Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.3 Bogotá July/Sept. 2019
https://doi.org/10.22516/25007440.251
Case report
Transcatheter venous coil embolization of gastric varices
1Radiólogo Intervencionista, Hospital Universitario Fundación Santa Fe, Universidad El Bosque, Bogotá, Colombia.
2Radiólogo, Hospital Universitario Fundación Santa Fe, Universidad El Bosque, Bogotá, Colombia.
3Residente de Cirugía General, Hospital Universitario Fundación Santa Fe, Universidad El Bosque, Bogotá, Colombia.
Coils and microcoils, the most commonly used embolization agents, have reported technical success rates ranging from 81% to 100% of cases. The spirals or coils are available in a wide variety of configurations and sizes which fit into vessels of different calibers. They have good radiopacity allowing for accurate release. Coils are the analogue of a surgical arterial ligation, because they produce mechanical occlusion due to their positioning in the vascular lumen. This decreases blood flow while their synthetic fibers have an additional thrombogenic effect.
Case:
We present four cases of coil embolization treatment of gastric varicose veins at our institution. All procedures were successful and had good technical results. We also present a review of the literature.
Keywords: Digestive bleeding; gastric varices; embolization; coils
Los espirales de embolización (coils o microcoils) son los agentes más comúnmente usados, con un éxito técnico reportado en aproximadamente el 81-100 % de los casos. Los espirales o coils se encuentran disponibles en una amplia variedad de configuraciones y tamaños, lo que permite acomodarse a vasos de distintos calibres; además, por su buena radiopacidad, tienen la ventaja de ser liberados con precisión. Los espirales o coils son el análogo de una ligadura arterial quirúrgica, debido a que producen una oclusión mecánica por su posicionamiento en el lumen vascular, lo que disminuye el flujo sanguíneo, y sus fibras sintéticas tienen un efecto trombogénico adicional.
Caso:
presentamos cuatro casos del Hospital Universitario Fundación Santa Fe de pacientes con várices gástricas tratadas satisfactoriamente con embolización transcatéter con coils, los cuales tuvieron un buen resultado técnico; además presentamos una revisión de la literatura.
Palabras clave: Sangrado digestivo; várices gástricas; embolizacion; coils
Introduction
Embolization is the endovascular treatment of choice for acute bleeding of the upper gastrointestinal tract, hepatobiliary bleeding and lower digestive tract bleeding. Superselective arterial catheterization or venous catheterization using a microcatheter with a caliber less than 3 French (F) is generally required. The catheter is advanced coaxially through a diagnostic catheter (usually 5 F) to those distal vascular segments or as close as possible to the site that is bleeding. This technique allows more selective embolization and avoids other vascular territories which decreases the risk of intestinal ischemia. 1,2
Arterial embolization is a feasible treatment of upper gastrointestinal bleeding because it carries no significant risk of ischemia due to the wide network of collateral arteries that supply the upper gastrointestinal tract. The arterial segments proximal and distal to the hemorrhage should be embolized to prevent retrograde irrigation of the artery and new episodes of bleeding. This is known as closing the front and back doors of the bleeding site. 2
Even though some cases of intermittent gastrointestinal bleeding cannot be identified during arteriography, blind embolization of the bleeding vessels is possible. Due to the rich vascular irrigation of the upper gastrointestinal tract, the segment where the bleeding is probably located can be guessed and targeted. It has been reported that this type of empirical embolization can be performed in up to 46% of all cases, and it has been shown that there are no statistically significant differences in the clinical outcomes of these patients. 2,3,4. It is even possible to embolize branches of the hepatic artery without a significant ischemic risk due to dual irrigation of the liver (75% through the portal vein and 25% through the hepatic artery). 2
For 25 years gastric varices have also been managed with balloon-occluded retrograde transvenous obliteration (BRTO) which requires a sclerosing agent and a permanent balloon to retain the sclerosing agent in the gastric varice, to prevent it from going into systemic circulation, and to optimize the sclerosis of the vessels causing local early thrombosis. Numerous variables involved in this technique have been described. In fact, variations of it do not require balloon occlusion which can be replaced with a wide variety of embolization materials. Nevertheless, there is no conclusive evidence showing that any single embolization agent is better than the others. In practice, use of these techniques depends on the experience and preference of the operator and the availability of the product. The most commonly used embolic agents are spirals or coils. Others include absorbable gelatin sponges (Gelfoam®), particles and liquid embolic agents. 2,5
Embolization spirals (coils or microcoils) have reported technical success rates ranging from 81% to 100% of cases. Coils are available in a wide variety of configurations and sizes that can be used in different calibers vessels. Because they have good radiopacity, they can be released accurately. These coils are the analogues of surgical arterial ligation because they produce mechanical occlusion due to positioning in the vascular lumen which decreases blood flow. In addition, their synthetic fibers provide a thrombogenic effect. 1,5,6
Gelfoam® sponges, polyvinyl alcohol particles, and trisacryl gelatin microspheres have all been used successfully, but controlling their release is more difficult and less precise than controlling coil release. Another disadvantage of embolization particles is that they can reach the blood circulation of the distal intestinal wall which increases the risk of ischemia potentially compromising circulation in vascular territory. To avoid this risk, larger particles measuring more than 500 microns (µ) should be used. Gelfoam® sponges produce temporary occlusion which has the theoretical advantage of allowing recanalization of embolized vessels within two to six weeks. Nevertheless, intestinal ischemia occurs in the first eight to twelve hours after interruption of blood flow, so these sponges have this risk. 1,5,7
Technical success of embolization is close to 100%, and it can satisfactorily control digestive hemorrhaging in 80% to 90% of patients. Recurrent bleeding is uncommon except in cases of angiodysplasia, arteriovenous malformations and inflammatory lesions. It has been reported in approximately 15% of patients. New bleeding episodes may require a second performance of arteriography and embolization, but this does not increase the risk of intestinal ischemia. 1,5,8,9
Major complications related to arterial embolization include intestinal ischemia and contrast-induced nephropathy. Today, clinically relevant ischemic complications occur in less than 2% of patients thanks to the development of microcatheter technology and improvement of embolization materials. Most complications are insignificant and do not require additional treatment. 2,5
In addition, gastric varices’ pathological and hemodynamic characteristics are slightly different from those of esophageal varices. Most gastric varices are secondary to portal hypertension. Other causes include varicose veins secondary to thrombosis of the splenic vein. BRTO is another highly effective minimally invasive procedure for treating isolated gastric varices, especially in patients with poor functional hepatic reserve who are not candidates for TIPS. This technique uses a catheter with a distal balloon that obstructs blood flow during injection of the sclerosant through portosystemic veins (usually a gastrorenal shunt) to adequately fill the varicose veins with enough time for sclerotherapy to be effective while preventing reflux of the sclerosant into the systemic or portal circulation. 2
We replaced the balloon used in BRTO with coils and obtained good results and good bleeding control. We present a series of four cases of control of upper gastrointestinal hemorrhaging due to gastric varices with gastrorenal shunt in our institution that we treated with transcatheter venous embolization with coils. We obtained good technical results and good bleeding control in all four patients.
Case series
First case
This patient was a 74-year-old man who had a history of metastatic hepatocellular carcinoma, cirrhosis, and tumor invasion of the portal vein who came to the hospital after two days of bloody stools. Upper digestive tract endoscopy found small esophageal varices with no signs of bleeding. A subcardial varice was found. It extended approximately 15 mm towards the gastric fundus and had signs of bleeding with red signs at the level. In addition, an ulcerated area on the surface without active bleeding was found. We concluded that the patient had upper digestive bleeding from a large varicose vein in the fundus that was secondary to portal hypertension. Because he was not a candidate for endoscopic management, interventional radiological evaluation was requested. They performed an abdominal CT scan which found tortuous varices adjacent to the lower curvature of the stomach (Figure 1A). Selective venography was used to make the tortuous varices in the lesser curvature, some paraspinal drainage veins, and a gastrorenal shunt opaque. (Figure 1B) Coil embolization (Figure 1C) was used to occlude the flow in the varicose veins. The procedure was performed without complications, and the patient was discharged two days later.
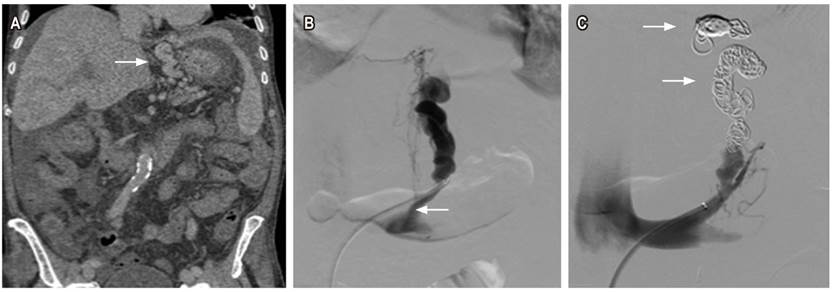
Figure 1 74 year old man. Cirrhosis, gastric varices with gastrorenal shunt. A. Contrast abdominal CT scan shows coronal cut with soft tissue window showing tortuous varices adjacent to the lower curvature of the stomach (arrow). B. Selective venography opacifying tortuous varices in lesser curvature, with some paraspinal drainage veins and gastrorenal shunt (arrow). C. Coil embolization (arrow) occluding the flow in varicose veins.
Second Case
This patient was a 60-year-old man who had previously undergone the Puestow procedure to treat pancreatic neoplasia. He came to the hospital because of melena and anemia with a hemoglobin level of 7 g/dL. Upper endoscopy found blood in the gastric cavity. A large clot was found in the posterior wall of greater curvature of the stomach, but it was not removed because bleeding was observed from the tissue below it. Sclerotherapy with adrenaline solution was performed. An endoscopic follow up examination found two large groups of varices that were not actively bleeding in the fundus of the stomach. Because of their sizes, it was not possible to ligate them, so embolization was required. An abdominal CT scan showed the tortuous varices in the lower curvature of the stomach (Figure 2A). Selective venography was used to opacify the tortuous varices in the lesser curvature and a gastrorenal shunt (Figure 2B). Coil embolization (Figure 2C) was used to occlude the flow of blood in the varicose veins. The procedure was performed without complications, and the patient was discharged the next day.

Figure 2 A 60-year-old man who had undergone pancreatoduodenectomy had developed a hepatic artery pseudoaneurysm with gastric varices and gastrorrenal shunt which were embolized with coils (triangles A, B and C). A. Contrast abdominal tomography shows coronal cut with soft tissue window showing tortuous varices in the lesser curvature of the stomach (arrow). B. Selective venography opacifying tortuous varices in the lesser curvature and gastrorenal shunt (arrow). C. Coil embolization(arrow) occluding the flow in varicose veins.
Third Case
This 66-year-old woman had a history of primary biliary cirrhosis and portal hypertension. She came to the hospital after two episodes of hematemesis. Upper endoscopy found four dilated varices in the distal third of the esophagus occupying 25% of the esophageal lumen. There were no signs or stigmas of recent or old acute bleeding. Remains of old blood were found in the gastric lake, but there was no evidence of active bleeding. A large subcardial varice was found near the greater curvature but there were no stigmas of acute, recent or old bleeding. An abdominal MRI found tortuous varices and a gastrorenal shunt adjacent to the lower curvature of the stomach (Figure 3A). The patient was considered to have a high risk of bleeding, so she required embolization. Selective venography opacified the tortuous varicose vein in the lesser curvature, and the gastrorenal shunt (Figure 3B). Coil embolization(Figure 3C) occluded the flow in the varicose veins. This procedure was performed without complications and the patient was discharged early.

Figure 3 66 year old woman with liver cirrhosis. A. Contrast abdominal magnetic resonance, T1 coronal section with fatty saturation, tortuous varices adjacent to the lower curvature of the stomach and gastrorenal shunt (arrow). B. Selective venography opacifying tortuous varice in the minor curvature and gastrorenal shunt (arrow). C. Coil embolization (arrow) occluding the flow in varicose veins.
Fourth Case
This 69-year-old woman had a history of Child Pugh C alcoholic liver cirrhosis. She came to the hospital because of bleeding esophageal and gastric varices that were difficult to treat endoscopically. The patient required protection of the airway due to the risk of bronchoaspiration, and she received multiple transfusions and vasopressor support. Embolization by way of the route through the abdominal wall and the parenchyma of the liver was considered. An abdominal CT scan showed tortuous varices adjacent to the lower curvature of the stomach (Figure 4A). Selective retrograde portal access venography opacified the tortuous varices in the lower curvature of the stomach (Figure 4B), and coil embolization and Gelfoam® (Figure 4C) were used to occlude the flow of blood through the varices. The procedure was performed without complications and the patient’s bleeding was controlled.
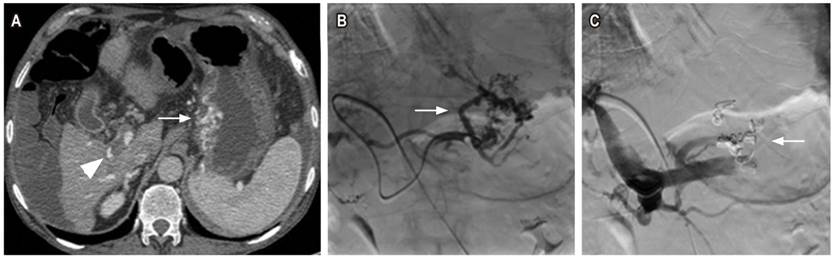
Figure 4 66-year-old woman with liver cirrhosis who was not a candidate for TIPS due to portal thrombosis (triangle A). A. Abdominal CT scan shows axial cut with soft tissue window and tortuous varices adjacent to the lower curvature of the stomach (arrow). B. Selective retrograde portal venography opacifying tortuous varices in the lower curvature of the stomach (arrow). C. Coil embolization (arrow) occluding the flow through varices.
Discussion
Upper gastrointestinal bleeding secondary to gastroesophageal varices is a major complication in patients with cirrhosis and portal hypertension: Its reported incidence is between 4% and 14%. It is increasingly common due to increase number of patients with liver pathologies. In turn, it indicates portal vein hypertension of which cirrhosis is the most frequent cause. 10,11 Varices are the source of approximately 59% of the cases of upper gastrointestinal bleeding in cirrhotic patients. Peptic ulcers, the second leading cause, account for only 16% of cases. 12,13
A gastric varicose vein system is defined as a gastrorrenal shunt, gastric varices in the submucosa, extragastric varices, and the veins, especially the portal vein. Between 60% and 80% of gastric varices are associated with spontaneous portosystemic communication on the left side, including especially gastro-splenic shunts. 14 These have been associated with a higher mortality rate. Endoscopic treatment of them is not always very effective, 12,14 so angiography and embolization of bleeding gastric varices is indicated in these cases. This subgroup of patients requires angiographic intervention to locate the source of the bleeding. Treatment should be done by the endovascular route. 2,5,15,16 For this reason, transcatheter venous coil embolizations were performed on the four patients in this series.
The current technique of coil embolization for treatment of acute gastrointestinal bleeding successfully controls bleeding in approximately 80% to 90% of patients. 8,9 It is a safe technique in which the coil’s fibers cause thrombosis of the vessel while the coil itself functions as a scaffold for the thrombus. Significant adverse events occur in less than 2% of patients. 2 One disadvantage of this mechanism is that it prevents future endovascular access to the specific lesion, but the rates of new hemorrhaging after coil embolization are between 0% and 40%. 6 Some embolized patients very selectively develop minor, asymptomatic and self-limiting ischemic changes such as small ulcers. In addition, very selective coil embolization is unlikely to cause a delayed infarct since this complication typically occurs within the first 48 hours after the embolization procedure. Coil embolization of blood vessels that are not targeted is rare since coils are introduced only after a microcatheter has been successfully inserted into the target vessel. For this reason, one must carefully choose the appropriate coil size since an oversized coil can displace the microcatheter from its superselective position. This could lead to coil deployment in a vessel other than the one chosen for embolization. Similarly, insufficiently large coils may not adequately occlude the target vessel or they may lodge distally to the lesion to be treated thereby decreasing the procedure’s success rates. 5 Nevertheless, because of the large caliber of the left gastric vein and gastric varices combined with the high rate of blood flow through the splenic-renal shunt, some authors such as Ford et al. prefer to oversize coils used in in the venous system by at least 15% to 20% to minimize the probability of migration.17 In our cases there were no major or minor complications during or after transcatheter venous coil embolization, and there were no subsequent migrations of coils.
BRTO is a highly effective, minimally invasive treatment of isolated gastric varices especially for patients with poor functional hepatic reserve who are not candidates for TIPS such as some of our patients. This technique uses a catheter with a distal balloon that obstructs blood flow during injection of the sclerosant through the veins of the portosystemic communication (usually gastrorenal). It allows adequate filling of the varicose veins with enough time for sclerotherapy to be effective while preventing reflux of the sclerosing substance into systemic or portal circulation. 2 Nevertheless, we consider, as do some reviews in the literature, that transcatheter venous coil embolization has tended to replace the BRTO because the logistic load that can wear out the interventional radiology team and increase expenditure of hospital resources. In addition, since replacement of the balloon with coils is technically feasible, 18 we use transcatheter venous coil embolization. To date, we have obtained good results.
Conclusion
Transcatheter venous coil embolization is an effective and safe alternative to emergency surgery in patients with hepatobiliary pathologies for whom surgery could increase morbidity and mortality. Technical advances and increasing availability of diagnostic angiography and transcatheter embolization have strengthened this option for treating bleeding gastric varices that are refractory to medical and endoscopic therapy.
REFERENCES
1. Navuluri R, Kang L, Patel J, Van Ha T. Acute lower gastrointestinal bleeding. Semin Intervent Radiol. 2012 Sep;29(3):178-86. https://doi.org/10.1055/s-0032-1326926. [ Links ]
2. Navuluri R, Patel J, Kang L. Role of interventional radiology in the emergent management of acute upper gastrointestinal bleeding. Semin Intervent Radiol. 2012 Sep;29(3):169-77. https://doi.org/10.1055/s-0032-1326925. [ Links ]
3. Aina R, Oliva VL, Therasse E, Perreault P, Bui BT, Dufresne MP, et al. Arterial embolotherapy for upper gastrointestinal hemorrhage: outcome assessment. J Vasc Interv Radiol. 2001 Feb;12(2):195-200. https://doi.org/10.1016/S1051-0443(07)61825-9. [ Links ]
4. Padia SA, Geisinger MA, Newman JS, Pierce G, Obuchowski NA, Sands MJ. Effectiveness of coil embolization in angiographically detectable versus non-detectable sources of upper gastrointestinal hemorrhage. J Vasc Interv Radiol. 2009 Apr;20(4):461-6. https://doi.org/10.1016/j.jvir.2009.01.006. [ Links ]
5. Walker TG, Salazar GM, Waltman AC. Angiographic evaluation and management of acute gastrointestinal hemorrhage. World J Gastroenterol. 2012 Mar 21;18(11):1191-201. https://doi.org/10.3748/wjg.v18.i11.1191. [ Links ]
6. d’Othée BJ, Surapaneni P, Rabkin D, Nasser I, Clouse M. Microcoil embolization for acute lower gastrointestinal bleeding. Cardiovasc Intervent Radiol. 2006 Jan-Feb;29(1):49-58. https://doi.org/10.1007/s00270-004-0301-4. [ Links ]
7. Abdel-Aal AK, Bag AK, Saddekni S, Hamed MF, Ahmed FY. Endovascular management of nonvariceal upper gastrointestinal hemorrhage. Eur J Gastroenterol Hepatol. 2013 Jul;25(7):755-63. https://doi.org/10.1097/MEG.0b013e32835fb9a9. [ Links ]
8. Patel TH, Cordts PR, Abcarian P, Sawyer MA. Will transcatheter embolotherapy replace surgery in the treatment of gastrointestinal bleeding? (2)(2). Curr Surg. 2001 May;58(3):323-327. https://doi.org/10.1016/S0149-7944(01)00417-2. [ Links ]
9. Schenker MP, Duszak R Jr, Soulen MC, Smith KP, Baum RA, Cope C, et al. Upper gastrointestinal hemorrhage and transcatheter embolotherapy: clinical and technical factors impacting success and survival. J Vasc Interv Radiol. 2001 Nov;12(11):1263-71. https://doi.org/10.1016/S1051-0443(07)61549-8. [ Links ]
10. Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992 Dec;16(6):1343-9. https://doi.org/10.1002/hep.1840160607. [ Links ]
11. Castillo O, Palacios F, Yoza M, Contardo C, Soriano CC. Uso de Cianoacrilato en la Terapia Endoscópica de várices Gástricas: Experiencia en el Hospital Nacional Edgardo Rebagliati Martins del 2006 al 2010. Rev Gastroenterol Perú. 2011;31(3):208-215. [ Links ]
12. Gibson JA, Odze RD. Pathology of diseases that cause upper gastrointestinal tract bleeding. Gastrointest Endosc Clin N Am. 2011 Oct;21(4):583-96. https://doi.org/10.1016/j.giec.2011.07.006. [ Links ]
13. Sostres C, Lanas A. Epidemiology and demographics of upper gastrointestinal bleeding: prevalence, incidence, and mortality. Gastrointest Endosc Clin N Am. 2011 Oct;21(4):567-81. https://doi.org/10.1016/j.giec.2011.07.004. [ Links ]
14. Saad WE. Endovascular management of gastric varices. Clin Liver Dis. 2014 Nov;18(4):829-51. https://doi.org/10.1016/j.cld.2014.07.005. [ Links ]
15. Wee E. Management of nonvariceal upper gastrointestinal bleeding. J Postgrad Med. 2011 Apr-Jun;57(2):161-7. https://doi.org/10.4103/0022-3859.81868. [ Links ]
16. Edelman DA, Sugawa C. Lower gastrointestinal bleeding: a review. Surg Endosc. 2007 Apr;21(4):514-20. https://doi.org/10.1007/s00464-006-9191-7. [ Links ]
17. Ford JM, Shah H, Stecker MS, Namyslowski J. Embolization of large gastric varices using vena cava filter and coils. Cardiovasc Intervent Radiol. 2004 Jul-Aug;27(4):366-9. https://doi.org/10.1007/s00270-004-0071-z. [ Links ]
18. Saad WE, Nicholson DB. Optimizing logistics for balloon-occluded retrograde transvenous obliteration (BRTO) of gastric varices by doing away with the indwelling balloon: concept and techniques. Tech Vasc Interv Radiol. 2013 Jun;16(2):152-7. https://doi.org/10.1053/j.tvir.2013.02.006. [ Links ]
Ethical Approval Informed written consent was obtained from all patients for publication of this document
Received: May 11, 2018; Accepted: June 29, 2018











 text in
text in 


