Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.3 Bogotá July/Sept. 2019
https://doi.org/10.22516/25007440.451
Case report
Case report and literature review of Budd-Chiari syndrome during the puerperium
1Médico Internista, Fellow de Hepatología Clínica, Universidad de Antioquia, Medellín, Colombia
2Médico y Cirujano, Residente de Medicina Interna, Universidad Libre, Cali, Colombia
3Estudiante de Pregrado, Facultad de Medicina, Universidad Pontificia Bolivariana, Medellín, Colombia
4Unidad de hepatología y trasplante hepático Hospital Pablo Tobón Uribe; Profesor Universidad Pontifica Bolivariana, Medellín, Colombia
Budd-Chiari syndrome is defined as obstruction of hepatic blood outflow. This obstruction can be located anywhere from the small hepatic veins at the entrance of the inferior vena cava to the right atrium. Most cases are primary Budd-Chiari syndrome which is caused by endoluminal thrombosis. Secondary Budd-Chiari syndrome occurs as the result of extrinsic compression associated with space-occupying lesions such as malignant tumors. Hereditary thrombophilic states are the main risk factors, but since pregnancy and the puerperium are hypercoagulable states, they can be associated with Budd-Chiari syndrome. Nevertheless, the prevalence of this type of case in the literature varies according to the population studied. There have been no studies on the incidence or prevalence of this disease in Colombia. The small number of case reports here have not been related to pregnancy.
We report the case of a patient who developed Budd-Chiari syndrome 12 weeks postpartum. Our report includes management and clinical evolution as well as a review of the literature of cases associated with pregnancy.
Keywords: Budd-Chiari syndrome; postpartum period; venous thrombosis
El síndrome de Budd-Chiari es una entidad definida como la obstrucción al flujo sanguíneo en el tracto de salida hepático. Esta obstrucción se puede localizar desde las pequeñas venas hepáticas hasta la entrada de la vena cava inferior a la aurícula derecha. En la mayoría de los casos, se ocasiona por una trombosis endoluminal conocida como Budd-Chiari primario y secundario, cuando ocurre por una compresión extrínseca asociada a las lesiones que ocupan espacio como malignidad. Por tanto, los estados trombofílicos hereditarios se conocen como los principales factores de riesgo. El embarazo y el puerperio, al ser estados hipercoagulables, se pueden asociar al síndrome de Budd-Chiari, sin embargo, la prevalencia reportada en la literatura es muy variable dependiendo de la población estudiada. En Colombia no hay estudios de incidencia o prevalencia de la enfermedad; existen varios reportes de caso, pero no relacionados con el embarazo. Reportamos el caso de una paciente, que 12 semanas posparto presentó un síndrome de Budd-Chiari; además presentamos el manejo ofrecido, la evolución clínica y una revisión de la literatura de los casos asociados con el embarazo.
Palabras clave: Síndrome de Budd-Chiari; periodo posparto; trombosis de la vena
Introduction
Budd-Chiari syndrome is a condition in which hepatic venous flow is obstructed anywhere from the hepatic veins to the site of attachment to the inferior vena cava and the right atrium. 1 It can be divided into primary and secondary. Primary Budd-Chiari syndrome is intraluminal vascular compromise usually due to thrombosis while secondary Budd-Chiari syndrome is due to extrinsic compression of the venous bed. Accepted causes of secondary obstruction include liver transplantation, liver resection, cardiac surgery, extrinsic compression and tumor invasion. 2 Epidemiology varies greatly throughout the world: in Denmark there is an incidence of 0.5 cases/million people/year while in Japan the prevalence reaches 2.4/million people with approximately 20 new cases each year. 3,4 Established risk factors are include myeloproliferative syndromes, antiphospholipid syndrome, nocturnal paroxysmal hemoglobinuria, hyperhomocysteinemia, mutations of Factor V Leiden, mutations of the prothrombin gene (G20210A), deficiencies of C and S proteins, pregnancy, the puerperium, poverty and family history. 2 Pregnancy, a particularly hypercoagulable physiological state in preparation for childbirth, increases the risk of thromboembolic events with an incidence that is 7-10 times higher than in controls of the same age. 5,6
Similarly, there is clinical evidence that the risk continues during postpartum with a much higher incidence than among non-pregnant controls. 7 The literature on Budd-Chiari syndrome’s relation to pregnancy and the puerperium reports rates of prevalence that vary greatly. 8 This article reports a case of postpartum Budd-Chiari syndrome. We highlight the importance of taking into account pregnancy and the puerperium as risk factors in this group of patients.
Clinical case description
Our patient was a 14-year-old Afro-Colombian patient from the urban area of Quibdó, Chocó who had had a spontaneous term delivery without complications followed by postpartum contraception with depot medroxyprogesterone acetate. She had no other relevant medical history. In the second postpartum month, she developed generalized abdominal pain, increased abdominal perimeter and jaundice, but she did not consult until one month after the onset of symptoms at which time she had an episode of hematemesis.
Physical examination found that the whites of her eyes were jaundiced, and she had ascites and a palpable hepatomegaly four centimeters from the right costal edge. Digestive endoscopy showed hypertensive gastropathy and esophageal varices grade II. They were ligated endoscopically. She required paracentesis twice to evacuate ascitic fluid (5,000 and 7,000 mL) which had a high albumin gradient. The Doppler study of hepatic circulation showed an absence of flow in the suprahepatic veins. An abdominal CT scan showed portal hypertension (collateral circulation and ascites) with extensive thrombosis of the suprahepatic veins and hepatomegaly compressing the vein cava (Figure 1). This confirmed the diagnosis of subacute postpartum Budd-Chiari syndrome. Laboratory studies are described in Table 1. The Rotterdam score, a prognostic index for Budd-Chiari syndrome, was 1.16 which placed her at intermediate risk. Studies were extended in search of thrombophilia to explain the etiology of the clinical picture, but none of these tests were positive. This confirmed the causal relationship between the hypercoagulable state of the puerperium as and Budd-Chiari syndrome. We considered that the use of medroxyprogesterone had probably enhanced the thrombotic condition.
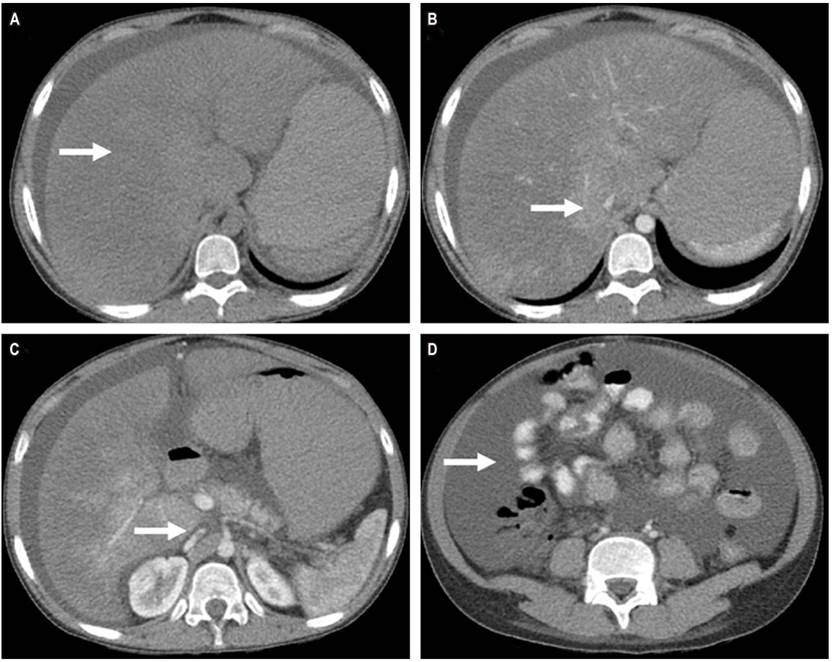
Figure 1 CT scan of the abdomen and pelvis. A. Phase without contrast shows hepatomegaly. B. Contrasted phase shows absence of suprahepatic vein flow. C. Contrasted phase shows compression of the inferior vena cava. D. Contrasted phase shows ascites.
Table 1 Laboratory Test Results
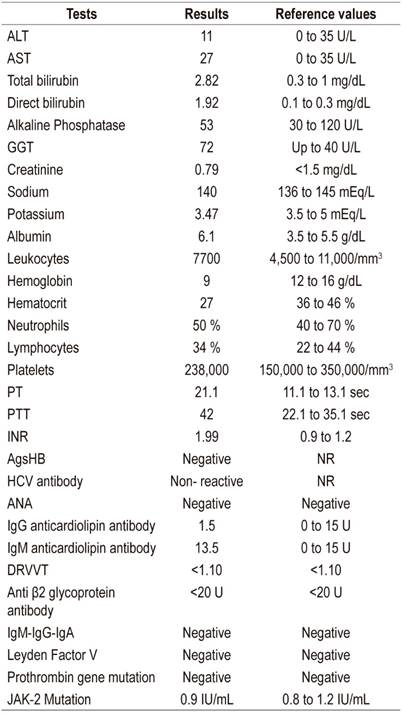
HCV: hepatitis C virus; AgsHB: hepatitis B virus surface antigen; ALT: alanine aminotransferase; ANA: antinuclear antibodies; AST: aspartate aminotransferase; dRVVT: dilute Russell’s viper venom time; GGT: gamma glutamyl transpeptidase; IgA: immunoglobulin A; IgG: immunoglobulin G; IgM: immunoglobulin M; INR: International Normalized Ratio; NR: not reactive; PT: prothrombin time; PTT: partial thromboplastin time.
The patient’s hepatic hemodynamics were measured, and angiography of the vena cava was performed. Total chronic occlusion of hepatic outflow was found. Blood flow had been diverted through a collateral and hepatic venous pressure gradient (GPVH) of 22 mm Hg with no possibility of management through stenting. Consequently, a 10 x 70 mm Viatorr transjugular intrahepatic portosystemic shunt (TIPS) was placed. This required a 10 x 60 mm proximal stent extension. Angiographic monitoring revealed disappearance of varicose veins, and post-TIPS GPVH was 8 mm Hg (Figure 2). After the procedure, the patient began to progressively improve. Abdominal pain diminished, ascites was brought under control with diuretics, and there was no need to perform paracentesis again. In addition, aminotransferase and bilirubin levels decreased. The patient was discharged with a prescription for anticoagulation with low molecular weight heparins. Two subsequent follow-up examinations found that the patient had no ascites, her hepatomegaly had resolved, and her liver profile was normal. Doppler studies during follow-ups confirmed permeability of the TIPS.
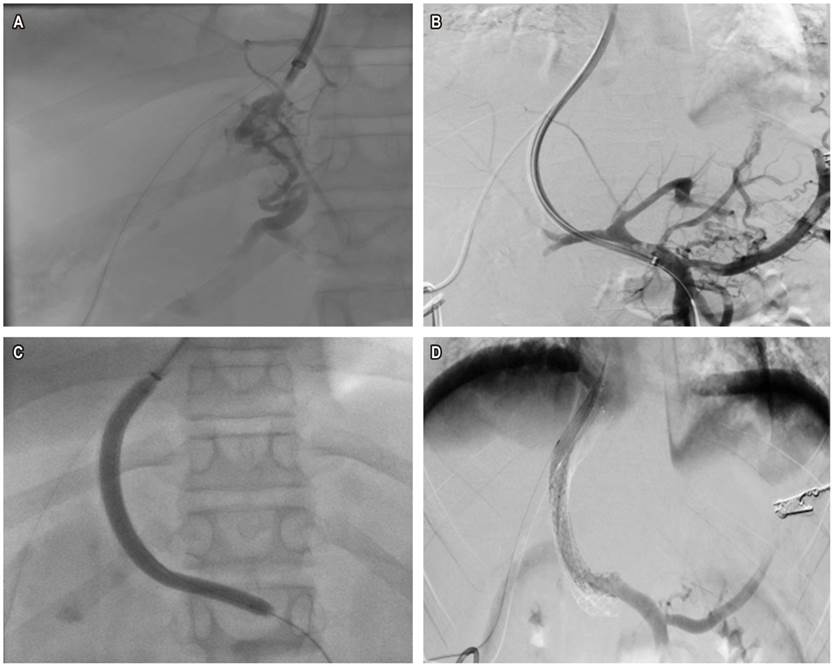
Figure 2 TIPS implant. A. Complete obstruction of suprahepatic veins with collateral flow bypass. B. Permeability of the portal vein and its branches, esophageal varices. C. Balloon dilation of the TIPS path. D. GORE® VIATORR® TIPS Endoprosthesis with proximal extension (10 x 60 mm self-expanding stent), disappearance of esophageal varices.
Discussion
The postpartum period is associated with increased risks of thrombotic events. 9 Although the puerperium is currently definition as the six weeks following delivery, some studies indicate that high risk of thrombosis continues as long as 12 weeks after giving birth. 9 Various studies have reported thrombotic complications such as myocardial infarction, stroke and venous thromboembolism during the puerperium. 10,11,-12) Nevertheless, reports of Budd-Chiari syndrome related to pregnancy and the puerperium are very variable. 8 A recent systematic review that brought together 120 patients with Budd-Chiari syndrome related to pregnancy found the prevalence of this syndrome to be 6.8%. 6 This places pregnancy as a hypercoagulable state with an associated prevalence similar to those of other known risk factors such as the Leiden V mutation, the prothrombin gene G20210A and other types of thrombophilia. Therefore, when the etiology of a case of Budd-Chiari syndrome is evaluated, pregnancy should be considered a risk factor.
The systematic review described brings together patients from 20 countries, predominantly from Asia and Europe. 6 Although the report of this case is important, information about the real prevalence of risk factors for Budd-Chiari in Colombia requires a collaborative study of the referral centers where we patients with hepatic vascular pathologies are evaluated. There are even cultural differences in the management of the puerperium. In India, where reported prevalence of Budd-Chiari syndrome related to pregnancy is as high as 13.1%, occurrence seems to be related both to the puerperal hypercoagulable state and to postpartum rest with limited access to good hydration of between 30 and 40 days. 13 A similar belief still exists in Colombia, especially in rural areas.
Most commonly, the clinical presentation of Budd-Chiari syndrome associated with pregnancy is acute and is due to thrombosis of the suprahepatic veins with obstruction of the outflow tract. 14 This was the case in our patient although the patient consulted late due to social difficulties.
Better understanding of this disease combined with development of new treatments has made it possible to modify the natural history of patients with Budd-Chiari syndrome. Depending on the situation of each particular patient and the hepatic hemodynamics findings, the step-by-step treatment algorithm validated in a number of cohorts proposes initial management with anticoagulation, followed by angioplasty or placement of a stent with thrombolysis, followed by placement of a TIPS. Performance of liver transplantation is necessary in cases of acute liver failure, chronic liver failure or when the Rotterdam score is adverse. 15,16 In the case we have reported, the hemodynamic findings of chronic thrombosis with complete occlusion of the outflow tract indicated placement of a TIPS. Thanks to the availability of this device, decompression of the hepatic outflow tract and clinical recovery were achieved.
Finally, with this case we want to highlight that pregnancy and the puerperium should be understood as hypercoagulable states that are risk factors for hepatic vascular events in this specific population group.
Referencias
1. DeLeve LD, Valla DC, Garcia-Tsao G; American Association for the Study Liver Diseases. Vascular disorders of the liver. Hepatology. 2009 May;49(5):1729-64. https://doi.org/10.1002/hep.22772. [ Links ]
2. Qi X, Han G, Guo X, De Stefano V, Xu K, Lu Z, et al. Review article: the aetiology of primary Budd-Chiari syndrome - differences between the West and China. Aliment Pharmacol Ther. 2016 Dec;44(11-12):1152-1167. https://doi.org/10.1111/apt.13815. [ Links ]
3. Almdal TP, Sørensen TI. Incidence of parenchymal liver diseases in Denmark, 1981 to 1985: analysis of hospitalization registry data. The Danish Association for the Study of the Liver. Hepatology. 1991 Apr;13(4):650-5. https://doi.org/10.1016/0270-9139(91)92559-Q. [ Links ]
4. Okuda H, Yamagata H, Obata H, Iwata H, Sasaki R, Imai F, et al. Epidemiological and clinical features of Budd-Chiari syndrome in Japan. J Hepatol. 1995 Jan;22(1):1-9. https://doi.org/10.1016/0168-8278(95)80252-5. [ Links ]
5. Falter HJ. Deep vein thrombosis in pregnancy and the puerperium: a comprehensive review. J Vasc Nurs. 1997 Jun;15(2):58-62. https://doi.org/10.1016/S1062-0303(97)90002-9. [ Links ]
6. Ray JG, Chan WS. Deep vein thrombosis during pregnancy and the puerperium: a meta-analysis of the period of risk and the leg of presentation. Obstet Gynecol Surv. 1999 Apr;54(4):265-71. [ Links ]
7. Mahmoodi BK, Brouwer JL, Ten Kate MK, Lijfering WM, Veeger NJ, Mulder AB, et al. A prospective cohort study on the absolute risks of venous thromboembolism and predictive value of screening asymptomatic relatives of patients with hereditary deficiencies of protein S, protein C or antithrombin. J Thromb Haemost. 2010 Jun;8(6):1193-200. https://doi.org/10.1111/j.1538-7836.2010.03840.x. [ Links ]
8. Ren W, Li X, Jia J, Xia Y, Hu F, Xu Z. Prevalence of Budd-Chiari Syndrome during Pregnancy or Puerperium: A Systematic Review and Meta-Analysis. Gastroenterol Res Pract. 2015;2015:839875. https://doi.org/10.1155/2015/839875. [ Links ]
9. Kamel H, Navi BB, Sriram N, Hovsepian DA, Devereux RB, Elkind MS. Risk of a thrombotic event after the 6-week postpartum period. N Engl J Med. 2014 Apr 3;370(14):1307-15. https://doi.org/10.1056/NEJMoa1311485. [ Links ]
10. Sultan AA, West J, Tata LJ, Fleming KM, Nelson-Piercy C, Grainge MJ. Risk of first venous thromboembolism in and around pregnancy: a population-based cohort study. Br J Haematol. 2012 Feb;156(3):366-73. https://doi.org/10.1111/j.1365-2141.2011.08956.x. [ Links ]
11. James AH, Bushnell CD, Jamison MG, Myers ER. Incidence and risk factors for stroke in pregnancy and the puerperium. Obstet Gynecol. 2005 Sep;106(3):509-16. https://doi.org/10.1097/01.AOG.0000172428.78411.b0. [ Links ]
12. Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR, Melton LJ 3rd. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Ann Intern Med. 2005 Nov 15;143(10):697-706. https://doi.org/10.7326/0003-4819-143-10-200511150-00006. [ Links ]
13. Dilawari JB, Bambery P, Chawla Y, Kaur U, Bhusnurmath SR, Malhotra HS, et al. Hepatic outflow obstruction (Budd-Chiari syndrome). Experience with 177 patients and a review of the literature. Medicine (Baltimore). 1994 Jan;73(1):21-36. https://doi.org/10.1097/00005792-199401000-00003. [ Links ]
14. Rautou PE, Plessier A, Bernuau J, Denninger MH, Moucari R, Valla D. Pregnancy: a risk factor for Budd-Chiari syndrome? Gut. 2009 Apr;58(4):606-8. https://doi.org/10.1136/gut.2008.167577. [ Links ]
15. Plessier A, Sibert A, Consigny Y, Hakime A, Zappa M, Denninger MH, et al. Aiming at minimal invasiveness as a therapeutic strategy for Budd-Chiari syndrome. Hepatology. 2006 Nov;44(5):1308-16. https://doi.org/10.1002/hep.21354. [ Links ]
16. Seijo S, Plessier A, Hoekstra J, Dell’era A, Mandair D, Rifai K, et al. Good long-term outcome of Budd-Chiari syndrome with a step-wise management. Hepatology. 2013 May;57(5):1962-8. https://doi.org/10.1002/hep.26306. [ Links ]
Received: April 19, 2018; Accepted: May 16, 2018











 text in
text in 


