Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.1 Bogotá Jan./Mar. 2020
https://doi.org/10.22516/25007440.454
Original articles
Educational models for learning Peroral Endoscopic Myotomy (POEM) and Endoscopic Ultrasound Elastography
1Médico internista y gastroenterólogo. Unidad de gastroenterología y ecoendoscopia, UGEC. Hospital Universitario Nacional. Profesor de Medicina, Universidad Nacional de Colombia. Bogotá, Colombia
2Médico internista y gastroenterólogo. Unidad de gastroenterología y ecoendoscopia, UGEC. Hospital Universitario Nacional. Profesor de Medicina, Universidad Nacional de Colombia. Bogotá, Colombia
3Médico internista. Fellow de gastroenterología, Universidad Nacional de Colombia. Hospital Universitario Nacional. Bogotá, Colombia
Objectives:
This article presents the development of educational models for learning two widespread recent endoscopic techniques which have great clinical implications. Its sole intention is to allow acquisition of basic and advanced skills by residents and gastroenterologists.
Materials and methods:
Two simple, very low cost, easily reproducible and reusable models were devised. Procedures are fully described in ways that allow the operator to integrate the development of skills and acquisition of the minimum theoretical concepts required without the pressures generated by risks of complications.
Results:
The current global trend is to develop teaching models that accelerate the learning curve for highly demanding procedures that are associated with potentially serious complications. With these models it is possible to test endoscopists through continuous supervised evaluations. Implementation by gastroenterology units can be done easily without the need for large investments or travel to other countries.
Conclusions:
This is a great contribution to the scientific and educational development of Colombia since neither development of new endoscopic techniques nor the process of learning how to perform them should put patients at risk. We agree with the ideas of numerous medical associations regarding theoretical-practical courses of short duration even though some virtual sessions, “do not constitute the minimum training required needed for accreditation”.
Keywords: POEM; elastography; echoendoscopy; achalasia; cystic lesions; solid tumors
Objetivos:
presentar el desarrollo de modelos educativos para el aprendizaje de dos técnicas endoscópicas vigentes, ampliamente difundidas y de gran implicación clínica, con la única intención de permitir la adquisición de destrezas básicas y avanzadas a residentes y gastroenterólogos.
Materiales y métodos:
se idearon dos modelos sencillos, de muy bajo costo, fácilmente reproducibles y reutilizables, con los cuales se logra ejecutar la totalidad de los procedimientos descritos. Además, permiten al operador integrar el desarrollo de habilidades y la adquisición de los conceptos teóricos mínimos requeridos, sin las presiones generadas por el riesgo existente de complicaciones.
Resultados:
la tendencia actual a nivel mundial se conduce hacia el desarrollo de modelos de enseñanza que aceleren la curva de aprendizaje, así como de procedimientos altamente exigentes y asociados a complicaciones potencialmente graves. Con estos modelos es posible poner a prueba al endoscopista, mediante una evaluación continua y supervisada. Su implementación en unidades de gastroenterología es sencilla, sin la necesidad de una inversión superlativa o el desplazamiento a otros países.
Conclusiones:
se trata de un gran aporte al desarrollo científico y educativo de nuestro país, ya que la creación y la implementación de nuevas técnicas endoscópicas y su aprendizaje no deben ser asumidos por los pacientes. En este punto, estamos de acuerdo con los conceptos emitidos por diferentes asociaciones médicas respecto a que los cursos teórico-prácticos de corta duración -y en algunas ocasiones virtuales- no constituyen una formación mínima, requerida para lograr la acreditación.
Palabras clave: POEM; elastografía; ecoendoscopia; acalasia; lesiones quísticas; tumores sólidos
Introduction
This article’s aim is to encourage development of educational models based on two extremely interesting and widely used endoscopic techniques. Our objectives are to allow residents and gastroenterologists to acquire basic and advanced skills and to define a systematic evaluation method that contributes to establishing minimum objective requirements for their performance.
In our opinion, implementation of these models is a necessity given that short practical courses do not provide the minimum training required for accreditation in these procedures. On this point, we agree with a great diversity of medical associations.
The explosion of newly developed endoscopic techniques requires continuous exercise of procedural skills which should not be performed on patients since complications derived from malpractice are unacceptable. 1 Therefore, it is urgent to establish structured programs for learning advanced techniques without requirement burdensome investments or travel to other countries. 2,3
Currently available simulators include animal models, biological simulators and virtual simulators. They can be used accelerate the learning curve of training or to maintain competence in those who need retraining after long periods without exercising these skills. 4
A recent opinion of the American Society for Gastrointestinal Endoscopy (ASGE) considers that virtual simulation is inferior to in vivo animal models and simulators with organic parts. 5
Endoscopic myotomy by oral route
Peroral Endoscopic Myotomy (POEM) is a demanding procedure with potentially serious complications. 6 Given its complexity, endoscopy societies worldwide recommend that physicians who have mastered advanced therapeutic procedures should be provided with training strategies that simulate POEM procedural clinical scenarios prior to use on human beings. 7
Multiple models currently being developed can be divided into biological and non-biological. Of these the use of foams, explanted animal esophagi and stomachs, and sedated live animals stand out. 8 Pigs are probably the most appropriate animal model for developing skills and techniques for endoscopic myotomy.
The advantages of pigs include longer esophagi, softer submucosal spaces and distribution of muscle fibers of the variable esophagogastric junction which creates an additional challenge during training. 9
Endoscopic ultrasound elastography
Endoscopic ultrasound (EUS) has modified the work of gastroenterologists by allowing integration of various medical subspecialties. Their interpretation can radically modify the definitive prognosis and treatment of a patient. 10
In Colombia, the use of ultrasound is not yet widely disseminated given the cost of the devices and the fact that the small number of medical centers which have them have not yet acquired the ability to use high quality techniques. 11 The first phase of training specialists in gastroenterology and endoscopy should include the use of learning models so that they can acquire certain skills through supervised practice before intervention patients. This will avoid complications that could arise during this process. 12
The learning curve is long and associated complications are generally severe. Among these complications are perforations, bleeding and infections. 13 Nevertheless, those who perform EUS probably are more afraid that they will make an erroneous diagnosis that directly affects the patient’s condition and indirectly affects the doctor’s well-being.
Thus, learning diagnostic and therapeutic techniques must be ensured without jeopardizing patient safety. 14 One tool developed for this purpose and included in the latest generation ultrasound equipment is quantitative elastography which allows an operator to quickly and practically approximate the structural characteristics of the alterations documented which aids establishment of a probable etiology.
Within this panorama, we have decided to develop an elastographic model that approximates the real practice of quantitative elastography and can aid physicians to assimilate the concepts needed for its adequate implementation. 15
Materials and methods
Preparation and Assembly of the POEM Model
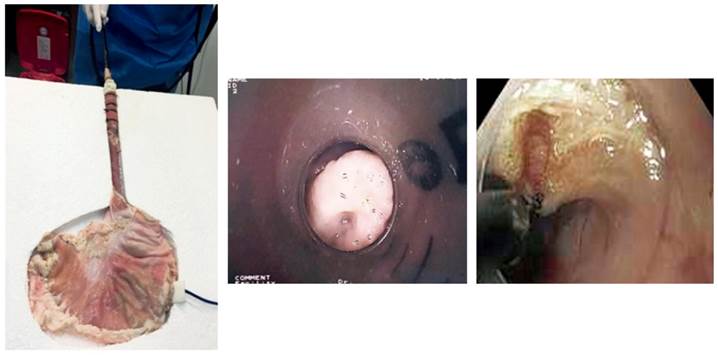
Each copy of this model uses the esophagus, stomach and second duodenal portion extracted a pig. The segment of the esophagus averages 30 cm in length. The extracted organs are washed with saline solution, the food remains are removed, and a small incision is made through the greater curvature order to invaginate the mucosa and achieve better preparation.
Emphasis is then placed on the esophagogastric junction and the subcardial region because of the interest in these work areas and also because we frequently observe that food debris accumulates in this area. Following this, the incisions made in the gastric corpus and the second duodenal portion are closed with continuous stitches to ensure adequate insufflation.
The entire piece is articulated on an expanded polystyrene base which consists of two sheets whose approximate size is 50 x 50 cm. An anatomical cut is made in the upper sheet to match the arrangement and size of the esophagus-stomach segment. Similarly, the electrosurgical unit’s plate is attached to the polystyrene sheet attached to the posterior of the explanted stomach and conductive gel is applied to it.
A modified 20 cm syringe is installed at the proximal end of the esophagus as an overtube to allow the endoscope to advance easily. Plastic clamps are used to fix this syringe in the proximal part of the esophagus. A perforated latex glove is used in the proximal hole of the syringe as a valve to limit air leakage (Figure 1).
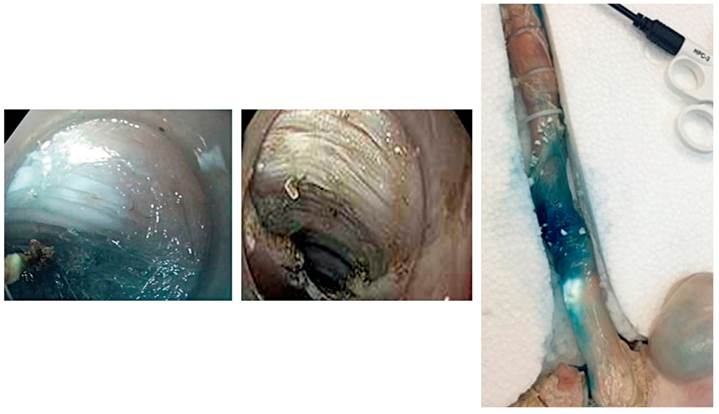
After assembly, supplies required for the procedure are prepared. They include an endoscope, an injection needle, saline solution, indigo carmine, an ERBE model electrosurgical unit using default settings for mucosal disruption and myotomy, coagulation forceps, a triangular-tipped scalpel, and endoclips (Figures 2 and 3).
Description of Procedure
The first step of the procedure is using endoscopy to determine the distance at which the esophagogastric junction is located. Then, just 15 cm before the junction, the procedure begins by elevating the mucosa through injecting saline and indigo carmine.
At this the options of anterior and posterior approaches are discussed to guarantee development of necessary competences given the possibility of multiple anatomical variants in patients with achalasia.
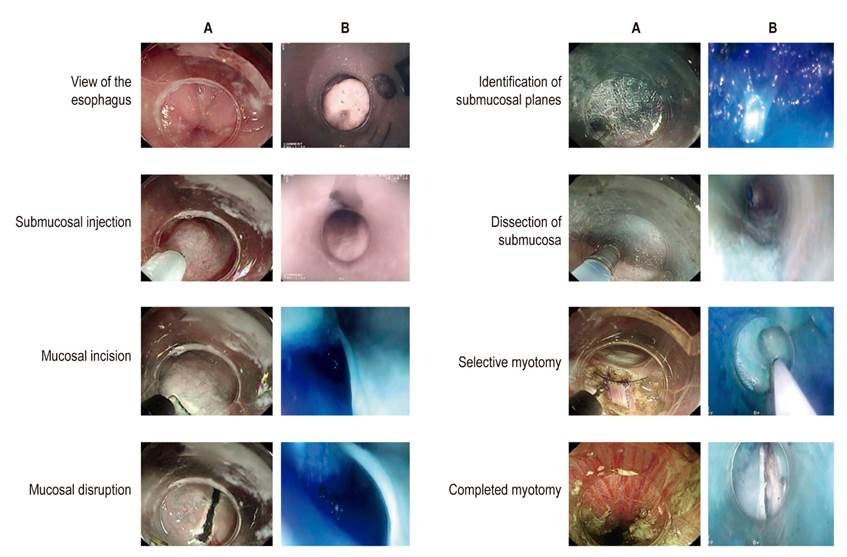
After choosing the desired approach, a 2 cm transverse incision is made in the mucosa. Then, the tip of the endoscope is slid into the submucosal space to create a tunnel using an injection technique and constant dissection (Figure 4).
We have modified the technique because of concern to ensure depth of insertion and because of the multiple techniques described. An additional injection of indigo carmine is made just over the cardia to facilitate identification of the distal end and also to guarantee the desired trajectory with the tunnel. All this can be done without any need for accessory endoscopes or repeated tunnel withdrawals which could extend the initial mucosal cut.
The myotomy of muscle fibers is performed using the technique of lifting and cutting up to 2 cm from the distal mark or the esophagogastric junction. Once the myotomy is completed, the mucosal incision is closed using endoclips (Figure 5). 16
Endoscopic Ultrasound Elastography Model
Elaboration and Assembly
Materials used to create this model included a 5 L plastic container, 400 g of gelatin, 2 L of water, plastic balloons filled with air, water, oil and various objects of different consistencies that are inserted into the model. These objects included rubber balls, grapes, peas and meat cubes. Objects of different consistencies allow for elastographic evaluation.
The 400 g of gelatin and water are mixed in the plastic container. When the mixture solidifies, solid and cystic appearing objects are introduced. After that, the model is left in the refrigerator for at least 12 hours to be used the next morning. After the day of training has ended, it is refrigerated again. It can be used for up to eight days (Figure 6).
Description of Procedure
The procedure begins with radial EUS. Before beginning, a balloon is placed on the tip of the echoendoscope. Piñata balloons which cost less than endoscopic balloons can used in this model. The balloon is then cut at its open end and attached to the transducer with dental floss. Then the echoendoscope is introduced and learning begins. Students must become familiar with the console, demonstrate how image quality can be affected, and learn how to optimize image by using gain, ranges, and contrasts (Figure 7).
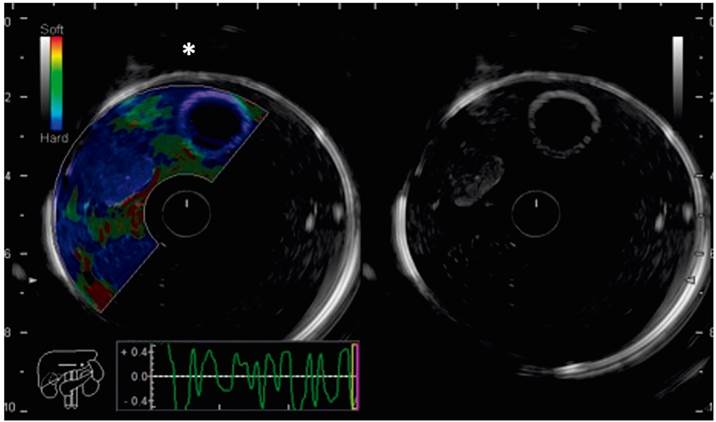
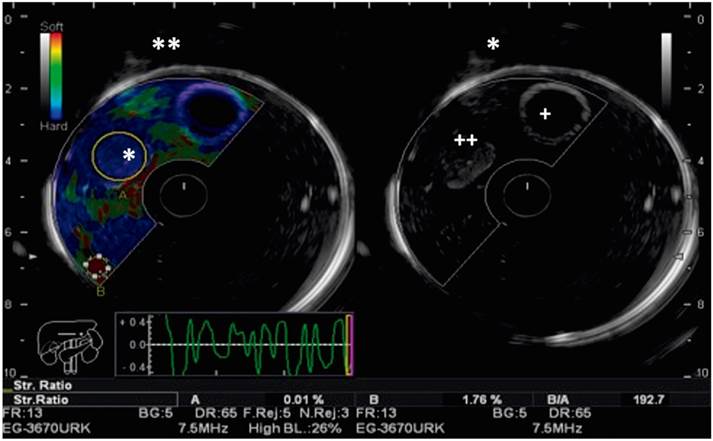
Figure 7 Elastography model and echoendoscopic view. Note the different echogenic characteristics of the cystic and solid lesions on the right. On the left, the cystic lesions have no elastographic pattern (*).
Next, students investigate characteristics of the lesions (previously introduced objects) that they identify and learn about echogenic image qualities from anechoic indicating liquid, through isoechoic, hypoechoic and hyperechoic.
Volume forms (spherical, oval, linear) are also evaluated, and students learn to use the caliper to measure lesions. These instruments allow measurement in two dimensions and calculation of volumes (Figure 8).
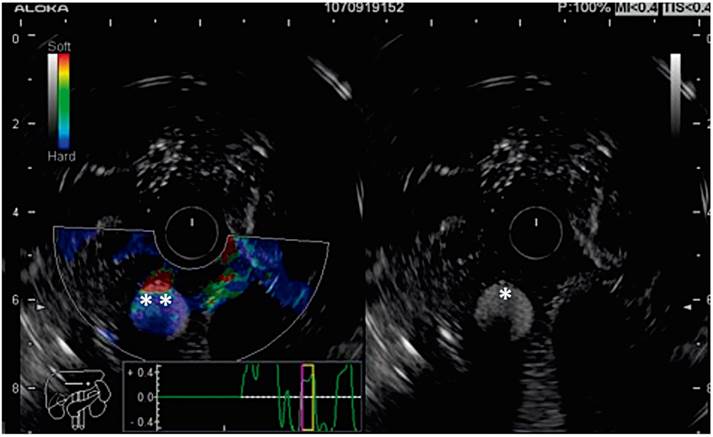
Figure 8 Elastography model and echoendoscopic view: the echogenic characteristics of a solid lesion are shown on the right (*), and its elastographic representation (**) are highlighted on the left.
Once students have been introduced to these skills, it is necessary to switch to linear equipment and to introduce students to the differences between radial and linear equipment. A key difference is that the image of the radial equipment is 360º while the linear equipment’s image is 160º. Other differences include the types of consoles, the use of Doppler, and measurement of images.
Upon achieving complete mastery of these skills, students are trained in the usefulness of elastography for determining parameters related to the structural organization and consistency of tissues and changes in the stiffness of different elements. All this is based on interpretation and calculation of strain ratio and linear histogram which allow approximation of etiology. For example, it allows differentiation between neoplastic and non-neoplastic lesions.
Quantitative elastography is based on measurement of the speed of propagation of transverse shear waves. These waves are produced in the process of tissue compression and recovery to its original shape. 15 They are represented on heat maps that vary from blue which indicates stiffer tissues to red which indicates softer tissues. 17
The strain ratio is the ratio between the average tension measured in a solid lesion and the average tension of a similar area of healthy tissue or of tissue adjacent to the lesion. 18 The difference in deformation reflects the relative stiffness of the lesion, as shown in Figure 9. Various studies have related a stiff strain ratio of more than 20 to malignant lesions. 19,20
Discussion
The creation of a third space, the submucosal tunnel, has generated therapeutic and diagnostic options for various pathologies that have had favorable results. Its uses continue to increase. 21 They include diagnosis of functional esophageal disorders such as achalasia, diffuse esophageal spasms, and disturbances of gastric emptying. In addition, it enables resection of minimally invasive esophagogastric subepithelial tumors. Consequently, it is essential that endoscopists familiarize themselves with his technique to guarantee fewer complications from the intervention. 22
We have intentionally left the second duodenal portion within the model in order to simulate gastric POEM as a treatment for gastroparesis. 23
On the other hand, the endoscopic ultrasound elastography teaching model can be used for learning the basic foundations of this interesting technique in a simple way that guarantees adequate interaction and knowledge of the equipment and each of the console devices. In addition, it fully establishes the identification and details of various radiological characteristics of lesions and accustoms the hand and eye to their detection. 24
This makes it easy for the tutor to choose which the type of lesion is going to be identified in order to design practical lessons using the model. It also makes it possible to develop a continuous evaluation format since although the quickly-learned technique’s conceptual universe is large while clinical correlations contribute to practice and modification of the therapeutic threshold based on elastographic findings. 25 This factor seems fundamental and novel to us given that the concepts excluded from other models have eminently diagnostic purposes only in relation to radiological findings. 26,27,28
Conclusions
The underlying concern regarding the introduction of diagnostic and therapeutic techniques that have high economic, social, prognostic, emotional, and professional impacts is clear. Therefore, it is imperative that professionals who use them are well trained and have sufficient experience.
Although there are other simulators with higher technology, their operating costs makes them unattainable in our environment. For this reason, we consider our contribution to be a fundamental impulse in the development of the skills of gastroenterologists and residents in training.
Educational models like ours are essential in Colombia, since their elaboration has low costs. They are also easily reproducible, allow multiple uses, and guarantee easy access to specialized techniques
Referencias
1. Bisschops R, Wilmer A, Tack J. A survey on gastroenterology training in Europe. Gut. 2002;50(5):724-9. http://dx.doi.org/10.1136/gut.50.5.724 [ Links ]
2. McCashland T, Brand R, Lyden E, de Garmo P. The time and financial impact of training fellows in endoscopy. CORI Research Project. Clinical Outcomes Research Initiative. Am J Gastroenterol. 2000;95(11):3129-32. http://dx.doi.org/10.1111/j.1572-0241.2000.03280.x [ Links ]
3. Bini EJ, Firoozi B, Choung RJ, Ali EM, Osman M, Weinshel EH. Systematic evaluation of complications related to endoscopy in a training setting: A prospective 30-day outcomes study. Gastrointest Endosc. 2003;57(1):8-16. https://doi.org/10.1067/mge.2003.15 [ Links ]
4. Cohen J, Thompson CC. The next generation of endoscopic simulation. Am J Gastroenterol . 2013 Jul;108(7):1036-9. https://doi.org/10.1038/ajg.2012.390 [ Links ]
5. Varadarajulu S, Christein JD, Wilcox M. 298 Endoscopic Transmural Drainage of Pancreatic Fluid Collections (PFCs) in 200 Consecutive Patients: An Assessment of Outcomes. Gastrointest Endosc . 2011;73(4):AB122. https://doi.org/10.1016/j.gie.2011.03.038 [ Links ]
6. AbouHashem Y, Dayal M, Savanah S, Štrkalj G. The application of 3D printing in anatomy education. Med Educ Online. 2015;20:29847. https://doi.org/10.3402/meo.v20.29847 [ Links ]
7. Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Maselli R, Santi G. Submucosal tunnel endoscopy: Peroral endoscopic myotomy and peroral endoscopic tumor resection. World J Gastrointest Endosc . 2016;8(2):86-103. https://doi.org/10.4253/wjge.v8.i2.86 [ Links ]
8. Li QL, Zhou PH. Perspective on peroral endoscopic myotomy for achalasia: Zhongshan experience. Gut Liver. 2015;9(2):152-8. https://doi.org/10.5009/gnl14227 [ Links ]
9. Onimaru M, Inoue H, Ikeda H, Sato C, Sato H, Phalanusitthepha C, et al. Greater curvature myotomy is a safe and effective modified technique in per-oral endoscopic myotomy (with videos). Gastrointest Endosc . 2015;81(6):1370-7. https://doi.org/10.1016/j.gie.2014.11.014 [ Links ]
10. Onimaru M, Inoue H, Ikeda H, Yoshida A, Santi EG, Sato H, et al. Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg. 2013;217(4):598-605. https://doi.org/10.1016/j.jamcollsurg.2013.05.025 [ Links ]
11. Eleftheriadis N, Protopapas A, Katsogridakis J, Hatzitolios AI .Successful peroral endoscopic myotomy for radical treatment of sigmoid-type esophageal achalasia by Greek gastroenterologists. Ann Gastroenterol. 2014;27(4):430-431. [ Links ]
12. Li QL, Chen WF, Zhou PH, Yao LQ, Xu MD, Hu JW, et al. Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg. 2013;217(3):442-51. https://doi.org/10.1016/j.jamcollsurg.2013.04.033 [ Links ]
13. Sedlack RE, Kolars JC. Computer simulator training enhances the competency of gastroenterology fellows at colonoscopy: results of a pilot study. Am J Gastroenterol. 2004;99(1):33-7. https://doi.org/10.1111/j.1572-0241.2004.04007.x [ Links ]
14. Gómez MA. Utilidad de un modelo para el entrenamiento del ultrasonido endoscópico radial y lineal. Rev Col Gastroenterol. 2007;22:104-110. [ Links ]
15. Nightingale K, Bentley R, Trahey G. Observations of tissue response to acoustic radiation force: opportunities for imaging. Ultrason Imaging. 2002;24(3):129-38. https://doi.org/10.1177/016173460202400301 [ Links ]
16. Grimes KL, Inoue H. Per Oral Endoscopic Myotomy for Achalasia: A Detailed Description of the Technique and Review of the Literature. Thorac Surg Clin. 2016;26(2):147-62. https://doi.org/10.1016/j.thorsurg.2015.12.003 [ Links ]
17. Nightingale K, McAleavey S, Trahey G. Shear-wave generation using acoustic radiation force: in vivo and ex vivo results. Ultrasound Med Biol. 2003;29(12):1715-23. https://doi.org/10.1016/j.ultrasmedbio.2003.08.008 [ Links ]
18. Bercoff J, Tanter M, Fink M. Supersonic shear imaging: a new technique for soft tissue elasticity mapping. IEEE Trans Ultrason Ferroelectr Freq Control. 2004;51(4):396-409. https://doi.org/10.1109/TUFFC.2004.1295425 [ Links ]
19. Sandrin L, Fourquet B, Hasquenoph JM, Yon S, Fournier C, Mal F, Christidis C, Ziol M, Poulet B, Kazemi F, Beaugrand M, Palau R. Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol . 2003;29(12):1705-13. https://doi.org/10.1016/j.ultrasmedbio.2003.07.001 [ Links ]
20. Sandrin L, Tanter M, Catheline S, Fink M. Shear modulus imaging with 2-D transient elastography. IEEE Trans Ultrason Ferroelectr Freq Control. 2002;49(4):426-35. https://doi.org/10.1109/58.996560 [ Links ]
21. Harewood GC, Wiersema MJ, Nelson H, Maccarty RL, Olson JE, Clain JE, et al. A prospective, blinded assessment of the impact of preoperative staging on the management of rectal cancer. Gastroenterology. 2002;123(1):24-32. https://doi.org/10.1053/gast.2002.34163 [ Links ]
22. Chang KJ, Nguyen P, Erickson RA, Durbin TE, Katz KD. The clinical utility of endoscopic ultrasound-guided fine-needle aspiration in the diagnosis and staging of pancreatic carcinoma. Gastrointest Endosc. 1997;45(5):387-93. https://doi.org/10.1016/S0016-5107(97)70149-4 [ Links ]
23. Hochberger J, Maiss J, Magdeburg B, Cohen J, Hahn EG. Training simulators and education in gastrointestinal endoscopy: current status and perspectives in 2001. Endoscopy. 2001;33(6):541-9. https://doi.org/10.1055/s-2001-14972 [ Links ]
24. Silver B, Metzger TS, Matalon TA. A simple phantom for learning needle placement for sonographically guided biopsy. AJR Am J Roentgenol. 1990;154(4):847-8. https://doi.org/10.2214/ajr.154.4.2107686 [ Links ]
25. Burmester E, Leineweber T, Hacker S, Tiede U, Hütteroth TH, Höhne KH. EUS Meets Voxel-Man: three-dimensional anatomic animation of linear-array endoscopic ultrasound images. Endoscopy. 2004;36(8):726-30. https://doi.org/10.1055/s-2004-825669 [ Links ]
26. Fusaroli P, Caletti G. Endoscopic ultrasonography. Endoscopy. 2003;35(2):127-35. https://doi.org/10.1055/s-2003-37010 [ Links ]
27. Classen M, Ruppin H. Practical Endoscopy Training Using a New Gastrointestinal Phantom. Endoscopy (1974) 127-131. https://doi.org/10.1055/s-0028-1098609 [ Links ]
28. Qiao W, Bai Y, Lv R, Zhang W, Chen Y, Lei S, et al. The effect of virtual endoscopy simulator training on novices: a systematic review. PLoS One. 2014;9(2):e89224. https://doi.org/10.1371/journal.pone.0089224 [ Links ]
Received: November 26, 2018; Accepted: January 28, 2019











 text in
text in