovascular disease in the older population which did not impact the type of treatment received for AIH for which no differences were found. No differences were found with respect to autoimmune comorbidities.
Aging involves a series of changes which alter homeostasis of the immune response and which can influence the presentation and course of autoimmune diseases. 24 Classic extrahepatic autoimmune diseases such as systemic lupus erythematosus, rheumatoid arthritis and Sjögren’s syndrome have been studied most. 24 Beyond the immunosenescence process, changes have been found in the architecture of organs involved in the immune response, alterations in the balance between proinflammatory and anti-inflammatory factors, and in the balance between pro-apoptotic and anti-apoptotic factors all of which can modify both humoral and cellular immune responses. 24,26,27 In older people, greater thymic atrophy has been reported with a decrease in the immune response mediated by T lymphocytes without affecting the humoral response. 27,28 This could explain the findings of hyperglobulinemia, better response to immunosuppressive treatment, 11 and lower relapse frequency, 5 the latter two of which were corroborated in this study (100% biochemical remission versus 83.9%, p = 0.022). The indications and treatment scheme recommended for AIH in the older population do not differ from those for the general population. 2 However, treatment may be conditioned by comorbidities and a higher frequency of adverse effects. 7,9 It should be noted that we found no differences in the development of adverse effects related to treatment in our population.
This study has several limitations starting with those inherent in a retrospective study, especially information bias, since the data were collected from the hospital’s electronic medical record base. Second, this is a single-center study. However, this is a national referral center for liver diseases which has the largest number of patients with AIH published in Latin America. 19 Third, some patients were included without liver biopsies who had been diagnosed with a simplified AIH score of less than six. However, these patients responded to pharmacological treatment which helped to corroborate these diagnoses. Fourth, HLA haplotypes were not characterized even though HLA-DQ2 and HLA-DR2 have been demonstrated to be risk factors for AIH in the Latin American population, 29 and even though HLA-DR4 and HLA- DRB1*04 have been demonstrated to be risk factors for older patients. 5,8 Finally, there were differences in patient follow-up times which were shorter for the older group. This limitation has also been found in the most representative studies of AIH in older adults by Al-Chalabi et al. and by Czaja et al. 4,8 In our study, this is explained by growing awareness in recent years of the need to search for AIH in older patients: 72.4% of these patients were diagnosed between 2013 and 2016.
Strengths of this study include the fact that it is one of the largest studies of the behavior of AIH in this group of patients. 5 Other strengths include follow-up in times which allowed study of the differences in AIH behavior by age group; the percentage of patients (82%) with diagnoses confirmed with liver biopsy; the detailed descriptions of clinical presentation forms, and the evaluations of responses to treatment since these issues were not evaluated in some of the studies on AIH in older adults. 5
In conclusion, AIH affects adults of all ages, but it is common in those over 65 years of age who have a higher frequency of cirrhosis at the time of diagnosis. By including AIH in the differential diagnosis of liver disease in this group of patients, timely diagnoses and treatment to which patients respond better with less adverse effects can be achieved.
REFERENCES
1. Waldeström J. Leber, Blut proteine und Nahrungseiweiss. DischZ Verdan Stoff’Wechselkr. 1950;15:113-6. [ Links ]
2. European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Autoimmune hepatitis. J Hepatol. 2015 Oct;63(4):971-1004. https://doi.org/10.1016/j.jhep.2015.06.030. Epub 2015 Sep 1. Erratum in: J Hepatol. 2015 Dec;63(6):1543-4. [ Links ]
3. Mieli-Vergani G, Vergani D. Autoimmune paediatric liver disease. World J Gastroenterol. 2008 Jun 7;14(21):3360-7. https://doi.org/10.3748/wjg.14.3360 [ Links ]
4. Al-Chalabi T, Boccato S, Portmann BC, McFarlane IG, Heneghan MA. Autoimmune hepatitis (AIH) in the elderly: a systematic retrospective analysis of a large group of consecutive patients with definite AIH followed at a tertiary referral centre. J Hepatol. 2006 Oct;45(4):575-83. https://doi.org/10.1016/j.jhep.2006.04.007 [ Links ]
5. Chen J, Eslick GD, Weltman M. Systematic review with meta-analysis: clinical manifestations and management of autoimmune hepatitis in the elderly. Aliment Pharmacol Ther. 2014 Jan;39(2):117-24. https://doi.org/10.1111/apt.12563 [ Links ]
6. Mieli-Vergani G, Vergani D, Czaja AJ, Manns MP, Krawitt EL, Vierling JM, et al. Autoimmune hepatitis. Nat Rev Dis Primers. 2018 Apr 12;4:18017. https://doi.org/10.1038/nrdp.2018.17 [ Links ]
7. Czaja AJ. Special clinical challenges in autoimmune hepatitis: the elderly, males, pregnancy, mild disease, fulminant onset, and nonwhite patients. Semin Liver Dis. 2009 Aug;29(3):315-30. https://doi.org/10.1055/s-0029-1233530 [ Links ]
8. Czaja AJ, Carpenter HA. Distinctive clinical phenotype and treatment outcome of type 1 autoimmune hepatitis in the elderly. Hepatology. 2006 Mar;43(3):532-8. https://doi.org/10.1002/hep.21074 [ Links ]
9. Schramm C, Kanzler S, zum Büschenfelde KH, Galle PR, Lohse AW. Autoimmune hepatitis in the elderly. Am J Gastroenterol. 2001 May;96(5):1587-91. https://doi.org/10.1016/S0002-9270(01)02345-0 [ Links ]
10. Granito A, Muratori L, Pappas G, Muratori P, Ferri S, Cassani F, et al. Clinical features of type 1 autoimmune hepatitis in elderly Italian patients. Aliment Pharmacol Ther. 2005 May 15;21(10):1273-7. https://doi.org/10.1111/j.1365-2036.2005.02488.x [ Links ]
11. Czaja AJ. Clinical features, differential diagnosis and treatment of autoimmune hepatitis in the elderly. Drugs Aging. 2008;25(3):219-39. https://doi.org/10.2165/00002512-200825030-00005 [ Links ]
12. Verslype C, George C, Buchel E, Nevens F, van Steenbergen W, Fevery J. Diagnosis and treatment of autoimmune hepatitis at age 65 and older. Aliment Pharmacol Ther. 2005 Mar 15;21(6):695-9. https://doi.org/10.1111/j.1365-2036.2005.02403.x [ Links ]
13. Parker DR, Kingham JG. Type I autoimmune hepatitis is primarily a disease of later life. QJM. 1997 Apr;90(4):289-96. https://doi.org/10.1093/qjmed/90.4.289 [ Links ]
14. Newton JL, Burt AD, Park JB, Mathew J, Bassendine MF, James OF. Autoimmune hepatitis in older patients. Age Ageing. 1997 Nov;26(6):441-4. https://doi.org/10.1093/ageing/26.6.441 [ Links ]
15. Miyake Y, Iwasaki Y, Takaki A, Kobashi H, Sakaguchi K, Shiratori Y. Clinical features of Japanese elderly patients with type 1 autoimmune hepatitis. Intern Med. 2007;46(24):1945-9. https://doi.org/10.2169/internalmedicine.46.0420 [ Links ]
16. Hennes EM, Zeniya M, Czaja AJ, Parés A, Dalekos GN, Krawitt EL, et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008 Jul;48(1):169-76. https://doi.org/10.1002/hep.22322 [ Links ]
17. Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999 Nov;31(5):929-38. https://doi.org/10.1016/S0168-8278(99)80297-9 [ Links ]
18. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007 Oct 16;147(8):W163-94. https://doi.org/10.7326/0003-4819-147-8-200710160-00010-w1 [ Links ]
19. Díaz-Ramírez GS, Marín-Zuluaga JI, Donado-Gómez JH, Muñoz-Maya O, Santos-Sánchez Ó, Restrepo-Gutiérrez JC. Characterization of patients with autoimmune hepatitis at an university hospital in Medellín-Colombia: cohort study. Gastroenterol Hepatol. 2018 Feb;41(2):87-96. https://doi.org/10.1016/j.gastrohep.2017.09.003 [ Links ]
20. Czaja AJ. Diagnosis and management of the overlap syndromes of autoimmune hepatitis. Can J Gastroenterol. 2013 Jul;27(7):417-23. https://doi.org/10.1155/2013/198070 [ Links ]
21. Björnsson E, Talwalkar J, Treeprasertsuk S, Kamath PS, Takahashi N, Sanderson S, et al. Drug-induced autoimmune hepatitis: clinical characteristics and prognosis. Hepatology. 2010 Jun;51(6):2040-8. https://doi.org/10.1002/hep.23588 [ Links ]
22. Kessler WR, Cummings OW, Eckert G, Chalasani N, Lumeng L, Kwo PY. Fulminant hepatic failure as the initial presentation of acute autoimmune hepatitis. Clin Gastroenterol Hepatol. 2004 Jul;2(7):625-31. https://doi.org/10.1016/S1542-3565(04)00246-0 [ Links ]
23. Feld JJ, Dinh H, Arenovich T, Marcus VA, Wanless IR, Heathcote EJ. Autoimmune hepatitis: effect of symptoms and cirrhosis on natural history and outcome. Hepatology. 2005 Jul;42(1):53-62. https://doi.org/10.1002/hep.20732 [ Links ]
24. Watad A, Bragazzi NL, Adawi M, Amital H, Toubi E, Porat BS, et al. Autoimmunity in the Elderly: Insights from Basic Science and Clinics - A Mini-Review. Gerontology. 2017;63(6):515-523. https://doi.org/10.1159/000478012 [ Links ]
25. Amador-Patarroyo MJ, Rodriguez-Rodriguez A, Montoya-Ortiz G. How does age at onset influence the outcome of autoimmune diseases? Autoimmune Dis. 2012;2012:251730. https://doi.org/10.1155/2012/251730 [ Links ]
26. Schwab R, Russo C, Weksler ME. Altered major histocompatibility complex-restricted antigen recognition by T cells from elderly humans. Eur J Immunol. 1992 Nov;22(11):2989-93. https://doi.org/10.1002/eji.1830221134 [ Links ]
27. De Paoli P, Battistin S, Santini GF. Age-related changes in human lymphocyte subsets: progressive reduction of the CD4 CD45R (suppressor inducer) population. Clin Immunol Immunopathol. 1988 Sep;48(3):290-6. https://doi.org/10.1016/0090-1229(88)90022-0 [ Links ]
28. Ben-Yehuda A, Weksler ME. Immune senescence: mechanisms and clinical implications. Cancer Invest. 1992;10(6):525-31. https://doi.org/10.3109/07357909209024815 [ Links ]
29. Duarte-Rey C, Pardo AL, Rodríguez-Velosa Y, Mantilla RD, Anaya JM, Rojas-Villarraga A. HLA class II association with autoimmune hepatitis in Latin America: a meta-analysis. Autoimmun Rev. 2009 Feb;8(4):325-31. https://doi.org/10.1016/j.autrev.2008.11.005 [ Links ]
Received: August 27, 2018; Accepted: March 12, 2019











 text in
text in