Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.4 Bogotá Oct./Dec. 2019
https://doi.org/10.22516/25007440.302
Original articles
Sedation for total colonoscopy with propofol administered by non-anesthesiologists
1Docente del departamento quirúrgico de la Universidad de Caldas. Unión de Cirujanos, Manizales, Caldas, Colombia
Introduction:
Colonoscopy is a very precise procedure for diagnosis and treatment of diseases of the colon. It allows visualization of the mucosa of the entire colon and the terminal ileum if the examination is adequate. Classically, anxiolysis or conscious sedation has been used through the administration of benzodiazepines, or benzodiazepines plus opiates. However, the use of propofol as a sedative in digestive endoscopy has been gradually spreading in recent years.
Objective:
This study evaluates the evolution of sedation procedures with propofol administered by non-anesthesiologists for total colonoscopies.
Material and Method:
Patients who underwent total colonoscopy who were sedated with propofol administered by appropriately trainedg non-anesthesiologists were evaluated. Hemodynamic and respiratory behavior were measured. Patients were excluded if they were over II on the American Society of Anesthesiologists Physical Status Classification System.
Results:
Three hundred ninety patients were evaluated, 269 (69%) were women, and 121 (31%) were men. Their average age was 53.1 years. The average dose of propofol used was 2.3 mg/kg. Bradycardia developed in 4.9% of the patients according to the definition used. The average dose of propofol in patients with bradycardia was 1.76 mg/kg.
Conclusion:
The use of propofol by non-anesthesiologists can be considered safe as long as the protocols established for this purpose are followed.
Keywords: Colonoscopy; propofol; endoscopy; conscious sedation
Introducción:
la colonoscopia es un procedimiento de gran precisión en el diagnóstico y tratamiento de las enfermedades del colon, lo que permite visualizar la mucosa de todo el colon y el íleon terminal, si la exploración es adecuada. Clásicamente se ha utilizado ansiólisis o sedación consciente mediante la administración de benzodiacepinas o la asociación de estos fármacos y opiáceos, sin embargo, la utilización de propofol como sedante en endoscopia digestiva se ha ido extendiendo de forma paulatina en los últimos años.
Objetivo:
evaluar la evolución de los procedimientos de sedación con propofol administrado por médicos no anestesiólogos en colonoscopia total.
Material y métodos:
se evaluaron los pacientes programados para colonoscopia total que fueron sedados con propofol administrado por médicos no anestesiólogos, con el entrenamiento apropiado para tal fin, midiendo el comportamiento hemodinámico y respiratorio. Se excluyen los pacientes con ASA (American Society of Anesthesiologists) mayor de II.
Resultados:
se evaluaron 390 pacientes, 269 (69%) mujeres y 121 (31%) hombres, con una edad promedio de 53,1 años. La dosis promedio utilizada de propofol fue de 2,3 mg/kg. El 4,9% de los pacientes presentó bradicardia según la definición utilizada. La dosis promedio de propofol en los pacientes que presentaron bradicardia fue de 1,76 mg/kg.
Conclusión:
la utilización del propofol por médicos no anestesiólogos es un procedimiento que se puede considerar seguro, siempre y cuando se sigan los protocolos establecidos para tal fin.
Palabras clave: Colonoscopia; propofol; endoscopia; sedación consciente
Introduction
Colonoscopy is very precision for diagnosis and treatment of diseases of the colon. It allows visualization of the entire mucosa of the colon and the terminal ileum if the examination is done well. 1 Classically, anxiolysis (minimal sedation) through administration of benzodiazepines or a combination of these drugs with opiates has been used. However, the use of propofol as a sedative has been gradually increasing in digestive endoscopy in recent years. 2 The administration of propofol is directed by an anesthesiologist in most cases, but 82,620 procedures that have used propofol without presence of an anesthesiologist have been reported by endoscopists. The morbidity rate has been 0.19% while the mortality is zero. 3
The objective of this project is to evaluate the behavior of patients during total colonoscopy with the administration of propofol sedation by non-anesthesiologists.
Material and methods
This work was carried out in the diagnostic endoscopy section of the Union of Surgeons in Manizales, Colombia. Patients scheduled for total colonoscopy were evaluated according to protocol and met the inclusion criteria. They were sedated with propofol administered by appropriately trained non-anesthesiologists. Blood oxygen saturation, hemodynamic behavior and respiratory behavior during sedation were all monitored. Patients under 18 years of age and those with ASA (American Society of Anesthesiologists) Physical Status Classifications over II were excluded in accordance with general recommendations for this type of procedure. Intravenous boluses of propofol were administered starting with a 10-30 mg dose and continuing with titrated propofol as needed according to the patient’s response. All patients received at least 3 L/min of oxygen by nasal cannula. A heart rate of less than 50 beats per minute was defined as bradycardia for these procedures. This study was approved by the Institutional Bioethics Committee of the Faculty of Health Sciences of the University of Caldas in Resolution CBCS-023-16 of March 31, 2016.
Results
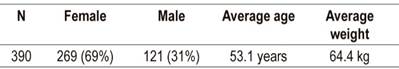
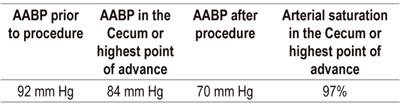
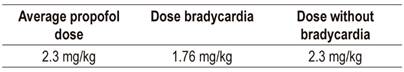
Of the 390 patients evaluated, 269 (69%) were women and 121 (31%) were men. Their average age was 53.1 years, and their average weight was 64.4 kg (Table 1). 70.8% of the patients were ASA I and 29.2% were ASA II. 26.7% of the patients suffered from arterial hypertension, 6.2% had diabetes mellitus, 38.2% had histories of abdominal surgery, 8.2% of the women had had abdominal hysterectomies, 9.5% of the patients were smokers, 8.5% consumed alcohol regularly, and 0.3% consumed other substances (Table 2). The average arterial blood pressure before the procedure was 92 mm Hg, it was 84 mm Hg in the cecum or site of greatest advance, and it was 79 mm Hg after the procedure. The average arterial saturation in the cecum or site of greatest progress was 97% (Table 3). The average dose of propofol used was 2.3 mg/kg (Table 4). Bradycardia (according to the definition used) developed in 4.9% of the patients, and reversal required the use of hyoscine butylbromide although there was no need for atropine or other medications. No relationship was found between bradycardia and ASA I or ASA II classification. The average dose of propofol in patients who presented bradycardia was 1.76 mg/kg, while in those who did not present it was 2.3 mg/kg. The difference was significant (p = 0.012 with statistical power of 99%).
Table 2 Background
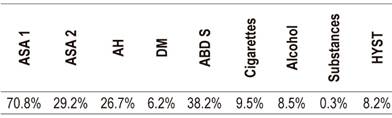
ASA: American Society of Anesthesiologists; ABD S: abdominal surgery; DM: diabetes mellitus; HYST: hysterectomy; AH: arterial hypertension.
Discussion
This study evaluated the hemodynamic and oxygenation behavior of ASA I and ASA II patients during colonoscopies performed with sedation administered by non-anesthesiologists. Although most of the patient were classified as ASA I patients, we found no real differences in blood pressure levels during the procedure and at the different sites evaluated. Similarly, no differences were found in arterial oxygen saturation. When bradycardia developed, it was reversed with hyoscine butylbromide. Bradycardia may be more closely related to the tension on the mesocolon (vagal reflex) than to the dose of propofol used since patients who developed bradycardia had lower doses of propofol. This association was statistically significant.
To facilitate diagnostic and therapeutic procedures, sedation and/or analgesia is commonly used for medical, dental or surgical procedures by a wide range of health professionals with various qualifications and training. 4 The purpose of sedation and analgesia is to reduce anxiety, discomfort and pain and decrease memories of the event. The appropriate level of sedation ranges from minimal sedation to general anesthesia. 5 Patient comfort is an important measure of colonoscopy quality and outcome and has an influence on patient satisfaction and acceptance of a new procedure. 6
Sedation levels range from minimal to moderate sedation to deep sedation and anesthesia. A sedated patient may or may not be awake but maintains an open airway and breathes spontaneously. Similarly, conscious sedation allows communication and response to verbal orders. 7 In general, three types of sedation are used during colonoscopy:
General anesthesia administered by an anesthesiologist
Procedural sedation and analgesia (PSA) administered by an anesthesiologist or a gastroenterologist other than the one performing the colonoscopy
PSA administered by a trained nurse. 8
Sedation schemes that have been used for invasive procedures include these being midazolam with meperidine, midazolam with fentanyl, and midazolam alone. However, these medications have longer durations of action than does propofol. Their side effects include nausea after the procedure, respiratory depression and accumulation in cases of renal failure. 9 Propofol, developed for induction and maintenance of general anesthesia, has rapid onset of action, less nausea and vomiting. and a short recovery time among its greatest advantages. The latter allows rapid exit of a patient from the endoscopy room. 10
Propofol is regularly used for sedation, induction, hypnosis, maintenance, anticonvulsant effect and decreasing the cerebral metabolic rate. It acts nonspecifically on lipid membranes and partially in the inhibitory transmitter system (Gamma aminobutyric acid - GABA). 11 It is classified as an ultra-short-acting hypnotic sedative agent that causes amnesia and minimal levels of analgesia. 12
Injection site pain occurs in more than 30% of patients who receive propofol intravenously. Cardiovascular effects include decreased cardiac output, systemic vascular resistance and blood pressure. Respiratory depression and weakening of cardiac muscular contractions can also occur. 13
Sedation with propofol for colonoscopy has been shown to be superior to other sedation methods because propofol is associated with a low incidence of cardiopulmonary complications and is superior to benzodiazepines with respect to the speed of sedation of induction and recovery. 14
Propofol sedation by nurses under the direction and supervision of the endoscopist who is performing the endoscopic procedure remains controversial due to safety-related concerns about the use of an anesthetic for sedation. 15 Recently it has been shown that propofol can be an effective and safe agent when used by non-anesthesiologists to achieve an adequate level of sedation, and adequate evidence supports its use by non-anesthesiologists due to the rarity of life-threatening episodes. 16 In the absence of another person dedicated solely to monitoring the patient and administering medication, administration of sedation by the endoscopist who performs the endoscopic procedure or the nurse who assists is safe and effective. 17 A disadvantage of propofol is its ability to produce rapid changes in neuropsychological function, from conscious sedation to deep sedation, or even narcosis with respiratory depression and apnea. Another disadvantage is that there is no antagonist. 18
It has been shown that cardiorespiratory complications during colonoscopy may be associated with anesthesia, especially to excessive doses of a drug, inadequate patient monitoring, and/or rapid induction of sedation. 19 A multifaceted specialized training program is needed for individuals who administer propofol. It should include advanced cardiac support and courses designed for this purpose. 20-22 Propofol is one of the medications recommended for sedation grade I and grade II in Colombia. It is recommended by the Colombian Society of Anesthesiology and Resuscitation, the Colombian Association of Gastroenterology and the Colombian Association of Digestive Endoscopy. 23
Conclusion
The use of propofol by non-anesthesiologists can be considered safe for ASA I and ASA II patients as long as the protocols established for this purpose are followed, the person administering the propofol has basic knowledge of the drug and possible complications, and the necessary resources for any untoward eventuality are on hand.
REFERENCES
1. González-Huix L, Figa M, Huertas C. Criterios de calidad que deben exigirse en la indicación y en la realización de la colonoscopia. Gastroenterol Hepatol. 2010;33:33-42. doi: https://doi.org/10.1016/j.gastrohep.2009.02.014. [ Links ]
2. Martínez J, Casellas J, Aparicio J, Garmendia M, Amorós A. Seguridad de la administración de propofol por el personal de la unidad de endoscopia digestiva. Gastroenterol Hepatol. 2007;30:105-9. doi: https://doi.org/10.1157/13100070. [ Links ]
3. Triantafillidis J, Merikas E, Nikolakis D, Papalois A. Sedation in gastrointestinal endoscopy: current issues. World J Gastroenterol. 2013;19:463-81. doi: https://doi.org/10.3748/wjg.v19.i4.463. [ Links ]
4. Baker B, Roessler K, Sutherland J, Tay T. Guidelines on sedation and/or analgesia for diagnostic and interventional medical, dental or surgical procedures. ANZCA PS09 BP. 2014;1-5. [ Links ]
5. Faigel D, Baron T, Goldstein J, Hirota W, Jacobson B, Johanson JF, et al. Guidelines for the use of deep sedation and anesthesia for GI endoscopy. Gastrointest Endosc. 2002;56:613-7. doi: https://doi.org/10.1016/S0016-5107(02)70104-1. [ Links ]
6. Ball AJ, Rees CJ, Corfe BM, Riley SA. Sedation practice and comfort during colonoscopy: lessons learnt from a national screening programme. Eur J Gastroenterol Hepatol. 2015;27:741-6. doi: https://doi.org/10.1097/MEG.0000000000000360. [ Links ]
7. Burtea D, Dimitriu A, Malos A, Saftoiu A. Current role of non-anesthesiologist administered propofol sedation in advanced interventional endoscopy. World J Gastrointest Endosc. 2015;7:981-6. doi: https://doi.org/10.4253/wjge.v7.i10.981. [ Links ]
8. Sporea I, Popescu A, Sandesc D, Salha Ch, Sirli R, Danila M. Sedation during colonoscopy. Rom J Gastroenterol. 2005;14:195-8. [ Links ]
9. Rex DK. Review article: moderate sedation for endoscopy: Sedation regimens for non-anaesthesiologists. Alimen Pharmacol Ther. 2006;24:163-71. doi: https://doi.org/10.1111/j.1365-2036.2006.02986.x. [ Links ]
10. Byrne M, Chiba N, Singh H, Sadowski D. Propofol use for sedation during endoscopy in adults: A Canadian association of gastroenterology position statement. Can J Gastroenterol. 2008;22:457-9. doi: https://doi.org/10.1155/2008/268320. [ Links ]
11. Muñoz-Cuevas JH, de la Cruz-Paz MA, Olivero-Vásquez YI. Propofol ayer y hoy. Rev Mex Anestesiol. 2005;28:148-58. [ Links ]
12. Vargo J, Holub J, Faigel D, Lieberman D, Eisen G. Risk factors for cardiopulmonary events during propofol-mediated upper endoscopy and colonoscopy. Aliment Pharmacol Ther. 2006;24:955-63. doi: https://doi.org/10.1111/j.1365-2036.2006.03099.x. [ Links ]
13. Lichtenstein DR, Jagannath S, Baron T, Anderson M, Banerjee S, Dominitz J. Sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008;68:815-26. doi: https://doi.org/10.1016/j.gie.2008.09.029. [ Links ]
14. Horiuchi A, Nakayama Y, Kajiyama M, Kato N, Kamijima T, Ichise Y, et al. Safety and effectiveness of propofol sedation during and after outpatient colonoscopy. World J Gastroenterol. 2012;18:3420-5. doi: https://doi.org/10.3748/wjg.v18.i26.3420. [ Links ]
15. Ooi M, Thomson A. Morbidity and mortality of endoscopist-directed nurse-administered propofol sedation (EDNAPS) in a tertiary referral center. Endosc Int Open. 2015;3:E393-7. doi: https://doi.org/10.1055/s-0034-1392511. [ Links ]
16. Repici A, Pagano N, Hassan C, Carlino A, Rando G, Strangio G. Balanced propofol sedation administered by nonanesthesiologists: the first Italian experience. World J Gastroenterol. 2011;17:3818-23. doi: https://doi.org/10.3748/wjg.v17.i33.3818. [ Links ]
17. Sáenz-López S, Rodríguez Muñoz S, Rodríguez-Alcalde D, Franco A, Marín JC, de la Cruz J, et al. Endoscopist controlled administration of propofol: an effective and safe method of sedation in endoscopic procedures. Rev Esp Enferm Dig. 2006;98:25-35. doi: https://doi.org/10.4321/S1130-01082006000100004. [ Links ]
18. Sieg A. Propofol sedation in outpatient colonoscopy by trained practice nurses supervised by the gastroenterologist: a prospective evaluation of over 3000 cases. Z Gastroenterol. 2007;45:697-701. doi: https://doi.org/10.1055/s-2007-963349. [ Links ]
19. Cardin F, Minicuci N, Campigotto F, Andreotti A, Granziaera E, Donà B, et al. Difficult colonoscopies in the propofol era. BMC Surg. 2012;12(S9). doi: https://doi.org/10.1186/1471-2482-12-S1-S9. [ Links ]
20. Vargo J, Cohen L, Rex DK, Kwo PY. Position statement: nonanesthesiologist administration of propofol for GI endoscopy. Gastrointest Endosc. 2009;70:1053-9. doi: https://doi.org/10.1016/j.gie.2009.07.020. [ Links ]
21. Morse J, Fowler S, Morse A. Endoscopist-administered propofol: a retrospective safety study. Can J Gastroenterol. 2008;22:617-20. doi: https://doi.org/10.1155/2008/265465. [ Links ]
22. Dumonceau J, Riphaus A, Beilenhoff U, Vilmann P, Hornslet P, Aparicio J. European curriculum for sedation training in gastrointestinal endoscopy: position statement of the European Society of Gastrointestinal Endoscopy (ESGE). Endoscopy. 2013;45(3):496-504. doi: https://doi.org/10.1055/s-0033-1344142. [ Links ]
23. Ibarra P, Galindo M, Molano A, Niño C, Rubiano A, Echeverry P. Recomendaciones para la sedación y la analgesia por médicos no anestesiólogos y odontólogos de pacientes mayores de 12 años. Rev Colomb Anestesiol. 2012:40:67-74. doi: https://doi.org/10.1016/S2256-2087(12)40012-8. [ Links ]
Received: October 08, 2018; Accepted: July 23, 2019











 text in
text in