Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.3 Bogotá July/Sept. 2019
https://doi.org/10.22516/25007440.214
Case report
A case of heterotopic pancreas in a gastric polyp
1Especialista de primer grado en Anatomía Patológica. Instructor. Hospital Provincial Docente Manuel Ascunce Domenech. Camagüey, Cuba.
2Especialista de segundo grado en Medicina Interna. Profesor titular. Hospital Provincial Docente Manuel Ascunce Domenech. Camagüey, Cuba.
3Especialista de primer grado en Medicina Interna. Instructor. Hospital Provincial Docente Manuel Ascunce Domenech. Camagüey, Cuba.
4Especialista de segundo grado en Medicina Interna. Profesor auxiliar. Hospital Provincial Docente Manuel Ascunce Domenech. Camagüey, Cuba.
Pancreatic heterotopia is rare and is sometimes found accidentally. It can occur anywhere in the digestive tract and even outside of it. Heterotopic pancreas is congenital, but its pathogenesis is under discussion. Although it develops slowly and progressively, its behavior is benign and asymptomatic. Nevertheless, it can manifest in obstructions, hemorrhaging, inflammation and neoplasia. In the latter case, histopathological diagnosis is essential. We present the case of a symptomatic patient with pancreatic heterotopia at the gastric pylorus, a very uncommon location.
Keywords: Heterotopic pancreas; gastric polyp
La heterotopia pancreática es un hallazgo poco frecuente, en ocasiones accidental, que se puede observar en cualquier nivel del tracto digestivo e inclusive fuera del mismo; es congénita y su patogenia está en discusión. Aunque su forma de presentación es lenta y progresiva y su comportamiento benigno y asintomático, en ocasiones puede originar manifestaciones obstructivas, hemorrágicas, inflamatorias y neoplásicas. En este último caso es imprescindible el diagnóstico histopatológico. Se presenta el caso de un paciente sintomático con heterotopia pancreática a nivel del píloro gástrico cuya localización es bastante infrecuente.
Palabras clave: Páncreas heterotópico; pólipo gástrico
Introduction
Pancreatic heterotopia (PH), also known as heterotopic pancreas and ectopic pancreas, is characterized by normal pancreatic tissue in a different anatomical structure or site without vascular, neuronal or anatomical continuity with the pancreas. 1 The authors consulted point to Shultz as the person responsible for the first description of PH in 1727. They also agree that, in 1859, Klob was the first to offer histopathological confirmation while in 1916 Otschkin first reported PH in the gallbladder. 2 The frequency of this finding is calculated at between 0.11% and 13.7%. It is usually an incidental finding of autopsies or surgical procedures and is rarely found intentionally. 3 Its most frequent sites are the duodenum (30.3%), stomach (26.5%), jejunum (16.3%), ileum (5.8%) and Meckel’s diverticulum (5.3%). It also occurs in the gallbladder, extrahepatic bile ducts, the Ampulla of Vater, the mesentery, bladder, lung, esophagus, thyroid, colon and spleen. 3
Von Heinrich 4 classified PH morphologically into three varieties: Type I has all the elements of a normal pancreas, type II has no pancreatic islets and type III has only ducts surrounded by entangled fascicles of smooth muscle. These lesions are known as adenomyomata or mucoepithelial hamartomata. 3
Other classifications such as the 2010 effort of Bromberg et al. 5 have multiple adherents.
Although the typical endoscopic ultrasound features of the PH include heterogeneous echogenicity, indistinct borders and a location within two or more layers, it can also exhibit hypoechoic homogenous echogenicity and a distinct border within the fourth ultrasound (muscularis propria) layer similar to the endoscopic ultrasound characteristics of gastrointestinal stromal tumors. 6
Despite the development of modern diagnostic procedures such as endoscopic ultrasound, computed tomography (CT) and gastroduodenoscopy, diagnosis remains difficult.
Asymptomatic patients diagnosed with PH should remain under medical supervision with periodic follow-ups. Patients without symptomatic complications should have their lesions removed, preferably by local resection. In sites accessible to endoscopy, endoscopic excision can be performed successfully in experienced hands in selected patients at appropriate institutions. The use of endoscopic ultrasound in this type of intervention is essential. 7
Complications in ectopic pancreatic tissue are similar to those that occur in a normal pancreas and include acute pancreatitis, pancreatic cancer, insulinomas, gastrinomas and cystic degeneration 2,3,8,9.
The objective of this work is to present the extremely rare case of a patient with pancreatic heterotopia. After presenting upper digestive manifestations refractory to conventional treatment, digestive endoscopy found gastric polypoid thickening and histopathological studies confirmed pancreatic heterotopia.
Clinical case
The patient was a 66-year-old retired man who had a history of degenerative osteoarthritis and was being treated with non-steroid anti-inflammatory drugs (NSAIDs) at maximum dosage. He came to the hospital after two months of burning abdominal pain in the epigastrium that was exacerbated by food consumption and was accompanied by retrosternal burning and gastroesophageal regurgitation. A gastroenterological assessment concluded with a diagnosis of NSAID gastropathy, so treatment with proton pump inhibitors (PPIs) and dopamine agonists was started. Twenty days later he returned because of persistent symptoms which had not improved.
Physical Examination
Physical examination showed that the patient was obese, his skin and mucous membranes were without alterations, and subcutaneous cellular tissue had not been infiltrated.
Cardiorespiratory System
His respiratory rate was 19 breaths per minute. He had a normal vesicular murmur without rales, a central heart rate of 96 beats per minute (bpm) and blood pressure of 125∕85.
Digestive system
His abdomen was globular, soft, and depressible. It was painful upon deep palpation in the epigastrium and mesogastrium, but there were no visceromegaly, abdominal masses, or abdominal murmurs.
Otherwise, the physical exam found no alterations.
Blood Tests
Blood tests found hemoglobin of 125 g/L, leucocytes of 9 × 109 g/L with normal differential formula, and a globular sedimentation rate of 55 mm/first hour. Cholesterol, triglycerides, blood sugar, uric acid, urea, creatinine, total and fractionated proteins, and liver functions were normal. In addition, hospital policies require a test for syphilis (VDRL) which was not reactive and ELISA for HIV which was negative.
Chest radiography was normal. Abdominal ultrasound found a diffuse, echogenic liver without dilated bile ducts. The pancreas had no alterations. The kidneys were normal size, without lithiasis or dilation. The bladder and prostate had no abnormalities. The x-ray of the esophagus, stomach and duodenum was inconclusive for the diagnosis.
Esophagogastroduodenoscopy
Stomach: A polypoid thickening of approximately 1.5 cm of the same color as the surrounding mucosa was found in the gastric antrum. It was exophytic, did not contain any erosions, and had a central depression through the duct exit (Figure 1). A biopsy of showed that it was pancreatic heterotopia type I (Figures 2 and 3).
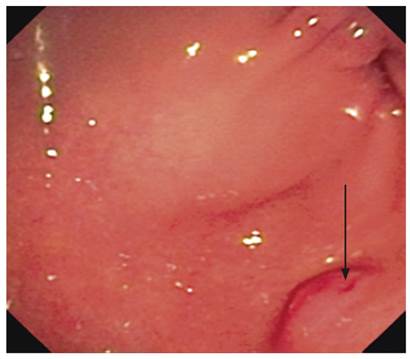
Figure 1 Endoscopic image of the antrum. Elevated submucosal lesion simulating a tumor in the antrum. Note the small depression at the exit of the duct.
Esophagus: The first and second portion of the duodenum were without alterations.
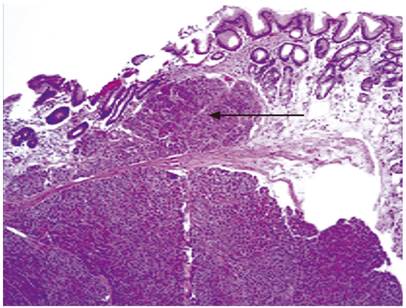
Figure 2 Panoramic image. Note the well-defined lesion in the submucosa and muscularis mucosae. H/E, 20 X.
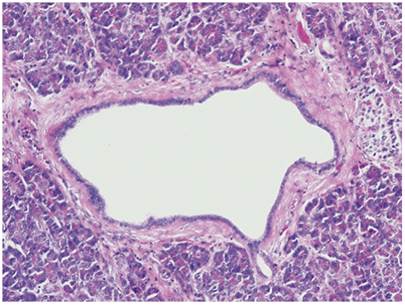
Figure 3 Image with higher magnification shows heterotopia type I. Note the ducts, acini and small islet nests to the right. H/E, 40 X.
After the diagnosis made, doses of the medications were modified, NSAIDs were suspended, and a date for surgery was scheduled. Given the histopathological result and the persistence of symptoms, the area of the gastric wall in which the ectopic tissue was implanted was excised. Three cm of healthy tissue surrounding the lesion were resected.
Discussion
Although PH is linked to organogenesis, it is usually discovered in adulthood. It is normally present as a benign and asymptomatic entity from birth. It is most common in males. Among females, it is found more often in girls and adolescents than in adult women. The most common form in female patients is gallbladder PH. 3,5 This patient was a 66 year old man.
Several hypotheses have emerged to try to explain the pathogenesis of PH. They include origin as a hamartoma such as focal glandular hyperplasia, reactive changes in response to a persistent harmful stimulus, diverticular invagination and fibro-adenomatous involution associated with old age. 10
Cytokeratins detected by immunohistochemistry in adenomyomata are similar to those exhibited by the normal biliary and pancreatic duct systems. They test positive for cytokeratin 7 and negative for cytokeratin 20 (CK 7 +/CK 20‒). For this reason, comparisons of this expression profile with the expression profile of the intestinal epithelium show an inverted pattern (CK 7 -/CK 20+), as demonstrated by Takahashi and Fukusato based on previous work by Babal, Handra-Luca and Yao. 8-11 Macroscopically, PH can be found either as a unique, firm, well-defined nodule ranging in size from 1 mm to 5 cm, or in clusters. In our case, it was a unique mass measuring 1.5 cm. They can be located anywhere on visceral wall in the submucosa. They are either solid or cystic, and at their edges they are whitish to yellow and often have a duct (or ducts) leading to the lumen, as in our patient. This is more likely when PH is found in or near Meckel’s diverticulum. 11 Histologically, the components of the exocrine and endocrine duct system are distinguished in different proportions and combinations, as in our patient.
Most asymptomatic cases of PH are not recognized prior to surgery. They are discovered during surgery, histological study of the anatomical piece, abdominal examination or during an autopsy. 12 In cases of confirmed diagnosis in asymptomatic patients, the recommendation depends on the lesion’s location and resectability. Potential for malignancy must always be taken into account. 11 Sometimes, monitored waiting is indicated, but if an incidental surgical finding is treated, it is advisable to perform complete resection to avoid late complications and the need for reoperation. 12
About 30% to 40% of PH cases have gastrointestinal symptoms, as in this case, or complications such as acute pancreatitis, pancreatic cancer, insulinoma, gastrinomas and cystic degeneration. 9 Differential diagnosis should be made for leiomyomas, lymphomas, neuroendocrine tumor, gastrointestinal stromal tumor and metastatic lesions. 2,3
Principal diagnostic studies include gastroduodenoscopy, CT scans and endoscopic ultrasound. The latter was not available to us at the time of the study, but it is usually a very useful resource for detecting tumors smaller than 2 cm even though it is not specific and cannot exclude other pathologies such as carcinoids, fibroids, eosinophilic granulomas and leiomyomas. In symptomatic patients, surgical examination is usually required to make a definitive diagnosis and to exclude other types of lesions including neoplasia.
Conclusions
PH is infrequently diagnosed but is most often discovered in the duodenum, stomach, jejunum, ileum and Meckel’s diverticulum. It may also be found in locations outside the digestive tract. A definitive diagnosis is often difficult. In this case, it was confirmed by histopathological studies.
Referencias
1. Yuan Z, Chen J, Zheng Q, Huang XY, Yang Z, Tang J. Heterotopic pancreas in the gastrointestinal tract. World J Gastroenterol. 2009;15(29):3701-3. https://doi.org/10.3748/wjg.15.3701. [ Links ]
2. Watanabe M, Shiozawa K, Kishimoto Y, Arai T, Nakano S, Kikuchi Y, et al. Heterotopic Pancreas of the Jejunum Incidentally Detected by Preoperative Abdominal CT: Report of Two Cases and Review of the Literature. Case Rep Gastroenterol. 2012;6(3):576-82. https://doi.org/10.1159/000343093. [ Links ]
3. Karpińska MS, Nienartowicz M, Markowska-Woyciechowska A, Budrewicz-Czapska K. Heterotopic pancreas in the stomach (type II according to Heinrich) - literature review and case report. Pol Przegl Chir. 2011;83(3):171-4. https://doi.org/10.2478/v10035-011-0026-4. [ Links ]
4. Von Heinrich H., Beitrag Zur Histologie des Sogen: akzessorischen Pankreas. Virchows Arch A Pathol Anat Histhopathol. 1909;198:392-401. https://doi.org/10.1007/BF02085327. [ Links ]
5. Bromberg S, Neto C, Borges A. Heterotopia pancreática: análisis clínico patológico de 18 pacientes. Rev Col Bras Cir. 2010;37(6):413-9. https://doi.org/10.1590/S0100-69912010000600007. [ Links ]
6. Chou JW, Cheng KS, Ting CF, Feng CL, Lin YT, Huang WH. Endosonographic features of histologically proven gastric ectopic pancreas. Gastroenterol Res Pract. 2014;2014:160601. https://doi.org/10.1155/2014/160601. [ Links ]
7. Bromberg SH, Camilo Neto C, Borges AF, Franco MI, França LC, Yamaguchi N. Pancreatic heterotopias: clinicopathological analysis of 18 patients. Rev Col Bras Cir. 2010;37(6):413-9. [ Links ]
8. Takahashi Y, Fukusato T. Adenomyoma of the small intestine. World J Gastrointest Pathophysiol. 2011;2(6):88-92. https://doi.org/10.4291/wjgp.v2.i6.88. [ Links ]
9. Babál P, Zaviacic M, Danihel L. Evidence that adenomyoma of the duodenum is ectopic pancreas. Histopathology. 1998;33(5):487-8. https://doi.org/10.1046/j.1365-2559.1998.0491d.x. [ Links ]
10. Handra-Luca A, Terris B, Couvelard A, Bonte H, Flejou JF. Adenomyoma and adenomyomatous hyperplasia of the Vaterian system: clinical, pathological, and new immunohistochemical features of 13 cases. Mod Pathol. 2003;16(6):530-6. https://doi.org/10.1097/01.MP.0000073525.71096.8F. [ Links ]
11. Yao JL, Zhou H, Roche K, Bangaru BS, Ginsburg H, Greco MA. Adenomyoma arising in a meckel diverticulum: case report and review of the literature. Pediatr Dev Pathol. 2000;3(5):497-500. https://doi.org/10.1007/s100240010097. [ Links ]
12. Lasky Davio M, Melgoza C, Benbassat M, Rescala E, Baquera J. Páncreas heterotópico de la vesícula biliar. AMCE. 2004,5(2):107-9. [ Links ]
Received: February 22, 2018; Accepted: May 09, 2018











 text in
text in 


