Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.3 Bogotá jul./set. 2019
https://doi.org/10.22516/25007440.271
Case report
An endoscopic videocapsule finding of heterotopia of the gastric mucosa of the small intestine
1Residente de medicina interna Universidad CES, Fundación valle del Lili. Cali, Colombia
2Médico, Servicio de gastroenterología y endoscopia, Fundación valle del Lili. Cali, Colombia
3Gastroenterólogo, Servicio de gastroenterología y endoscopia, Fundación valle del Lili. Cali, Colombia
4Cirujano gastrointestinal, Servicio de gastroenterología y endoscopia, Fundación valle del Lili. Cali, Colombia
5Patólogo, Servicio de patología, Fundación valle del Lili. Cali, Colombia
Introduction:
Heterotopia of the gastric mucosa refers to an ectopic location of gastric mucosa in any part of the gastrointestinal tract. It is a rare cause of gastrointestinal ulcers and occult digestive bleeding. Endoscopic videocapsules have become fundamental tools for study of the small intestine.
Methods:
This is a descriptive case study based on information from the medical history, pathology report and endoscopic studies extracted from the databases of the Fundación Valle del Lili in Cali, Colombia.
Results:
An endoscopic videocapsule was used to examine a 71-year-old male patient who suffered from occult digestive bleeding. Segments of stenosis and ulcers were found in the jejunum and histopathology revealed heterotopic gastric mucosa.
Conclusion:
Heterotopy of the gastric mucosa should be thought of as a possible cause of bleeding in the small intestine.
Keywords: Gastric heterotopy; occult digestive bleeding; endoscopic videocapsule
Introducción:
la heterotopia de mucosa gástrica se refiere a la localización ectópica de mucosa gástrica en cualquier parte del tracto gastrointestinal. Es una causa poco frecuente de úlceras gastrointestinales y sangrado digestivo oculto. La videocápsula endoscópica se ha convertido en una herramienta fundamental para el estudio del intestino delgado.
Métodos:
estudio descriptivo de reporte de caso. La información de la historia clínica, reporte de patología y estudios endoscópicos, se extrajo de las bases de datos de la Fundación Valle del Lili.
Resultados:
paciente masculino de 71 años, en quien se realizó videocápsula endoscópica por un sangrado digestivo oculto y se encontraron segmentos de estenosis y úlceras en el yeyuno. La histopatología reveló la presencia de mucosa gástrica heterotópica.
Conclusión:
la heterotopia de mucosa gástrica debe considerarse como una causa posible de sangrado del intestino delgado.
Palabras clave: Heterotopia gástrica; sangrado digestivo oculto; videocápsula endoscópica
Introduction
Ulcers rarely occur in the small intestine, but endoscopic techniques such as videocapsules and enteroscopy have allowed this type of lesions to be identified more frequently. Intestinal ulcers can manifest clinically with anemia, episodes of abdominal pain, bleeding, obstruction or perforation. 1 Heterotopic gastric mucosa (HGM), the presence of gastric mucosa in an abnormal location, can cause intestinal ulcers although it is rarely found below the Ligament of Treitz. It is difficult to differentiate heterotopia from gastric metaplasia which is associated with Crohn’s disease. 2
We present the case of the endoscopic videocapsule study of a male patient who had been suffering from digestive bleeding. Multiple ulcers plus stenosis in were found in several of his small intestine. Histological study revealed the presence of pyloric glands with gastric foveolar epithelium.
Clinical case
The patient was a 71-year-old man who had a history of hypertension and diverticular disease. He had been referred to the endoscopy unit of the Fundación Valle del Lili as an outpatient for endoscopic videocapsule diagnosis following two years of abdominal pain, colic and the sensation of a mass in the right iliac fossa that were associated with abdominal distension and episodic constipation alternating with occasional aqueous diarrhea. Paraclinical studies had found fecal occult blood and iron deficiency anemia refractory to administration of ferrous sulfate. He said that he did not use non-steroidal anti-inflammatory drugs (NSAIDs) and said that he was allergic to them. Reports of upper gastrointestinal endoscopy and total colonoscopy conducted elsewhere were normal. He was considered to have digestive bleeding, probably originating in the small intestine.
The patient provided and informed consent and was properly prepared prior to placement of the videocapsule. Erosions and small isolated ulcers were observed in the proximal jejunum. Erosions and deep ulcers with fibrin, retraction of folds, and mucosal edema which appeared to be chronic were found in the middle jejunum together with segments with partial stenoses. The capsule was retained by an ulcerated stenotic lesion in the distal jejunum (Figure 1).
One week after the study, the patient returned with symptoms of an intestinal obstruction. Fluoroscopy documented the capsule in the lower left quadrant of the small intestine. Exploratory laparoscopy found a flange of the omentum causing partial obstruction in the distal ileum of the small intestine. The loop was dilated with thickened and congestive serosa distal to the obstruction. The capsule was trapped in the stenotic segment which required a 6.5 cm resection of the intestine (Figure 2).
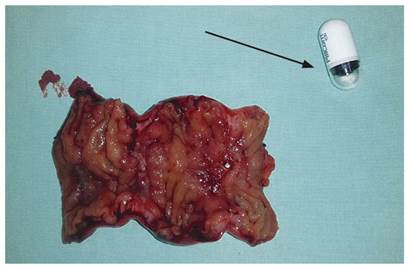
Figure 2 Surgical piece. Stenotic segment of 6.5 cm of small intestine (ileum). Endoscopic videocapsule (arrow).
The surgical piece contained two ulcerated lesions (1.5 cm x 1 cm and 1 cm x 1 cm) which were reported macroscopically. A microscopic examination showed that the small intestine had areas of mucosal ulceration with granulated tissue and fibrin deposits. Foci were found in which foveolar gastric epithelium was observed as well as pyloric glands without cytological atypia in the mucosal and submucosal regions. Inflammatory lymphoplasmocytic infiltrate with formation of hyperplastic lymphoid nodules was observed. Surgical margins had adequate viability. Immunohistochemical PAS (periodic acid-Schiff) staining was used to check for the MUC-5AC mucin marker. The interpretation of the results indicated that neutral mucin was present in the gastric mucosa represented by the foveolar epithelium and the pyloric glands (Figure 3).
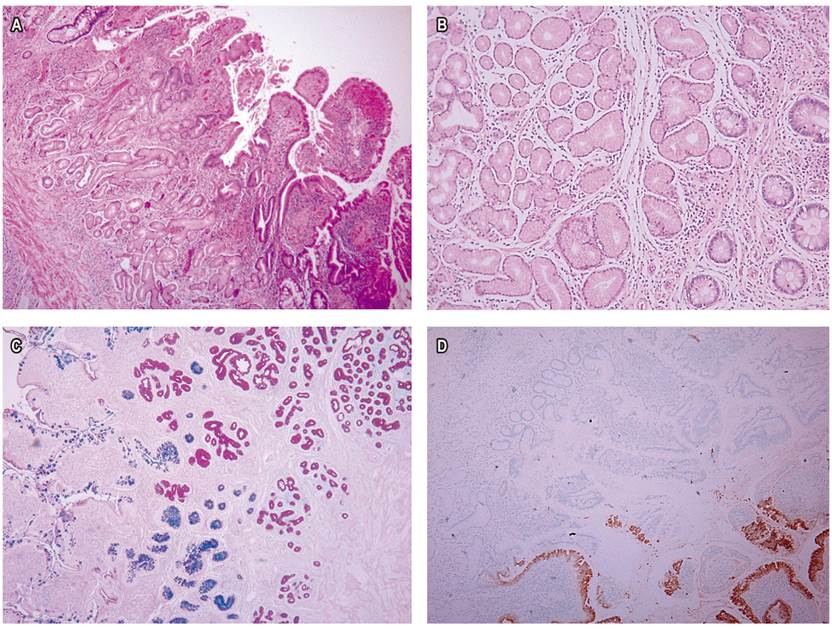
Figure 3 Histopathological study. A. Areas covered by the foveolar gastric epithelium (H-E x 10). B. Pyloric glands in the mucosa and submucosa (H-E x 40). C and D. PAS staining with immunohistochemical study with MUC-5AC showing the presence of neutral mucin of the gastric mucosa represented by the foveolar epithelium and the pyloric glands.
Omeprazole was prescribed for the patient during a postoperative follow-up appointment. Subsequent appointments documented improvement of gastrointestinal symptoms and resolution of anemia. Complementary studies of antineutrophil cytoplasmic antibodies (ANCA), anti-Saccharomyces cerevisiae antibodies (ASCA), rheumatoid factor, the erythrocyte sedimentation rate (ESR) and qualitative C-reactive protein (PCR) tests were done. The rheumatoid factor test was negative while the C-reactive protein (PCR) test was positive. It was decided to continue clinical follow-up with quarterly laboratory tests.
Discussion
The development and use of the endoscopic videocapsule has enabled diagnosis of various lesions in the small intestine that were previously difficult to identify. 3 This study has become a primary tool for evaluating hemorrhagic lesions, ulcers and tumors in this organ. 4 It is currently considered a first-line study for what was previously called occult digestive bleeding, a term that has changed to possible bleeding of the small intestine. This accounts for 5% to 10% of patients who consult for gastrointestinal bleeding. 5,6,7
A study by Pandey et al. of patients who were diagnosed by endoscopic videocapsule has shown that the most frequent causes of bleeding in the small intestine were angiodysplasia in up to 23.5% of these patients, Crohn’s disease in 14.7%, and NSAID enteropathy in 11.76%. Ulcers do not commonly cause bleeding in the small intestine although they have been reported in up to 5.8% of the cases. 8 In general, these ulcers are secondary to Crohn’s disease or NSAID enteropathy and are less frequently associated with entities such as Celiac’s disease, Behcet’s disease, unspecified jejunoileitis, vasculitis, gastrointestinal stromal tumors, intestinal adenocarcinoma, lymphoma, multiple myeloma, Meckel’s diverticulum, infections and HGM. 9
HGM is gastric mucosa in an ectopic location in any part of the gastrointestinal tract. HGM is identified most frequently in the esophagus, followed by the duodenum. 10,12,12) With the exception of Meckel’s diverticulum, locations below the Ligament of Treitz are extremely rare. There are only a few cases of HGM in the jejunum, ileum, colon and rectum in the medical literature. 13,14 Most reports involving the small intestine present asymptomatic patients whose HGMs were identified by histopathological studies of samples obtained surgically. Nevertheless, associated symptoms of gastrointestinal bleeding, 15,16 intussusception, 17 ulceration, perforation and intestinal obstruction have been described. In addition, there are cases in which HGMs have become malignant. 14,18-20 In our patient, the symptoms were abdominal pain and anemia with a bowel obstruction after the endoscopic videocapsule was retained. Findings of multifocal compromises of the small intestine due to several ulcers resulting in various segments of stenosis are very rare situations. There are only two similar cases reported in the literature. One was a 42-year-old patient who had episodes of recurrent abdominal pain, and the other was a 24-year-old patient who had abdominal pain and intestinal perforation. 2,21 Lesions were identified by endoscopic videocapsule in only one case. 14
Two types of HGM have been characterized in relation to histological findings. The first has both gastric glands and gastric foveolar epithelium as in our patient. The second has only gastric foveolar epithelium. It is believed that the former has its origin in a congenital abnormality of the gastrointestinal tract, while the latter could be acquired through a metaplastic process the mechanism of which remains unknown. 11,15,22 There is a possibility that these types of histological lesions are related to Crohn’s disease since outbreaks of pyloric metaplasia have been identified in patients with ileum ulcers and this disease. 23 Koukoulis et al. evaluated 45 biopsies of the terminal ileum of different patients and identified pyloric gland metaplasia in 10 (22.2%) specimens. These findings were observed in patients with terminal ileitis and were located below regeneration crypts and close to granulation and ulceration tissue. No granulomas were observed in any of the pieces. The meaning of this type of lesions is not entirely clear and has been considered a non-specific finding. 24 Agarwal et al. conducted a retrospective study which found that pyloric metaplasia in patients with inflammatory bowel disease who had ileoanal anastomoses with ileal pouches were more likely to have Crohn’s disease than ulcerative colitis. In addition, pyloric metaplasia was associated with postoperative complications such as chronic pouchitis. 25 Although there was not enough evidence to suggest Crohn’s disease in our patient, this possibility cannot be completely ruled out, which makes clinical, paraclinical and imaging follow-up necessary.
Conclusion
Endoscopic videocapsules have made it possible to obtain images of the small intestine that were previously not possible. Heterotopic gastric mucosa is a condition that had traditionally been considered to be congenital, one that very rarely compromised the gastrointestinal tract below the Ligament of Treitz. It is very rare to have a multifocal condition in the small intestine, as in the case of this patient. Distinguishing HGM from pyloric metaplasia is difficult and still remains a point of discussion. This situation requires that patients diagnosed with this condition be strictly monitored clinically, paraclinically and with imaging.
Referencias
1. Fisher L, Scheiman JM. Intestinal Ulcerations. En: Feldman M, Friedman LS, Brandt LJ (editores). Sleisenger and Fordran’s gastrointestinal and liver disease. 10.a edición. Filadelfia: Saunders; 2016. p. 2102-11. [ Links ]
2. Vani M, Nambiar A, Geetha K, Kundil B. Jejunal Gastric Heterotopia causing Multiple Strictures and Perforation Peritonitis- A Case Report with Review of Literature. J Clin Diagn Res. 2017;11(3):ED11-ED12. https://doi.org/10.7860/JCDR/2017/25585.9590. [ Links ]
3. Micic D, Semrad CE. Small Bowel Endoscopy. Curr Treat Options Gastroenterol. 2016;14(2):220-35. https://doi.org/10.1007/s11938-016-0095-x. [ Links ]
4. Ching HL, McAlindon ME, Sidhu R. An update on small bowel endoscopy. Curr Opin Gastroenterol. 2017;33(3):181-8. https://doi.org/10.1097/MOG. 0000000000000346. [ Links ]
5. Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015;110(9):1265-87. https://doi.org/10.1038/ajg.2015.246. [ Links ]
6. Pennazio M, Spada C, Eliakim R, Keuchel M, May A, Mulder CJ, et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2015;47(4):352-76. https://doi.org/10.1055/s-0034-1391855. [ Links ]
7. Gerson LB. Small Bowel Bleeding: Updated Algorithm and Outcomes. Gastrointest Endoscopy Clin N Am. 2017;27(1):171-80. https://doi.org/10.1016/j.giec.2016. 08.010. [ Links ]
8. Pandey V, Ingle M, Pandav N, Parikh P, Patel J, Phadke A, et al. The role of capsule endoscopy in etiological diagnosis and management of obscure gastrointestinal bleeding. Intest Res. 2016;14(1):69-74. https://doi.org/10.5217/ir.2016.14.1.69. [ Links ]
9. Ersoy O, Harmanci O, Aydinli M, Sivri B, Bayraktar Y. Capability of capsule endoscopy in detecting small bowel ulcers. Dig Dis Sci. 2009;54(1):136-41. https://doi.org/10.1007/s10620-008-0320-0. [ Links ]
10. Cooper JE, Roberts-Thomson IC. Gastrointestinal: heterotopic gastric mucosa. J Gastroenterol Hepatol. 2001;16(4):475. [ Links ]
11. Terada T. Heterotopic gastric mucosa of the gastrointestinal tract: a histopathologic study of 158 cases. Pathol Res Pract. 2011;207(3):148-50. https://doi.org/10.1016/j.prp.2010.12.004. [ Links ]
12. Yu L, Yang Y, Cui L, Peng L, Sun G. Heterotopic gastric mucosa of the gastrointestinal tract: prevalence, histological features, and clinical characteristics. Scand J Gastroenterol. 2014;49(2):138-44. https://doi.org/10.3109/00365521.2013.860558. [ Links ]
13. Lee SM, Mosenthal WT, Weismann RE. Tumorous heterotopic gastric mucosa in the small intestine. Arch surgery. 1970;100(5):619-22. https://doi.org/10.1001/archsurg.1970.01340230085022. [ Links ]
14. Qiao WG, Zhang LZ, Zhi FC. Tumor-like heterotopic gastric mucosa discovered by wireless capsule endoscopy. J Dig Dis. 2017;18(9):543-4. https://doi.org/10.1111/1751-2980.12464. [ Links ]
15. Tai CM, Chang IW, Wang HP. Heterotopic gastric mucosa of the ileum. Endoscopy. 2015;47(Suppl 1 UCTN):E423. https://doi.org/10.1055/s-0034-1392666. [ Links ]
16. Nawaz K, Graham DY, Fechner RE, Eiband JM. Gastric heterotopia in the ileum with ulceration and chronic bleeding. Gastroenterology. 1974;66(1):113-7. https://doi.org/10.1016/S0016-5085(74)80086-7. [ Links ]
17. Boybeyi O, Karnak I, Güçer S, Orhan D, Senocak ME. Common characteristics of jejunal heterotopic gastric tissue in children: a case report with review of the literature. J Pediatr Surg. 2008;43(7):e19-22. https://doi.org/10.1016/j.jpedsurg.2008.02.072. [ Links ]
18. Martínez A, Decanini-Terán O, Soria-Céspedes D. Polypoid and hyperplastic heterotopic gastric mucosa in the jejunum as a cause of recurrent subocclusive episodes. Ann Gastroenterol. 2013;26(2):184. [ Links ]
19. Abu-Zidan FM, El-Batrawy TM, Khan NH. Ectopic gastric mucosal ulcer of the jejunum without congenital anomaly causing intestinal obstruction. ANZ J Surg. 2018;88(1-2):E99-E100. https://doi.org/10.1111/ans.13318. [ Links ]
20. Chinnery GE, Bernon MM, Banderker MA, Roberts R, Krige JE. Gastric heterotopia causing jejunal ulceration and obstruction. S Afr J Surg. 2013;51(4):146-7. https://doi.org/10.7196/sajs.1735. [ Links ]
21. Houissa-Vuong S, Martin B, Lascar G, Vuong PN. Multiple jejunal strictures caused by gastric heterotopia. Ann Chir. 2001;126(1):70-4. https://doi.org/10.1016/S0003-3944 (00)00461-2. [ Links ]
22. Genta RM, Kinsey RS, Singhal A, Suterwala S. Gastric foveolar metaplasia and gastric heterotopia in the duodenum: no evidence of an etiologic role for Helicobacter pylori. Hum Pathol. 2010;41(11):1593-600. https://doi.org/10.1016/j.humpath.2010.04.010. [ Links ]
23. Kushima R, Borchard F, Hattori T. A new aspect of gastric metaplasia in Crohn’s disease: bidirectional (foveolar and pyloric) differentiation in so-called ‘pyloric metaplasia’ in the ileum. Pathol Int. 1997;47(6):416-9. https://doi.org/10.1111/j.1440-1827.1997.tb04517.x. [ Links ]
24. Koukoulis GK, Ke Y, Henley JD, Cummings OW. Detection of pyloric metaplasia may improve the biopsy diagnosis of Crohn’s ileitis. J Clin Gastroenterol. 2002;34(2):141-3. https://doi.org/10.1097/00004836-200202000-00007. [ Links ]
25. Agarwal S, Stucchi AF, Dendrinos K, Cerda S, O’Brien MJ, Becker JM, et al. Is pyloric gland metaplasia in ileal pouch biopsies a marker for Crohn’s disease? Dig Dis Sci. 2013;58(10):2918-25. https://doi.org/10.1007/s10620-013-2655-4. [ Links ]
Received: June 05, 2018; Accepted: August 13, 2018











 texto em
texto em 



