Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.4 Bogotá oct./dic. 2019
https://doi.org/10.22516/25007440.411
Review articles
How to perform and interpret high resolution anorectal manometry
1 Gastroenterólogos, Unidad de Gastroenterología Hospital Universitario San Ignacio. Bogotá, Colombia.
2 Fellow Gastroenterología, Pontificia Universidad Javeriana. Bogotá, Colombia.
Anorectal manometry is the most commonly used technique to evaluate anorectal functioning and coordination and detect functional abnormalities of the anal sphincter. In our physiology laboratory we perform approximately 15 high resolution anorectal manometry studies each week. We consider that proper performance and correct interpretation are vitally important. We want to share our high resolution anorectal manometry protocol based on the most relevant literature through this article.
Keywords: High resolution anorectal manometry; dyssynergic defecation; fecal incontinence
La manometría anorrectal es la técnica más utilizada para evaluar la función anorrectal y así detectar las anormalidades funcionales del esfínter anal y de coordinación anorrectal. En nuestro laboratorio de fisiología realizamos aproximadamente 15 estudios de manometría anorrectal de alta resolución a la semana, por lo que consideramos que es de vital importancia realizarlo de forma adecuada y tener una correcta interpretación. Mediante este artículo deseamos compartir nuestro protocolo de realización de manometría anorrectal de alta resolución con base en la literatura más relevante.
Palabras clave: Manometría anorrectal de alta resolución; disinergia defecatoria; incontinencia fecal
Introduction
High resolution anorectal manometry is an essential tool for evaluating functional anorectal disorders. From 10% to 25% of the population in developed countries has functional anorectal abnormalities. It is estimated that this figure is on the rise due increases in the elderly population. 1 Functional anorectal disorders are diagnostically challenging since some patients do not seek medical help and correct and complete evaluation of anorectal functioning is essential for proper diagnosis and management. A clinical history considering the Rome IV criteria is important as is knowledge of the clinical utility of diagnostic support studies. High-resolution anorectal manometry records circumferential pressure points through sensors assembled on a flexible probe. Information is presented topographically by colors using averages of the different circumferential pressures. This allows measurement of sphincter and rectal pressures. 2 These pressures are identified during rest, during contraction maneuvers, and during simulated defecation. The percentage of anal relaxation is measured to identify patterns of dyssynergic defecation. This article uses the best available evidence to discuss the procedure in detail and explain how results should be interpreted.
High resolution anorectal manometry (HR-ARM) with complementary studies such as magnetic resonance defecography, fluoroscopic defecography, endoscopic anal ultrasound, and anal sphincter electromyography is recommended for evaluation of anorectal disorders. 3 It is indicated for evaluating fecal incontinence, constipation, functional anorectal pain, before and after anorectal surgery and for functional defecation disorders. 4
To arrive at accurate diagnoses according to patients’ medical histories, the diagnostic principles of defecation disorders as described in the Rome IV criteria are essential, and the effects of age and body mass index on anorectal functions should be considered. 5 Studies by Brochard et al. and Ellington et al. have found that the resting pressure of the anal sphincters of obese people is higher than those of people who have normal weight and those who are overweight. Adipose tissue can increase the thickness of anal sphincters and consequently increase their resting pressures. 6,7
Anorectal manometry can identify abnormal motor, sensory and reflex patterns in patients with incontinence and constipation. These patterns suggest physiological differences which can predict the potentials of different treatments. Otto et al. have demonstrated the reproducibility of anorectal manometry in healthy volunteers and patients. They found a high intra-individual correlation between the pressure of the contraction maneuver and simulated defecation, and between the resting pressure of the anal sphincter and sensitivity. 8
The reproducibility of sphincter pressure at the time of contraction has been a point of controversy. This is considered the parameter that needs the most cooperation from the person undergoing the exam. This factor is considered to have contributed to the poor reproducibility found in some studies. 9,10
Motility laboratories
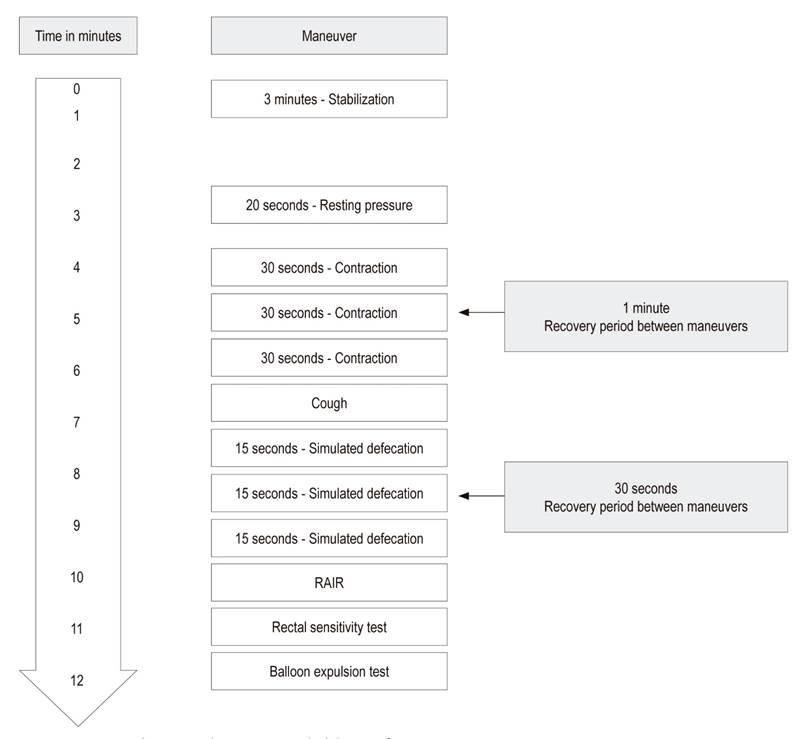
In addition to trained personnel, adequate space that provides patient privacy in an area with the appropriate equipment and a large enough space for performance of HR-ARM is essential (Figure 1).

Figure 1 Gastrointestinal motility laboratory. A. Procedure table B. Manoscan™ Eso High Resolution Manometry System C. Defecation simulation chair D. Cybermed Biofeedback
There are various systems with high resolution, high-definition catheters with circumferential pressure sensors along the longitudinal axis (Figure 2). Pressure sensing elements vary among these systems. Two versions of solid state pressure catheter (ManoScan Catheter AR) with external diameters of 4.2 mm are available. One probe has 12 circumferential pressure sensors: 10 sensors at 6 mm intervals along the anal canal and two sensors in the rectal balloon. The other has 8 circumferential sensors including one in the balloon. The manufacturer recommends using a 3.3 cm long latex-free rectal balloon with a maximum insufflation capacity of 400 mL. The catheter is guaranteed for 200 uses, so care and handling of these probes must be done by trained personnel. Pressure sensors are affected by differences in body and environmental temperatures. The software contains a thermal compensation algorithm to correct this phenomenon.
HR-ARM can be performed by physicians or nurses. For best results, the physician or nurses must know how to adequately prepare patients and must be able to convey a clear and reliable explanation to the patient.
Technique
Patient Preparation
The patient is asked to avoid muscle relaxants and anticholinergic agents prior to the procedure, but is not required to fast. The patient is instructed to take two enemas, the first on the night before the study, and the second two hours before the study.
Positioning
The study must be carried out in a comfortable, private space that is exclusively set aside for the exam. The patient is asked to place herself or himself in left lateral recumbency with the knees bent. The perianal region is inspected to identify fissures, fistulas, wounds and hemorrhoids. Then, the rectal examination verifies adequate preparation of the patient which facilitates introduction of the catheter and anorectal anatomical evaluation. The lubricated probe is gently inserted 14 centimeters into the rectum. The probe is oriented with its dorsal side towards the posterior wall of the patient. This orientation allows detailed reading of the measurements of the rectum and the anal canal.
At Rest Pressure
After placement of the probe, the patient should be allowed to relax for approximately 3-5 minutes, so that the tone of the anal sphincter returns to baseline levels. Anal resting pressure is usually measured for 20 seconds. Ultra slow waves with frequencies of 1.0 to 1.5 cycles/min which are associated with normal or increased anal rest pressures can then be identified.
Voluntary Contraction
The patient is asked to squeeze the anus as hard as possible for a maximum of 30 seconds, followed by a one minute break. By convention, this maneuver is performed 3 times. It is important to continuously monitor the probe assembly and to be aware of any movement of the probe, especially after the patient performs maneuvers such as tightening, coughing or pressing. The probe should be adjusted when necessary.
Simulated Defecation Maneuver
The patient is asked to push as if defecating. This test is performed using distension of a 50 mL rectal balloon with each push separated from the previous one by an interval of 30 seconds. It is essential to instruct patients not to try to retain the catheter. In fact, training patients while performing maneuvers improves the accuracy of the test.
To simulate a physiological defecation position, the subject is asked to sit in a chair with the HR-ARM catheter in position. A container is placed under the chair to catch the balloon, the probe and any other contents that may be accidentally ejected. The rectal balloon is inflated with 50 mL of air. Then, the subject is asked to sit in the chair and push for 30 seconds, as if he were trying to evacuate. The subject is placed back in bed and the manometry probe is removed.
Rectal Sensitivity
This maneuver consists of intermittent distension of the balloon in the rectum to assess rectal sensitivity and the rectoanal inhibitory reflex (RAIR). Prior to this test, the patient is told to report the moment of the first sensation, discomfort and urgency to evacuate.
The test starts with a balloon volume of 10 mL. The balloon is inflated in increments of 10 mL until the first sensation is reported or until balloon volume reaches 60 mL. Then, the balloon is inflated in steps of 30 mL to a maximum of 320 mL or until the maximum tolerated volume is reached (usually 400 mL).
Rectoanal inhibitory reflex (RAIR)
The RAIR should be tested by inflating the balloon at a rate of 30 mL/s and assessing its presence at 20, 40 and 60 mL. If the reflex is absent, the operator must ensure that there is no fecal impaction. If there is none, the balloon should continue to be inflated in increments of 60 mL to a maximum of 240 mL, recording values when the reflex is observed. (11)
Balloon Expulsion Test
The balloon expulsion test, performed on patients with constipation, has proven its usefulness for diagnosis of defecation disorders with a specificity of 86% and sensitivity of 73.9% for identification of defecation dyssynergia. Studies suggest that the best patient position for this maneuver is in the chair that simulates a toilet. 12
The balloon is inflated to 50 mL, and the patient is asked to push for a maximum of three minutes or until the balloon is expelled. The time required for expulsion is recorded. Failure to expel the balloon within the one minute is considered abnormal (obstruction to the outflow tract or dyssynergia).
Analysis and interpretation of anorectal parameters
At Rest Pressure
The internal anal sphincter (IAS) maintains approximately 55% of the anal tone at rest and the external anal sphincter (EAS) maintains approximately 30% of the anal tone at rest. The other 15% is generated by the hemorrhoidal plexus. 7 The basal pressure of the anal sphincter varies according to the sex and age of the patient. Various studies have identified that the at rest pressure is lower in women than in men, and that at it decreases in both men and women as they age. When base pressures are low, the diagnosis is hypotonia of the internal anal sphincter. This diagnosis is useful if the patient presents constipation and may suggest smooth or striated muscle spasms. It has a sensitivity of 51% and a specificity of 70% for identifying lesions of the internal anal sphincter or the rectal canal (Figure 3). 13
The most recent studies in healthy women under 50 years of age have identified the resting pressure range at 85 +/- 22 mm Hg. For women 50 and over it is 66 +/- 25 mm Hg. In men, the range is 83 +/- 25 mm Hg. 7
Voluntary Contraction
Voluntary contractions primarily reflect the strength of the external anal sphincter and the difference between atmospheric pressure and the highest pressure recorded at any level of the anal canal. The contraction must be performed in such a way that the intra-abdominal pressure does not increase simultaneously. The duration of the contraction is the time during which the subject maintains a contraction or 50% of the maximum pressure of the anal sphincter contraction. If this maneuver is abnormal, the diagnosis is alteration or dysfunction of the external anal sphincter. 4
Evacuation Maneuver (push)
For measurement, two attempts at the push maneuver should be made. The maneuver that most closely resembles a normal push should be used. The defecation index (DI) is defined as the maximum rectal pushing pressure/minimum residual anal pushing pressure.
In normal subjects, the push increases rectal pressure while decreasing anal sphincter pressure. A defecation index over 1.2 is considered normal. Inability to perform this coordinated maneuver indicates dyssynergia or a functional obstruction of the passage of the fecal bolus. 4
The proportion of abnormal defecation findings was 47% for dyssynergic manometry patterns and 52.9% for dyssynergic ultrasonography patterns. Four reproducible patterns have been defined although others may exist although none have been confirmed. 14 We consider normal the push maneuver to be normal when anal relaxation is greater than 20% and rectal pressure is greater than 40 mm Hg.
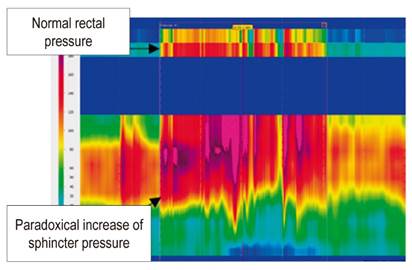
Dyssynergic defecation Type 1
The subject is capable of generating rectal pressure measuring over 40 mm Hg and adequate pushing force, but with no anal relaxation. Instead, there is a paradoxical increase in anal sphincter pressure (Figure 4).
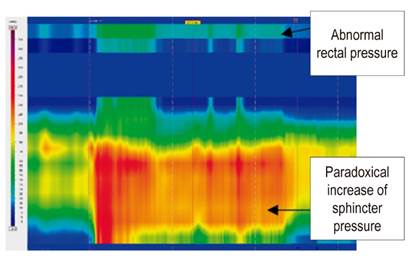
Dyssynergic defecation Type 2
The subject is unable to generate adequate pushing force and presents paradoxical increase in anal sphincter pressure (Figure 5).
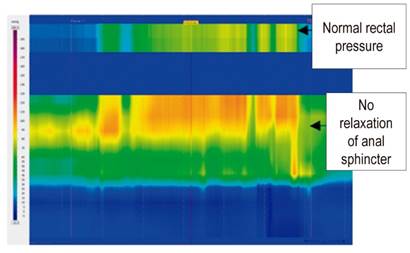
Dyssynergic defecation Type 3
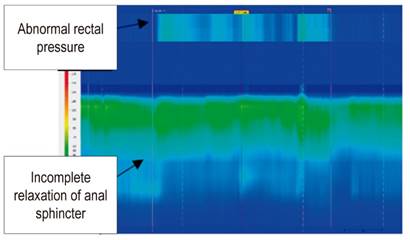
The subject is capable of generating adequate pushing force, but has incomplete or absent anal sphincter relaxation (<20%) with insufficient pressure decrease in the anal sphincter (Figure 6).
Dyssynergic defecation Type 4
The subject is unable to generate adequate pushing force and has incomplete or absent anal sphincter relaxation (has a worse response to Biofeedback therapy) (Figure 7).
Rectal Sensitivity
Rectal sensation is assessed by measuring perceptions of rectal distention including the first sensation, discomfort and urgency. Normal measurements of rectal sensation depend on the stiffness and configuration of the rectal balloon. Diminished perception is demonstrated by at least two modalities of rectal sensation (first sensation, urgency of defecation, maximum tolerable volume) and indicates rectal hyposensitivity.
In our physiology laboratory we consider it to be abnormal when the first sensation is achieved at or above 100 mL which indicates alteration of the sensory threshold of rectal hyposensitivity. This is associated with poor prognoses in patients with conditions as varied as diabetes, fecal incontinence and constipation. Two or more lower perception thresholds indicate rectal hypersensitivity including emergency incontinence, proctitis, and irritable bowel syndrome. We consider it to be abnormal when the first sensation is reported at less than 30 mL which indicates sensory threshold e rectal hypersensitivity.
RAIR is the relaxation reflex of the internal anal sphincter in response to rectal distention. It is associated with increased activity of the external anal sphincter which is eliminated by higher volumes of rectal distention. RAIR is modulated by the myenteric plexus of the autonomic nervous system and produced by the release of nitric oxide and vasoactive intestinal polypeptide. The absence of RAIR may indicate Hirschsprung disease, a postcircular myotomy, or anterior lower resection of the rectum. In patients for whom large volumes are needed to identify RAIR, megarectum (300 mL) and Chagas disease (200 mL) should be considered.
Cough Reflex
Coughing induces a reflex response that consists of a rapid increase in intra-abdominal pressure together with increased external anal sphincter pressure. This reflex assesses damage to the sacral reflex arch. Low contraction pressure of the external anal sphincter and a normal cough reflex may reflect an alteration of control of this sphincter, but reduced contraction pressure of the EAS and an abnormal cough reflex suggests a defect in the sacral reflex arch. 13
Our experience reveals a complete medical history of the patient and adequate training of the personnel who perform the procedure and operate the equipment are both essential. Interpretation of the study should always be in accordance with the most recent information in the literature.
REFERENCES
1. Zhao Y, Ren X, Qiao W, Dong L, He S, Yin Y. High-resolution anorectal manometry in the diagnosis of functional defecation disorder in patients with functional constipation: a retrospective cohort study. J Neurogastroenterol Motil. 2019;25(2):250-7. doi: https://doi.org/10.5056/jnm18032. [ Links ]
2. Carrington E, Scott M, Bharucha A, Mion F, Remes-Troche J, Malcolm A, et al. Expert consensus document: advances in the evaluation of anorectal function. Nature Rev Gastroenterol Hepatol. 2018;15:309-22. doi: https://doi.org/10.1038/nrgastro.2018.27. [ Links ]
3. Rao S, Bharucha A, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, et al. Anorectal disorders. Gastroenterology. 2016;150:1430-42. doi: https://doi.org/10.1053/j.gastro.2016.02.009. [ Links ]
4. Tetangco E, Yan Y, Rao S. Performing and analyzing high-resolution anorectal manometry. NeuroGastroLatam Reviews Rev. 2018;2:1-13. doi: https://doi.org/10.24875/NGL.19000016. [ Links ]
5. Oblizajek N, Gandhi S, Sharma M, Chakrabortv S, Muthyala A, Prichard D, et al. Anorectal pressures measured with high‐resolution manometry in healthy people-Normal values and asymptomatic pelvic floor dysfunction. Neurogastroenterol Motil. 2019;e13597. doi: https://doi.org/10.1111/nmo.13597. [ Links ]
6. Brochard C, Vénara A, Bodère A, Ropert A, Bouguen G, Siproudhis L. Pathophysiology of fecal incontinence in obese patients: a prospective case-matched study of 201 patients. Neurogastroenterol Motil. 2017;00:e13051. doi: https://doi.org/10.1111/nmo.13051. [ Links ]
7. Ellington D, Polin M, Szychowski J, Deng L, Richter H. The effect of obesity on fecal incontinence symptom distress, quality of life, and diagnostic testing measures in women. Int Urogynecology J. 2013;24:1733-8. doi: https://10.1007/s00192-013-2103-1. [ Links ]
8. Otto S, Clewing J, Gröne J, Buhr H, Kroesen A. Repeatability of anorectal manometry in healthy volunteers and patients. J Surg Res. 2013;185(2):e85-92. doi: http://dx.doi.org/10.1016/j.jss.2013.06.008. [ Links ]
9. Rogers J, Laurberg S, Misiewicz J. Anorectal physiology validated: a repeatability study of the motor and sensory tests of anorectal function. Br J Surg. 1989;76:607. doi: https://doi.org/10.1002/bjs.1800760628. [ Links ]
10. Ryhammer A, Laurberg S, Hermann A. Test-retest repeatability of anorectal physiology tests in healthy volunteers. Dis Colon Rectum. 1997;40:287-92. doi: https://doi.org/10.1007/BF02050417. [ Links ]
11. Association of Gastrointestinal Physiologists. Agreed AGIP Guidelines for High-Resolution Anorectal Manometry (HR-ARM). 2017. [ Links ]
12. Seo M, Joo S, Jung KW, Song EM, Rao SSC, Myung SJ. New metrics in high-resolution and high-definition anorectal manometry. Curr Gastroenterol Rep. 2018;20(12):57. doi: https://doi.org/10.1007/s11894-018-0662-5. [ Links ]
13. Tae L, Bharucha A. How to perform and interpret a high-resolution anorectal manometry test. J Neurogastroenterol Motil. 2016;22(1):46-59. doi: http://dx.doi.org/10.5056/jnm15168. [ Links ]
14. Carrington E, Heinrich H, Knowles C, Rao S, Fox M, Scott S, et al. Methods of anorectal manometry vary widely in clinical practice: results from an international survey. Neurogastroenterol Motil. 2017;29(8):e13016. doi: 10.1111/nmo.13016. [ Links ]
Received: June 13, 2019; Accepted: August 15, 2019











 texto en
texto en