Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.2 Bogotá Apr./June 2019
https://doi.org/10.22516/25007440.399
Case report
Laparoscopic-assisted transgastric retrograde endoscopic cholangiopancreatography in a patient with a Roux-en-Y gastric bypass: Case report and literature review
1 Programa de Especialización en Gastroenterología y Endoscopia Digestiva, Fundación Universitaria de Ciencias de la Salud, Sociedad de Cirugía de Bogotá. Servicio de gastroenterología y endoscopia digestiva, Hospital de San José. Bogotá D. C., Colombia
2 Programa de Especialización en Cirugía General, Fundación Universitaria de Ciencias de la Salud, Sociedad de Cirugía de Bogotá. Servicio de cirugía general, Hospital de San José. Bogotá D. C., Colombia
Obesity is a public health problem. Bariatric surgery plays an important role in the management of these patients. With the advent of bariatric surgical techniques, endoscopic digestive procedures, especially endoscopic retrograde cholangiopancreatography (ERCP), have become constant challenges. We describe a case of laparoscopic-assisted transgastric retrograde endoscopic cholangiopancreatography (ERCP) to treat calculi in the main bile duct of a patient with a history of a Roux-en-Y gastric bypass.
Keywords: Roux-en-Y gastric bypass; endoscopic retrograde endoscopic cholangiopancreatography (ERCP); laparoscopy
La obesidad es un problema de salud pública. La cirugía bariátrica juega un papel importante en el manejo de estos pacientes. Con la llegada de estas técnicas quirúrgicas, los procedimientos endoscópicos digestivos y en especial la colangiopancreatografía retrógrada endoscópica (CPRE) se convierten en un desafío constante. Se describe un caso de CPRE transgástrica asistida por laparoscopia para el manejo de cálculos de la vía biliar principal en un paciente con antecedente de derivación gástrica en Y de Roux (BPGYR).
Palabras clave: Derivación gástrica en Y de Roux; colangiopancreatografía retrógrada endoscópica (CPRE) transgástrica; laparoscopia
Introduction
Obesity is a disease whose incidence has reached global epidemic proportions. It affects approximately 600 million people according to data reported by the World Health Organization (WHO). 1
According to data from ASIS (Análisis de Situación de Salud - health situation analysis) of 2016; the prevalence of obesity in Colombia in 2010 was 20% higher than prevalence in 2005, having increased from 13 to 16 cases per 100 people. 2
Although surgery is currently throughout the world as an effective option for long-term obesity control, these surgical techniques have made digestive endoscopic procedures constant challenges due to complications inherent in bariatric surgery. 3,4
Other Latin American experiences of laparoscopic retrograde endoscopic retrograde cholangiopancreatography (ERCP) have already been published, 5,6 so the objective of this paper is to discuss the approach using this technique for managing bile duct stones in a patient with a history of Roux-en-Y gastric bypass (RYGB) surgery.
Clinical case
The patient was a 70-year-old woman who had undergone a gastric bypass in 2008 and laparoscopic cholecystectomy in 2013. She came to the hospital after having suffered abdominal pain for one year. After magnetic resonance cholangiopancreatography (MRC) identified a 5 mm calculus at the distal end of the bile duct. The patient was hospitalized. Because of her history of RYGB which alters the anatomy and affects the usual endoscopic approach to the pathway bile, she was scheduled for laparoscopic-assisted transgastric endoscopic retrograde cholangiopancreatography (LAERCP).
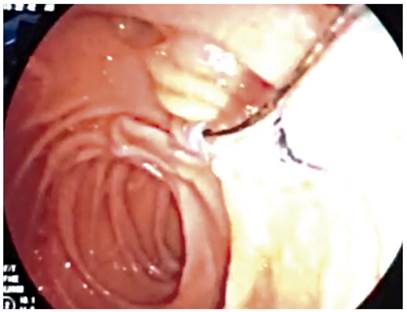
Prior to laparoscopy to allow the duodenoscope to enter the stomach, the second duodenal portion where the major papilla is usually located was found (Figure 1). The extrahepatic and intrahepatic bile ducts were dilated and a calculus was found inside. The ducts were canalized and electrosurgical biliary sphincterotomy was performed. The bile duct was explored with a basket, and the calculus was extracted without complications.
As of March 2018, the patient continued to be free of all digestive symptoms.
Discussion
Rapid weight loss in patients who undergo RYGB is considered a risk factor for gallstone formation, 3 postoperative weight loss of more than 25% of original weight reportedly is associated with the formation of symptomatic gallstones, 7 and about 35% of patients develop biliary lithiasis in the first 12 months after bariatric surgery. 8
Under normal conditions, ERCP is performed with a side-viewing duodenoscope inserted through the mouth and into the second portion of the duodenum to canalize the papilla. This successful technique combines endoscopy with radiological imaging. However, even in expert hands complications including bleeding, perforations, cholangitis and pancreatitis can occur. 9 For this reason, ERCP is considered an advanced endoscopy technique that requires special training. 10,11
The difficulties and complications inherent to ERCP increase when performed in altered anatomy. When ERCP is performed in patients with altered anatomy, important challenges determine the procedure’s success rate. These include ability to intubate the duodenum, ability to face the major papilla, ability to enter and canalize the major papilla, therapeutic success, total time of intervention, and complications inherent to the procedure. Due to these difficulties, ERCP should be performed at referral centers for advanced endoscopy with the support of a multidisciplinary team of gastroenterologists, radiologists, surgeons and anesthesiologists who can facilitate success and mitigate the number of complications. 8
There is no protocol on how to perform ERCP in post-bariatric surgery patients, and different types of endoscopes and endoscopic techniques can be used depending on availability and local experience. 11 Nevertheless, recommendations for performing ERCP in patients who have altered anatomy have recently been published. 12 For patients with Billroth II anatomy, biliary access is similar with front and side view endoscopes, but the latter are associated with increased risks of perforation. 12 In these cases, the major papilla can be reached since the afferent loop is relatively short, but the main challenges of duodenal intubation and entry into the bile duct remain. A series of 713 patients has demonstrated a success rate for duodenal intubation of 86% and a success rate for bile duct canalization of 94%. The overall perforation rate was 1.8%. 13
ERCP assisted by single or double balloon enteroscopy is one of the recommended options for patients who have undergone RYGB. The ERCP technique assisted by double balloon enteroscopy consists in advancing through the small intestine by inflating and deflating balloons until the major papilla is reached allowing canalization of the bile duct. A multicenter study of 159 ERCPs performed in 129 patients who had undergone RYGB found 69% duodenal access with double balloon enteroscopy and 72% with simple enteroscopy. The ERCP success rate was 88%. 14
A recently published metaanalysis covering 15 clinical trials with 461 patients has evaluated diagnostic and therapeutic success of ERCP assisted by simple enteroscopy in patients who had undergone RYGB, hepaticojejunostomy or the Whipple procedure. In general, the success rate for ERCP by simple enteroscopy was 81% with an adverse event rate of 6.5%. 15
Since oral access is difficult in patients who have undergone gastric bypasses and ERCP assisted by enteroscopy has disadvantages such as long duration of the procedure, difficulty orienting endoscopy equipment, less maneuverability of equipment, and availability of reliable and useful accessories for increasing the diagnostic and therapeutic performance of the procedure, an alternative method has been devised. This consists of reaching the major papilla through the stomach with laparoscopic assistance. Transgastric ERCP assisted by laparoscopy, originally described by Baron, 3 has been shown to be superior to ERCP assisted by enteroscopy in terms of duodenal intubation, identification of the major papilla, bile duct canalization rates, therapeutic success and total time of procedure. No statistically significant differences were found in relation to hospitalization stays and complication rates. 16,17
Recently, Snauwaert has published a retrospective, multicenter observational study of a cohort of patients with histories of RYGB who also presented complicated biliary pathologies including cholangitis, choledocholithiasis and biliary pancreatitis. The patients had all undergone laparoscopic-assisted transgastric ERCP between 2008 and 2014. A total of 23 patients had undergone the procedure, with a bile duct canalization success rate of 100%; without complications (bleeding, pancreatitis or perforation) and with an average hospital stay of 2.8 days (range: 2-4). 18
In recent years, another endoscopic technique has also been used to perform ERCP in patients who had undergone RYGB. This technique uses endoscopic ultrasonography (EUS) to gain access to the excluded stomach and perform transgastric ERCP. This procedure is performed in two stages during separate endoscopic sessions. The first stage consists of identifying the gastric remnant through EUS and placing a gastrostomy tube. The second stage consists of removing the gastrostomy tube and placing a metal stent through the fistula to allow introduction of the duodenoscope for performance of the ERCP. A study of six patients who underwent this procedure has shown that EUS guided access to the gastric remnant was successful in 100% of the cases. The average time of the procedure was 81 minutes. Antegrade ERCP was successfully performed in all six patients, with the two stages separated by an average of 5.8 days. 19
In our case, the bile duct was successfully canalized, a biliary sphincterotomy was performed, the bile duct was explored with a basket, and the stone was removed without complications. The patient evolved satisfactorily and was discharged at 72 hours.
In conclusion, the laparoscopic transgastric approach offers advantages including rapid access to the duodenum and adequate visualization of the papilla. This allows the use of a side view duodenoscope which increases both diagnostic and therapeutic performance. This approach also offers the possibility of subsequent access if required. Although surgical intervention is sometimes necessary, laparoscopic gastrostomy is associated with low rates of morbidity and mortality. For this reason, transgastric ERCP assisted by laparoscopy is a safe and successful method for management of biliary pathology in patients with modified anatomy following RYGB.
REFERENCES
1. Organización Mundial de la Salud. Informe sobre la situación mundial de las enfermedades no transmisibles. OMS [internet] 2017 [acceso el 15 de febrero de 2018]. Disponible en: Disponible en: https://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight [ Links ]
2. Ministerio de Salud y Protección Social. Análisis de Situación de Salud (ASIS) Colombia. MinSalud [internet] 2016 [acceso el 15 de febrero de 2018]. Disponible en: Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/ED/PSP/asis-colombia-2016.pdf [ Links ]
3. Secchi T, Falcao M, Cardoso A, Galvao M. Colangio-pancreatografía endoscópica retrógrada por acceso laparoscópico transgástrico. En: Campos J (editor). Endoscopia en cirugía de la obesidad. Sao Paulo: Amolca; 2009. p. 361-7. [ Links ]
4. Ramírez Rueda J, Garzón J. Cirugía bariátrica en el Hospital de San José, Bogotá D. C. Experiencia y resultados. Reper Med Cir. 2010;19:187-94. [ Links ]
5. Branco AJ, Noda RW, Kondo W, George MA, Rangel M. Colangiopancreatografía endoscópica retrógrada transgástrica laparoscópica poscirugía bariátrica. Rev Col Bras Cir. 2008;35:445-46. https://doi.org/10.1590/S0100-69912008000600016 [ Links ]
6. Aparcero M, Pacheco J, Giannopoulos I, Izzy A, Guerere K, Díaz A. Colangiopancreatografía asistida por laparoscopia en bypass gástrico y fistulotomía pre-corte por cálculo impactado en papila. GEN. 2017;71(1):13-6. [ Links ]
7. Li VK, Pulido N, Fajnwaks P, Szomstein S, Rosenthal R, Martinez-Duartez P. Predictors of gallstone formation after bariatric surgery: a multivariate analysis of risk factors comparing gastric bypass, gastric banding, and sleeve gastrectomy. Surg Endosc. 2009;23(7):1640-4. https://doi.org/10.1007/s00464-008-0204-6 [ Links ]
8. Moreels TG. Endoscopic retrograde cholangiopancreatography in patients with altered anatomy: How to deal with the challenges? World J Gastrointest Endosc. 2014;6(8):345-51. https://doi.org/10.4253/wjge.v6.i8.345 [ Links ]
9. Adler D, Baron T, Davila R, Egan J, Hirota W, Leighton J, et al. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005;62(1):1-8. https://doi.org/10.1016/j.gie.2005.04.015 [ Links ]
10. Peñaloza-Ramírez A, Leal-Buitrago C, Rodríguez-Hernández A. Adverse events of ERCP at San José Hospital of Bogotá (Colombia). Rev Esp Enferm Dig. 2009;101(12):837-49. [ Links ]
11. Moreels TG. ERCP in the patient with surgically altered anatomy. Curr Gastroenterol Rep. 2013;15(9):343. https://doi.org/10.1007/s11894-013-0343-3 [ Links ]
12. Liao WC, Angsuwatcharakon P, Isayama H, Dhir V, Devereaux B, Khor CJ, et al. International consensus recommendations for difficult biliary access. Gastrointest Endosc. 2017;85(2):295-304. https://doi.org/10.1016/j.gie.2016.09.037 [ Links ]
13. Bove V, Tringali A, Familiari P, Gigante G, Boškoski I, Perri V, et al. ERCP in patients with prior Billroth II gastrectomy: report of 30 years’ experience. Endoscopy. 2015;47(7):611-6. https://doi.org/10.1055/s-0034-1391567 [ Links ]
14. Iorgulescu A, Turcu F, Iordache N. ERCP after bariatric surgery-literature review and case report. J Med Life. 2014;7(3):339-42. [ Links ]
15. Inamdar S, Slattery E, Sejpal DV, Miller LS, Pleskow DK, Berzin TM, et al. Systematic review and meta-analysis of single-balloon enteroscopy-assisted ERCP in patients with surgically altered GI anatomy. Gastrointest Endosc. 2015;82(1):9-19. https://doi.org/10.1016/j.gie.2015.02.013 [ Links ]
16. Schreiner MA, Chang L, Gluck M, Irani S, Gan SI, Brandabur JJ, et al. Laparoscopy-assisted versus balloon enteroscopy-assisted ERCP in bariatric post-Roux-en-Y gastric bypass patients. Gastrointest Endosc. 2012;75(4):748-56. https://doi.org/10.1016/j.gie.2011.11.019 [ Links ]
17. Bertin PM, Singh K, Arregui ME. Laparoscopic transgastric endoscopic retrograde cholangiopancreatography (ERCP) after gastric bypass: case series and a description of technique. Surg Endosc . 2011;25(8):2592-6. https://doi.org/10.1007/s00464-011-1593-5 [ Links ]
18. Snauwaert C, Laukens P, Dillemans B, Himpens J, De Looze D, Deprez PH, et al. Laparoscopy-assisted transgastric endoscopic retrograde cholangiopancreatography in bariatric Roux-en-Y gastric bypass patients. Endosc Int Open. 2015;3(5):E458-63. https://doi.org/10.1055/s-0034-1392108 [ Links ]
19. Kedia P, Kumta NA, Widmer J, Sundararajan S, Cerefice M, Gaidhane M, et al. Endoscopic ultrasound-directed transgastric ERCP (EDGE) for Roux-en-Y anatomy: a novel technique. Endoscopy. 2015;47(2):159-63. https://doi.org/10.1055/s-0034-1390771 [ Links ]
Received: March 16, 2018; Accepted: August 21, 2018











 text in
text in