Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.3 Bogotá jul./set. 2019
https://doi.org/10.22516/25007440.449
Original articles
The role of endoscopic ultrasound in evaluating patients with dyspepsia in a Colombian population
1Especialista en gastroenterología y medicina interna. Hospital Universitario Nacional de Colombia, Hospital Occidente de Kennedy, Unidad de gastroenterología y endoscopia (UGEC). Bogotá, D. C., Colombia
2Profesor titular de medicina, coordinador de gastroenterología, Universidad Nacional de Colombia. Gastroenterólogo, Hospital Universitario Nacional de Colombia, Clínica Fundadores. Bogotá, D. C., Colombia
3Especialista en gastroenterología y medicina interna. Universidad San Martín, Hospital Occidente de Kennedy, Hospital Universitario Nacional de Colombia. Bogotá D. C., Colombia
Dyspepsia is defined as upper abdominal pain or discomfort that is considered to originate in the upper gastrointestinal tract. Many diseases and clinical conditions can cause dyspepsia. Among others, they include peptic ulcers, gastric and esophageal cancer, medications, biliary lithiasis, pancreatitis, and pancreatic cancer. Traditionally, dyspepsia is only evaluated with digestive endoscopy whose diagnostic yield is only 27%. On the other hand, endoscopic ultrasound combines an endoscopic image and an ultrasound image thereby potentially broadening diagnostic range to detect more of the causes of dyspepsia allowing treatment of patients in a timelier manner.
Objective:
To evaluate whether endoscopic ultrasound increases the diagnostic yield of endoscopy (27% in our environment) in the initial approach to previously unstudied dyspepsia.
Materials and methods:
This is a prospective study of analytical prevalence in adult patients with previously unstudied dyspepsia who were examined at a university institution in Colombia. The patients included were seen in the gastroenterology unit from January to October 2016 and underwent upper digestive endoscopy and endoscopic ultrasound. Under anesthesiologist-guided sedation, the stomach and duodenal esophagus were first evaluated endoscopically. Then retrograde endoscopic ultrasound was used to evaluate the pancreas in its entirety, the extra hepatic bile duct, the gallbladder, the celiac trunk, the left lobe of the liver and the mediastinal region. All abnormalities were noted on the patient’s admission form.
Results:
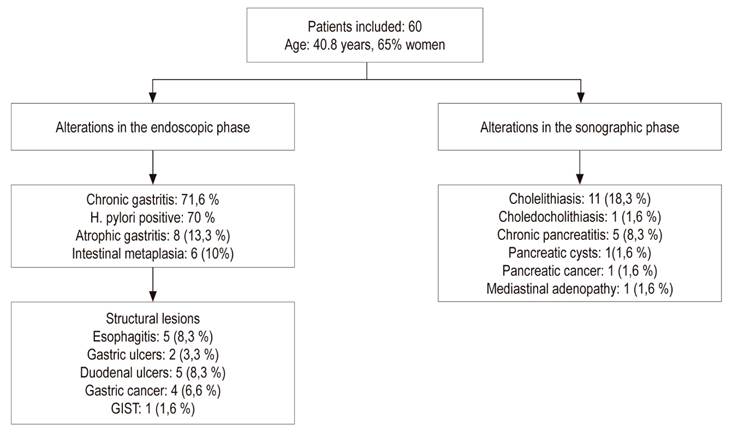
In total we included 60 patients of whom 65% were female and whose average age of was 40.8 years (SD: 12.5). The findings in the endoscopic phase of the endoscopic ultrasound were mainly chronic Gastritis 43 patients (71.6%), the rest had a structural lesion (17 patients): esophagitis 5 (8.3%), gastric ulcer 2 (3.3%), duodenal ulcer 5 (8.3%), gastric cancer, 4 (6.6%), gastric subepithelial lesion (GIST) 1 (1.6%). In the endoscopy phase, we found 11 cases of cholelithiasis (18.3%), one case of choledocholithiasis (1.6%), and five cases of chronic pancreatitis (8.3%). Only 17 patients of these patients (28.3%) had a structural finding in the endoscopy phase, but 18 additional patients (30%) had some positive finding in the ultrasound phase. In other words, the diagnostic yield rose to 58.3% (p < 0.001).
Conclusion:
Although this study’s sample size is small, it suggests that using endoscopic ultrasound in the initial evaluation of dyspepsia could be useful since it increased diagnostic yield in this group of patients from 28.3 to 58.3%. This is very significant because patients with dyspepsia and negative endoscopy are usually classified as functional and only treated with medications. However, in recognition of the methodological limitations of this study, it should be considered an initial exploration. Larger, controlled studies should be considered to confirm this work. Another factor that should be considered is the cost of endoscopic ultrasound which is much higher than the upper digestive endoscopy.
Keywords: Endoscopic ultrasound; evaluation; dyspepsia; gastric cancer
La dispepsia se define como un dolor o molestia abdominal superior que se considera originado en el tracto gastrointestinal superior. Muchas enfermedades y condiciones clínicas pueden producir dispepsia como la úlcera péptica, cáncer gástrico o esofágico, medicamentos, litiasis biliar, pancreatitis, cáncer de páncreas, entre otras. Por una parte, tradicionalmente la dispepsia solo se evalúa con la endoscopia digestiva y su producción solo es del 27 %. Por otra parte, la ecoendoscopia (ECE), al combinar una imagen endoscópica y una imagen ecográfica, podría ampliar el rango diagnóstico al detectar más causas de dispepsia que puedan ayudar a tratar al paciente de manera más oportuna.
Objetivo:
evaluar si la ECE aumenta el rendimiento diagnóstico que tiene la endoscopia (27 % en nuestro medio) en el enfoque inicial de la dispepsia no investigada (DPNI).
Materiales y métodos:
estudio prospectivo, de prevalencia analítica en pacientes adultos con DPNI, que consultaron a una institución universitaria de Colombia. Los pacientes incluidos consultaron a la unidad de gastroenterología durante el período comprendido entre enero a octubre del 2016 y se programaron para endoscopia digestiva alta (EDA). Bajo sedación guiada por anestesiólogo primero se realizó la fase endoscópica evaluando el esófago, estómago y duodeno; después se realizó la fase ecográfica y se inició el examen de manera retrógrada evaluándose el páncreas en su totalidad, la vía biliar extrahepática, la vesícula biliar, el tronco celíaco, el lóbulo izquierdo del hígado y la región mediastinal. Todas las anormalidades se anotaban en el formulario de ingreso del paciente.
Resultados:
En total se incluyeron a 60 pacientes, de los cuales el 65 % son de sexo femenino con un promedio de edad de 40,8 (desviación estándar: 12,5). Los hallazgos en la fase endoscópica de la ECE fueron principalmente gastritis crónica en 43 pacientes (71,6 %), el resto tenía una lesión estructural (17 pacientes): esofagitis en 5 (8,3 %), úlcera gástrica en 2 (3,3 %), úlcera duodenal en 5 (8,3 %), cáncer gástrico en 4 (6,6 %) y lesión subepitelial gástrica (GIST) en 1 (1,6 %). Los hallazgos en la fase ecográfica de la ECE fueron colelitiasis en 11 (18,3 %), coledocolitiasis en 1 (1,6 %) y pancreatitis crónica en 5 (8,3 %). Aunque solo el 28,3 % (17) de los pacientes con dispepsia tuvo un hallazgo estructural en la fase endoscópica, 18 pacientes (30 %) presentaron algún hallazgo positivo en la fase ecográfica, es decir que el rendimiento subió a un 58,3 % (p <0,001).
Conclusión:
este estudio, aunque pequeño, sugiere que la ECE como método inicial de enfoque en la evaluación de la dispepsia podría llegar a ser útil dado que aumenta el rendimiento diagnóstico en este grupo de pacientes, pasando de un 28,3 % a 58,3 %, lo cual es muy significativo si se tiene en cuenta que estos pacientes con dispepsia y endoscopia negativa usualmente se catalogan como funcionales y solo se les formula medicamentos. Sin embargo, se deben reconocer las fallas metodológicas del estudio y consideramos que es una exploración inicial y deben plantearse estudios más grandes y controlados para confirmar este trabajo; además, se debe tener en cuenta el costo del examen, que es mucho mayor que el de la EDA.
Palabras clave: Ecoendoscopia; evaluación; dispepsia; cáncer gástrico
Introduction
Dyspepsia is a clinical syndrome characterized by pain or discomfort in the upper abdomen. It affects at least 20% of the world’s population. 1,2 It has multiple causes including benign and malignant pathologies, negatively affects the quality of life, 8 and is often incorrectly called chronic gastritis or acid peptic disease. 3,4 In some countries the annual incidence of dyspepsia has been found to be approximately 1%, and has been estimated that one in two people will consult a physician for dyspeptic symptoms at some time in their lives. Dyspepsia accounts for 5% of the people seen by general practitioners and for approximately 20% to 30% of those seen by gastroenterologists. 5,6,7 When a patient has dyspepsia whose cause has not been determined, it is called uninvestigated dyspepsia (UD). 8 The approach to adult patients includes upper gastrointestinal endoscopy and occasionally includes upper abdominal ultrasound. 1,3 Dyspepsia can be secondary or organic if there are obvious alterations, it is called functional dyspepsia (FD) if examinations and images show no alterations that explain symptoms. 2,3
Early use of endoscopy is cost-effective, 9,10 but the timing of upper endoscopy varies from place to place. In developed countries, it is recommended after age 55, but in developing countries with high incidences of gastric cancer, it is recommended at age 35. 3 In Colombia, no studies of cost-effectiveness have been carried out for UD, but studies of the prevalence of endoscopic lesions in patients with UD have been performed. More than 10 years ago, a prospective study of patients with UD found that 73% had FD. 11. Another Colombian study of patients with UD found cholelithiasis in 21%. 12
Overall, the diagnostic yield of upper endoscopy alone for identification of organic causes does not exceed 30%,1,11 so other methods that have greater sensitivity need to be used. As understanding of these patients deepens, unknown causes may be found. In this regard, dyspepsia secondary to helicobacter pylori, a new entity that was previously included in the FD category, has recently been described. 13 It has now been shown that approximately 5% of patients with H. pylori can be cured of dyspepsia if the infection is eradicated. 13,14 This new finding demonstrates the need to continue investigating unknown etiologies that could explain dyspeptic symptoms. When upper endoscopy is negative in the traditional diagnostic approach, the diagnosis is FD. If no further studies are performed, the patient is treated with proton pump inhibitors (PPIs), prokinetic agents or antidepressants for several months. 8 This can mask unidentified pathologies that may lead to probable complications.
Endoscopic ultrasound (EUS) combines the image from conventional upper endoscopy with an ultrasound image. When radial equipment is used, the ultrasound image has a range of about 6 cm which can cover the entire esophagus, stomach or duodenum. 15 Since Pentax 360-Degree Radial-Array Ultrasound Gastroscopes are frontal, unlike Olympus Radial Ultrasound Endoscopes which are oblique, endoscopic views identical to those of conventional endoscopy can be obtained prior to the ultrasound phase. Visibility beyond the upper gastrointestinal lumen allows diagnoses of additional pathologies that may be associated with dyspepsia. Taking into account the high frequency of dyspepsia, as well as the lack of research other than the upper endoscopy in our environment, we decided to perform this study of EUS for diagnosis of patients with UD. The objective is to evaluate whether EUS increases the diagnostic yield from the 27% yield of conventional endoscopy here in Colombia.
Materials and methods
This is a prospective study of the prevalence of UD found in adult patients at a university institution in Colombia. The patients included came to the gastroenterology unit from January to October 2016 where they underwent upper endoscopy. After patients had agreed and signed consent forms, the Pentax echoendoscope was used instead of a conventional endoscope. On the basis of the ROME IV criteria, we defined dyspepsia as the presence of upper GI tract symptoms of postprandial fullness, early satiety and epigastric pain or burning. If no structural lesion is found endoscopically, it is defined as functional dyspepsia (FD). 8 Endoscopy indications used were those of the dyspepsia guide of the Colombian Association of Gastroenterology which recommends performing upper endoscopy in all patients with UD who are over 35 years old regardless of whether or not they have alarm symptoms. 16 We excluded patients who had any contraindication for performance of endoscopy with sedation, patients who had previously undergone upper endoscopy, patients with histories of gastrointestinal surgery including cholecystectomies, and patients who had had endoscopic retrograde cholangiopancreatography (ERCP), and patients who had had abdominal ultrasound images, magnetic resonance imaging (MRI) or computed tomography (CT). EUS was performed in the usual way. 17
Procedures were performed under sedation administered by an anesthesiologist. A Pentax echoendoscope, described above, was used. First, the endoscope was used to examine the esophagus, stomach and duodenum according to the protocol described by Yao. 18 This consists of the evaluation of 21 areas in the proximal, middle and distal third of the stomach using both direct view and rearview. Two biopsies each were taken from the antrum and the corpus to check for H. pylori infections. Additional biopsies were taken when patients had apparent structural lesions. After the ultrasound phase, EUS was used to the major papilla. A retrograde evaluated the entire pancreas, the extrahepatic bile duct, the gallbladder, the celiac trunk, the left lobe of the liver and the mediastinal region. All abnormalities were noted on the patient’s admission form. The protocol, investigation and informed consent form were approved by the ethics committee of the participating institution.
Results
In total, sixty patients with an average age of 40.8 years + 12.5 years were included. Sixty-five percent of them were women. In the first phase, forty-three of the patients (71.6%) were endoscopically diagnosed with chronic gastritis while 17 had structural lesions including five cases of esophagitis in 5 (8.3%), two cases of gastric ulcers (3.3%), five cases of duodenal ulcers (8.3%), four cases of histologically proven gastric cancer (6.6%), and one case of a gastrointestinal stromal tumor (GIST) (1.6%). H. pylori was found in 42 patients (70%), atrophic gastritis was found in 8 patients (13%), and intestinal metaplasia was found in six (10%).
In the second phase, EUS found cholelithiasis in 11 patients (18.3%), choledocolithiasis in one (1.6%), chronic pancreatitis defined according to by Rosemont’s criteria in five (8.3%), a pancreas cyst suggestive of mucinous cystadenoma in one (1.6%), stage T2 pancreatic cancer in one (1.6%) and mediastinal adenopathies in one patient who also had gastric cancer (1.6%). (19) Overall, 17/60 patients (28.3%) had structural alterations found in the endoscopy phase and 18/60 (30%) had some positive finding that had not been found in the endoscopic phase. In other words, these cases would have been technically considered to have FD. Only 25 patients (41.6%) had no findings in both the endoscopy phase and the EUS phase. In all cases, the gallbladder, bile duct, head, body and tail of the pancreas were properly visualized. Overall findings are shown in Figure 1.
Discussion
This study found that 28.3% of the patients with UD had alterations found during the endoscopic phase which is similar to the 27% found in a previous investigation by the National University and which corroborates the poor performance of upper endoscopy in our environment. 11 In the ultrasound phase using EUS equipment with frontal vision, additional lesions that could explain dyspeptic symptoms were detected in 30% of the patients for a total of 58.3% (p <0.001). In other words, only 25 (41.6%) of the 60 patients had normal results.
The finding of cholelithiasis in 18% of patients coincides with the prevalence of this pathology in the west. 20,21 However, it cannot be concluded that gallbladder stones cause dyspeptic symptoms since the symptom most frequently associated with them is colic. To determine the association of the two, a study with a greater number of patients, probably a case and control study, would be required. However, all gastroenterologists know that patients with cholelithiasis do not necessarily manifest the typical colic in the right hypochondrium but may manifest postprandial symptoms in the epigastrium which are very suggestive of dyspepsia. If the finding of cholelithiasis is eliminated, the diagnostic yield of EUS exceeds that of upper endoscopy by 12%. Given the types of pancreatic pathologies found, it can be inferred that when only upper endoscopy is taken into account for UD patients, negative findings can lead to the erroneous conclusion that the patient has FD which should be managed with prolonged administration of prokinetics, PPIs or antidepressants. 22 These medications would not achieve significant improvement but could generate anxiety in patients. For the safety of patients and doctors, in many cases research into the cause of dyspepsia should continue with additional tests such as abdominal ultrasound, CT scans and other studies. 8,22
A new approach for patients with FD and persistent symptoms is posed by the findings that more than 11% of UD patients have pancreatic pathologies while others suffer from choledocholithiasis. For these patients, the next step should be biliopancreatic EUS rather than another upper endoscopy. EUS is even preferable to conventional ultrasound, CT scans and abdominal MRI. A study conducted more than 15 years ago suggested that the EUS could also be more cost-effective. 23 A more recent study from the United States by Chang et al. showed that, in the presence of symptoms, using EUS as the first exam is more cost-effective than upper endoscopy followed by abdominal ultrasound. 24 Compared to abdominal CT scans and MRI, the advantages of EUS are even more evident. Taking into account our results and those of international studies, we consider that it is necessary and timely to determine the place of biliopancreatic EUS in patients with UD in our environment. We consider that it would be premature to recommend this test for all patients with UD given the high cost of EUS in our setting. Nevertheless, the prevalence of biliopancreatic pathologies demonstrates that it should become the test of choice for FD patients who do not improve with conventional treatments.
A very important issue is that complexity of EUS has been exaggerated here in Colombia. Performing gastroesophageal or pancreatic EUS is relatively simple, does not take more than 5 or 10 minutes, and training is not very complex. This recalls what happened with the introduction of ERCP in Colombia more than 50 years ago. It was considered to be a very complex procedure that could only be performed by a very few gastroenterologists in very few medical centers. Currently, ERCPs are routine procedures performed by many gastroenterologists the world over, and ERCP is a much more complex and dangerous procedure than is EUS. 24 The real complexity of EUS lies in therapeutic and invasive procedures such as staging of pancreatic cancer, punctures and drainage. It is time to demystify non-therapeutic EUS and understand reality. It is not difficult to imagine that EUS could be used for initial evaluation of UD in the near future. This is a complex pathology that, curiously, many consider to be an insignificant or easy-to-solve problem when it is called gastritis or acid peptic disease. In fact, addressing it is complex due to its recurrent nature. In addition, it causes deterioration of patients’ quality of life, has high costs for the world’s health care systems, and can have serious unsuspected etiologies, such as those found in this study.
To our knowledge, this is the first study of this type on the initial evaluations of patients with dyspepsia using EUS with frontal equipment done in Latin America. A study with a similar design done more than 15 years ago used an Olympus echoendoscope which only provides oblique views. 25 That study did not detect as many endoluminal lesions as did endoscopy. Unlike the Fuji and Pentax equipment, Olympus echoendoscopes do not have frontal vision, which makes it impossible to use for conventional endoscopy. 15 Because it limits the endoscopic phase, many areas cannot be evaluated which can leave lesions such as ulcers and tumors undiscovered.
It is also important to keep in mind that defensive medicine is frequently exercised. 26 Many patients press their doctors to reach a rapid diagnosis because they are anxious about their conditions and do not accept that their pain is only explained by gastritis. When the doctor is influenced, multiple tests that may even be more expensive than an EUS can be the result.
The limitations of this study include its sample size (not calculated) and the fact that it was performed at only one center. It would be convenient to conduct studies with larger samples to confirm the findings of this study.
Conclusion
This study was found that the diagnostic yield of EUS exceeds that of upper endoscopy by 30% in patients with UD. EUS identified pathologies in 58.3% of the patients whereas upper endoscopy alone could only identify them in 28.3% of the patients (p <0.001). When upper endoscopy is negative for a patient with UD, current recommendations call for a diagnosis of FD and indefinite prescription of medications whose efficacy is moderate. Our findings indicate the potential for using EUS as the initial evaluation examination as well as the potential for using it as a follow-up examination instead of a CT scan or MRI when symptoms persist. Studies of the cost-effectiveness of EUS for these purposes in our environment should be undertaken to determine whether this test should become the first choice instead of conventional endoscopy.
Referencias
1. Graham DY, Rugge M. Clinical practice: diagnosis and evaluation of dyspepsia. J Clin Gastroenterol. 2010;44(3):167-72. https://doi.org/10.1097/MCG.0b013e3181c64c69. [ Links ]
2. Tack J, Talley NJ, Camilleri M. Functional gastroduodenal disorders. Gastroenterology 2006;130:1466-79. https://doi.org/10.1053/j.gastro.2005.11.059. [ Links ]
3. Otero W, Gómez M, Otero L. Enfoque del paciente con dispepsia y dispepsia funcional. Rev Colomb Gastroenterol. 2014;29:132-8. [ Links ]
4. Talley NJ, Ford AC. Functional dyspepsia. N Engl J Med. 2015;373:1853-63. https://doi.org/10.1056/NEJMra1501505. [ Links ]
5. Halder SLS, Talley NJ. Functional dyspepsia: A New Rome III Paradigm. Curr Treat Options Gastroenterol. 2007;10(4):259-72. https://doi.org/10.1007/s11938-007-0069-0. [ Links ]
6. Talley NJ, Vakil NB, Moayyedi P. American gastroenterological association technical review on the evaluation of dyspepsia. Gastroenterology . 2005;129(5):1756-80. https://doi.org/10.1053/j.gastro.2005.09.020. [ Links ]
7. Talley NJ, Vakil N. Practice Parameters Committee of the American College ofGastroenterology . Guidelines for the management of dyspepsia. Am J Gastroenterol. 2005;100(10):2324-37. https://doi.org/10.1111/j.1572-0241.2005.00225.x. [ Links ]
8. Stanghellini V, Chan FK, Hasler WL, Malagelada JR, Suzuki H, Tack J, et al. Gastroduodenal disorders. Gastroenterology. 2016;150:1380-92. https://doi.org/10.1053/j.gastro.2016.02.011. [ Links ]
9. Delaney BC, Wilson S, Roalfe A, Roberts L, Redman V, Wearn A, et al. Cost effectiveness of initial endoscopy for dyspepsia in patients over age 50 years: a randomised controlled trial in primary care. Lancet. 2000;356(9246):1965-9. [ Links ]
10. Bytzer P. Diagnostic approach to dyspepsia. Best Pract Res Clin Gastroenterol. 2004;18:681-93. https://doi.org/10.1016/j.bpg.2004.04.005. [ Links ]
11. Pineda LF, Otero W, Gómez M, Arbeláez V. Enfermedad estructural y valor predictivo de la Historia Clínica en pacientes con dispepsia no investigada. Rev Col Gastroenterol. 2004;19:13-25. [ Links ]
12. Gómez M, Otero W, Rincón J. Frecuencia de colelitiasis en dispepsia funcional, enfermedad por reflujo gastro-esofágico y en pacientes asintomáticos. Rev Colomb Gastroenterol . 2007;22(3):64-172. [ Links ]
13. Sugano K, Tack J, Kuipers EJ. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015;64:1353-67. https://doi.org/10.1136/gutjnl-2015-309252. [ Links ]
14. Malfertheiner P, Megraud F, O’Morain CA, Gisbert JP, Kuipers EJ, Axon AT, et al. Management of Helicobacter pylori infection: The Maastricht V/Florence Consensus Report. Gut. 2017;66:6-30. https://doi.org/10.1136/gutjnl-2016-312288. [ Links ]
15. Bamber J, Cosgrove D, Dietrich CF, Fromageau J, Bojunga J, Calliada F, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: Basic principles and technology. Ultraschall Med. 2013;34(2):169-84. https://doi.org/10.1055/s-0033-1335205. [ Links ]
16. Pineda LF, Rosas MC, Amaya M, Rodríguez A, Luque A, Agudelo F, et al. Guía de Práctica Clínica para el diagnóstico y tratamiento de la dispepsia en adultos. Rev Colomb Gastroenterol . 2015;30(Suppl 1):9-16. [ Links ]
17. Godfrey EM, Rushbrook SM, Carroll NR. Endoscopic ultrasound: a review of current diagnostic and therapeutic applications. Postgrad Med J. 2010;16(4):111-22. https://doi.org/10.1136/pgmj.2009.096065. [ Links ]
18. Yao K. Endoscopic diagnosis of early gastric cancer. Ann Gastroenterol. 2013;26(1):11-22. [ Links ]
19. Catalano MF, Sahai A, Levy M, Romagnuolo J, Wiersema M, Brugge W, et al. EUS-based criteria for the diagnosis of chronic pancreatitis: the Rosemont classification. Gastrointest Endosc. 2009;69(7):1251-61. https://doi.org/10.1016/j.gie.2008.07.043. [ Links ]
20. Russo MW, Wei JT, Thiny MT, Gangarosa LM, Brown A, Ringel Y, et al. Digestive and liver diseases statistics, 2004. Gastroenterology . 2004;126(5):1448-53. https://doi.org/10.1053/j.gastro.2004.01.025. [ Links ]
21. Sakorafas GH, Milingos D, Peros G. Asymptomatic cholelithiasis: is cholecystectomy really needed? A critical reappraisal 15 year after the introduction of laparoscopic cholecystectomy. Dig Dis Sci. 2007,52:1313-25. https://doi.org/10.1007/s10620-006-9107-3. [ Links ]
22. Enck P, Azpiroz F, Boeckxstaens G, Elsenbruch S, Feinle-Bisset C, Holtmann G, et al. Functional dyspepsia. Nat Rev Dis Primers. 2017;3:17081. https://doi.org/10.1038/nrdp.2017.81. [ Links ]
23. Sahai AV, Penman ID, Mishra G, Williams D, Pearson A, Wallace MB, et al. An assessment of the potential value of endoscopic ultrasound as a cost-minimizing tool in dyspeptic patients with persistent symptoms. Endoscopy. 2001;33(8):662-7. https://doi.org/10.1055/s-2001-16223. [ Links ]
24. Chang KJ, Erickson RA, Chak A, Lightdale C, Chen YK, Binmoeller KF, et al. EUS compared with endoscopy plus transabdominal US in the initial diagnostic evaluation of patients with upper abdominal pain. Gastrointest Endosc . 2010;72(5):967-74. https://doi.org/10.1016/j.gie.2010.04.007. [ Links ]
25. Lee YT, Lai AC, Hui Y, Wu JC, Leung VK, Chan FK, et al. EUS in the management of uninvestigated dyspepsia. Gastrointest Endosc . 2002;56(6):842-8. [ Links ]
26. Studdert DM, Mello MM, Sage WM. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293:2609-261. https://doi.org/10.1001/jama.293.21.2609 [ Links ]
Received: March 25, 2018; Accepted: August 29, 2018











 texto en
texto en