Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.2 Bogotá Apr./June 2019
https://doi.org/10.22516/25007440.224
Case report
Perforation of the jejunum due to diverticular disease: A condition to consider in the elderly
1Medicina Interna, Universidad Libre. Cali, Colombia. Grupo Interinstitucional de Medicina Interna (GIMI 1). ORCID 0000-0001-9083-4460. Cali, Colombia
2Psiquiatra, Universidad Libre. Cali, Colombia
3Profesor Asociado, Departamento de Medicina Interna, Universidad Libre, GIMI 1. Profesor Asociado, Departamento de Medicina Familiar, Universidad del Valle. ORCID 0000-0001-6084-4764. Cali, Colombia
4Coordinadora Médica de Cirugía, Clínica Farallones. Directora Médica Regional Hospitalaria, Christus Sinergia Salud. ORCID 0000-0002-2356-1383. Cali, Colombia
Diverticular disease is the most common bowel disease after the age of 40 years. It is the most common finding in elective endoscopic procedures, and it has great relevance because of its broad manifestations which lead to frequent emergency service consultations. On the other hand, the prevalence of diverticulosis of the small intestine ranges from 2% to 5%. Clinical presentations such as bleeding, obstructions, abdominal pain, perforations, formation of abscesses and fistulas are usually more florid when they affect the colon. We present the case of an elderly emergency room patient with acute abdomen secondary to generalized peritonitis due to intestinal perforation caused by diverticular disease of the jejunum.
Keywords: Elderly patients; geriatrics; intestine; diseases of the jejunum; diverticulum; delirium
La enfermedad diverticular constituye la principal afección intestinal después de los 40 años; tiene gran relevancia por sus amplias manifestaciones, que llevan a consultas frecuentes en todos los servicios de urgencias y corresponden al hallazgo más usual en los procedimientos endoscópicos electivos. Por su parte, la diverticulosis del intestino delgado tiene una prevalencia que oscila entre 2 % y 5 %. Las presentaciones clínicas como sangrado, obstrucción, dolor abdominal, perforación, formación de abscesos y fístulas suelen ser más floridas cuando afectan el colon. Se presenta el caso de un paciente anciano quien consultó a urgencias con abdomen agudo secundario a peritonitis generalizada por perforación intestinal debida a enfermedad diverticular del yeyuno.
Palabras clave: Anciano; geriatría; intestino; enfermedades del yeyuno; divertículo; delirio
Introduction
Diverticula are saclike formations produced by protrusions of mucosa through the muscular wall of the intestine. Their prevalence is similar in men and women, 1 but it increases with age from less than 20% at 40 years to more than 63% in people over 70 years of age. 2 Diverticular disease mainly affects the colon, especially the sigmoid colon. 2 Diverticula are less common in the small intestine, but 80% of diverticulosis of the small intestine occurs in the jejunum, 15% occurs in the ileum and 5% affects both. 3 A series of autopsies has reported that between 1% and 4.5% of bodies examined had diverticular in the jejunum and ileum. 4,5
The etiology of jejunal diverticula is not clear, but motility alterations have been considered, 6 and some nutritional risk factors such as low-fiber diets and diets rich in refined sugars increase formation of diverticula in general. 7 Low fiber intake results in poorly hydrated feces which can alter intestinal transit time which translates into increased colonic pressure. This makes it difficult to evacuate intestinal contents and promotes the formation of diverticula. 7 Other risk factors that may increase frequency of occurrence include changes in microbiota, constipation, sedentary lifestyles, obesity, smoking and consumption of non-steroidal anti-inflammatory drugs (NSAIDs). 2
Up to 75% of cases of diverticular disease are asymptomatic. The most frequent symptoms are abdominal pain, 8 lower gastrointestinal bleeding, inflammation, abscess formation, perforations, and obstructions. 5 Diagnosis in the small intestine the can be difficult because there are no pathognomonic characteristics or specific symptoms. 9
Consequently, it is vitally important to know the forms of presentation of atypical diverticular disease in elderly patients because the timely diagnosis will have an impact on the patient’s survival.
Case description
The patient was a 67-year-old man who came to the clinic following two days of stabbing abdominal pain of moderate intensity located in the hypogastrium. Onset was gradual, then pain radiated to the mesogastrium and the right iliac fossa. It was accompanied by abdominal distension, postprandial emesis, two episodes of diarrhea without mucus or blood, and unquantified fever. Patient had experienced fluctuation of consciousness, disorientation and zoomorphic visual hallucinations.
The only comorbid history was chronic arterial hypertension which had been controlled with an angiotensin-converting enzyme inhibitor (ACEI). He had no history of surgery, cognitive compromise, or mental illness and had been functional condition and able to perform basic activities of daily life prior to admitting himself to the hospital (Barthel scale: 100/100).
Physical and mental examination at admission showed the patient to be lethargic, and temporospatially disoriented with a fluctuating state of consciousness. He was unable to maintain fluent conversation and had irrelevant thinking and incoherent language. The patient’s temperature was 38.8° C, he had tachycardia with a heart rate of 120 beats per minute, his respiratory rate was 24 breaths per minute, and he was hypotensive with blood pressure of 90/50 mm Hg) and capillary filling of 4 seconds. His abdomen was markedly distended without peristalsis, with pain on superficial palpation on the flank and right iliac fossa. He exhibited central tympanism and voluntary abdominal defense.
The initial clinical diagnostic impression was sepsis of abdominal origin secondary to acute appendicitis accompanied by hypoactive delirium. This was based on a quick Sequential Organ Failure Assessment (qSOFA) score of three points plus the obvious psychiatric manifestations at the time which were correlated with a Short Confusion Assessment Method (Short-CAM) evaluation of acute onset and fluctuating course of mental state.
Intravenous fluids were administered and hemodynamic normality was achieved. Ampicillin and sulbactam were also administered and paraclinical studies were requested that. They showed a leukocyte count of 15,530/μL, a hemoglobin count of 10.4 g/dL, a platelet count of 130,000/μL, a C-reactive protein (CRP) level of 114 mg/dL, arterial gases with pH of 7.31, partial carbon dioxide pressure (pCO2) of 22.7 mm Hg, partial oxygen pressure (PO2) of 70.3 mm Hg, a bicarbonate (HCO3) level of 11.2 mmol/L and base excess (BE) of -12.7 mmol/L. Standing chest x-rays (Figure 1) and simple abdominal x-rays (Figure 2) were taken.
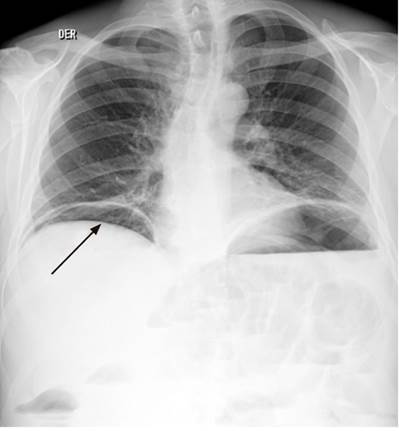
Figure 1 Posteroanterior standing chest x-ray shows bilateral pneumoperitoneum (arrow) with a bilateral basal subpulmonary collection of liquid on the left accompanied by the elevation of both hemidiaphragms and bilateral biliary reticular interstitial opacities without pleural effusion.

Figure 2 Simple x-ray showing multiple accumulations of gas and liquids (arrow) that compromise the entire abdominal cavity, especially in the mesogastrium and epigastrium, with air in the rectal ampulla (partial obstruction or ileus).
With these findings, an emergency exploratory laparotomy was performed. It found four quadrant peritonitis, a 10 cm segment of the jejunum with a congestive, edematous appearance, and areas of necrosis which were resected. End-to-end anastomosis was performed and washed with warm saline solution. The study of the surgical specimen identified diverticular formations with an inflammatory reaction (Figures 3 and 4).
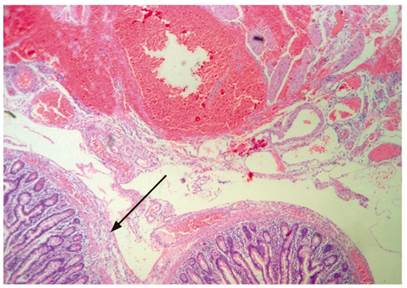
Figure 3 Segment of the jejunum in which edema and inflammation are most evident and appear together (arrow) with diverticular formations (hematoxylin-eosin 50 X).
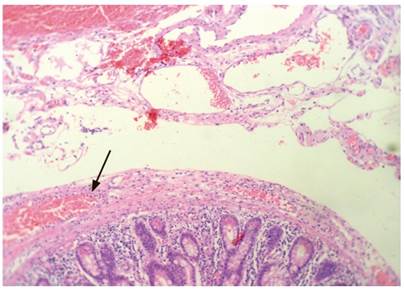
Figure 4 Segment of the small intestine in which there is edema of the wall with inflammatory infiltrate moving from the mucosa into the serosa. Bleeding can be seen beyond the serosa (arrow), but which does not adhere to it. It is probably related to bleeding in the peritoneum (hematoxylin-eosin 100 X).
The abdomen was initially operated on with the negative pressure system. Surgical washes were performed every 48 hours until the abdominal wall was closed on day 10. The patient was managed in the intensive care unit (ICU) for 6 days, then continued his favorable evolution in the general ward with resolution of abdominal sepsis, improvement of his clinical and mental condition, and recovery of functionality. He was discharged on day 14.
Discussion
Acute abdominal pain, especially in the elderly population, is a frequent reason for consultation in the emergency department. A large percentage of these cases require hospital admission and/or surgical management. 11 This increases the cost of the health care system, especially when rapid diagnosis and timely intervention is not possible.
We present the case of an older adult described above who consulted for acute abdominal pain associated with psychiatric manifestations compatible with delirium. Clinically, we found data on systemic inflammatory response syndrome (SIRS) with a qSOFA score over two. 10 Paraclinical studies reported high levels of inflammatory reactants, the CBC had a left shift, and the patient had metabolic acidosis all of which supported the diagnosis of sepsis and merited a goal-guided intervention. 10 Images showed the rupture of a hollow viscera and signs of partial intestinal obstruction. 12 Due to the anatomical location of the pain, appendicular pathology was suspected, but the possibility of spontaneous perforation of the small intestine was not ruled out. The causes of spontaneous perforation of the small intestine appear in Table 1.
Table 1 Causes of spontaneous perforation of the small intestine (13)
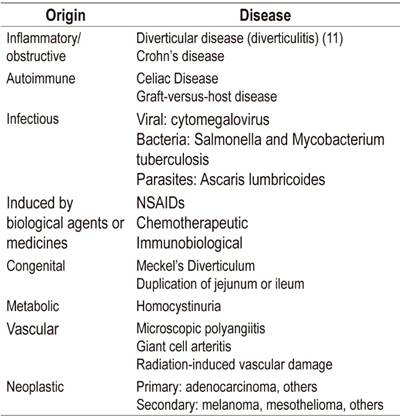
Adapted from Freeman HJ. World J Gastroenterol. 2014; 20 (29): 9990-7
However, there is another way to approach acute abdominal pain in elderly patients based on probable etiological cause in obstructive, inflammatory, vascular or cryptogenic causes. 14 Age and case presentation were in favor of an inflammatory rather than a vascular condition. 15 Finally, pathology identified severe jejunal diverticular disease with signs of perforation (Figures 3 and 4).
Diverticular disease of the small intestine does not have well-established etiology, so multiple hypotheses have been posited. It was first described in 1794 by Sommering and confirmed almost 15 years later by Sir Astley Cooper. 16 It is most prevalent between 47 and 86 years of age with an average age of 72. 17 Its presentation is not specific but ranges from diffuse abdominal pain to lethal complications of all kinds, especially in the elderly among whom atypical onset such as delirium can occur. 18 Nevertheless, it is asymptomatic in 90% of cases when the duodenum is affected and in 40% of cases that affect the jejunum. In this last group it becomes symptomatic in 40% of cases. In these cases, its primary manifestation is intestinal malabsorption syndrome. 19
Among its most frequent complications, the greatest risks come from intestinal obstruction and digestive bleeding which can result in formation of abscesses and, in rare cases, in fistulas and spontaneous perforation as a manifestation of acute abdomen, as in this case. 20 For this reason, it is important to expand differential diagnosis and remember that diverticula of the small intestine are always present.
Finally, the interesting thing to remember is that there are causes of acute abdomen that are not usually taken into account in assessment of geriatric patients. This is especially true when the onset of the condition is delirium, which has a potentially lethal organic cause.
REFERENCES
1. Young-Fadok TM, Roberts PL, Spencer MP, Wolff BG. Colonic diverticular disease. Curr Probl Surg. 2000;37(7):457-514. [ Links ]
2. Fluxá D, Quera R. Enfermedad diverticular: mitos y realidades. Rev Med Chile. 2017;145(2):209-18. https://doi.org/10.4067/S0034-98872017000200009 [ Links ]
3. Grande G, Zulli C, Bertani H, Mirante VG, Caruso A, Conigliaro R. Endoscopic Treatment of Stent-Related Esophagobronchial Fistula. ACG Case Rep J. 2016;3(4):e185. https://doi.org/10.14309/crj.2016.158 [ Links ]
4. Grubbs J, Huerta S. Perforated jejunal diverticulitis in a nonagenarian veteran: A case report. Int J Surg Case Rep. 2017;40:77-9. https://doi.org/10.1016/j.ijscr.2017.09.011 [ Links ]
5. Hevia M, Quera R, Soto L, Regueira T, O’Brien A, Larach A, et al. Diverticulitis aguda de intestino delgado en un paciente con enfermedad de Crohn. Rev Med Chile. 2017;145(3):397-401. https://doi.org/10.4067/S0034-98872017000300016 [ Links ]
6. Zager JS, Garbus JE, Shaw JP, Cohen MG, Garber SM. Jejunal diverticulosis: a rare entity with multiple presentations, a series of cases. Dig Surg. 2000;17(6):643-5. https://doi.org/10.1159/000051978 [ Links ]
7. Dahl C, Crichton M, Jenkins J, Nucera R, Mahoney S, Marx W, et al. Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review. Nutrients. 2018;10(2). pii: E137. https://doi.org/10.3390/nu10020137 [ Links ]
8. López AJ, Ramia JM, De la Plaza R, Alonso S, González JD, Kühnhardt AW. Enfermedad diverticular yeyuno-ileal complicada tratada quirúrgicamente: serie de 12 casos y revisión de literatura. Rev Gastroenterol Peru. 2017;37(3):240-5. [ Links ]
9. Karas L, Asif M, Chun V, Khan FA. Complicated small bowel diverticular disease: a case series. BMJ Case Rep. 2017;2017. pii: bcr-2017-219699. https://doi.org/10.1136/bcr-2017-219699 [ Links ]
10. Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):762-74. https://doi.org/10.1001/jama.2016.0288 [ Links ]
11. Bejarano M, Gallego CX, Gómez JR. Frecuencia de abdomen agudo quirúrgico en pacientes que consultan al servicio de urgencia. Rev Colomb Cir. 2011;26(1):33-41. [ Links ]
12. Jarral OA, Purkayastha S, Darzi A, Zacharakis E. Education and Imaging. Gastrointestinal: Enterolith-induced perforation on a background of jejunal diverticulum. J Gastroenterol Hepatol. 2010;25(2):429. https://doi.org/10.1111/j.1440-1746.2010.06261.x [ Links ]
13. Freeman HJ. Spontaneous free perforation of the small intestine in adults. World J Gastroenterol. 2014;20(29):9990-7. https://doi.org/10.3748/wjg.v20.i29.9990 [ Links ]
14. Ocampo Chaparro JM, González Hadad A. Acute abdomen in the elderly. Rev Colomb Cir. 2006;21(4):266-82. [ Links ]
15. Ocampo JM, Reyes-Ortiz CA, Rengifo A, Velasco MM. Isquemia mesentérica crónica en ancianos: un reto diagnóstico. Rev Colomb Cir. 2017;32:229-35. [ Links ]
16. Kavanagh C, Kaoutzanis C, Spoor K, Friedman PF. Perforated jejunal diverticulum: a rare presentation of acute abdomen. BMJ Case Rep. 2014;2014. pii: bcr-2013-202673. https://doi.org/10.1136/bcr-2013-202673 [ Links ]
17. Johnson KN, Fankhauser GT, Chapital AB, Merritt MV, Johnson DJ. Emergency management of complicated jejunal diverticulosis. Am Surg. 2014;80(6):600-3. [ Links ]
18. Ocampo JM, Osorno DA. Delirium: un gigante de la geriatría. Manizales: Universidad de Caldas; 2009. [ Links ]
19. Peery AF, Barrett PR, Park D, Rogers AJ, Galanko JA, Martin CF, et al. A high-fiber diet does not protect against asymptomatic diverticulosis. Gastroenterology. 2012;142(2):266-72.e1. https://doi.org/10.1053/j.gastro.2011.10.035 [ Links ]
20. Durgakeri P, Sarkar A. Perforated jejunal diverticulum: a case report. ANZ J Surg. 2017;87(7-8):634-5. https://doi.org/10.1111/ans.12954 [ Links ]
Received: March 13, 2018; Accepted: April 23, 2018











 text in
text in 


