Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.1 Bogotá jan./mar. 2020
https://doi.org/10.22516/25007440.340
Original articles
Comparison of abdominal pain and distention due to insufflation with CO 2 versus insufflation with air in an advanced digestive endoscopy unit in Manizales, Colombia
1Médico, cirujano general, residente de II año de Gastroenterología Clínica Quirúrgica. Universidad de Caldas, Manizales, Colombia
2Médico, cirujano general, gastroenterólogo clínico quirúrgico, coordinador del programa de Gastroenterología Clínico Quirúrgica, Universidad de Caldas, Manizales, Colombia
Objective:
This study compares the incidence of abdominal pain and distension, the magnitude of pain, abdominal perimeter, and related complications related to two different insufflating agents.
Patients and Method:
Prospective analytical cohort study. Data were collected from 43 performances of endoscopic retrograde cholangiopancreatography (ERCPs) and 20 colonoscopies in which patients were insufflated with CO2. A control examination using ambient air for insufflation was performed for each patient. In total, 86 ERCPs and 40 colonoscopies were performed. The study includes clinical characterizations, bivariate analysis and multivariate analysis.
Results:
The most painful procedure was colonoscopy, but 60% of colonoscopy patients and 70% of ERCP patients had no pain 15 minutes after waking up following their examinations. No statistically significant differences related to reasons for examination, presence or intensity of pain at the time of the procedure, age, sex or diagnosis were found. The relative risk (RR) of immediate pain is 4.8 times higher when insufflation is done with air instead of CO2 (RR = 4.8; 95% CI: 2.3 to 9.2; p <0.001). The risk of abdominal distension in the air group was 2.6 times higher than that of the group insufflated with CO2 (RR = 2.6; 95% CI: 1.8 to 3.9; p <0.001). CO2 reduces the likelihood and extent of abdominal distension and immediate post colonoscopy or ERCP pain. There were no complications in any of the 126 patients.
Conclusions:
Abdominal pain and bloating occur less frequently and less intensely when CO2 is used as an insufflating agent. None of the procedures presented major complications.
Keywords: Colonoscopy; carbon dioxide; endoscopic retrograde cholangiopancreatography; air; abdominal circumference; pain
Objetivo:
comparar la magnitud del dolor y el perímetro abdominal; la incidencia del dolor y la distensión abdominal, y las complicaciones según el agente insuflante utilizado.
Pacientes y método:
estudio prospectivo analítico de cohorte. Se recolectaron datos de 43 colangiopancreatografías retrógradas endoscópicas (CPRE) y 20 colonoscopias insufladas con dióxido de carbono (CO2); para cada una se buscó un examen control con aire ambiente. En total, se sumaron 86 CPRE y 40 colonoscopias. Además, se realizó una caracterización clínica, un análisis bivariado y multivariado.
Resultados:
el procedimiento más doloroso fue la colonoscopia; sin embargo, el 60 % de los pacientes de colonoscopia, y el 70 % de aquellos de CPRE, no presentaron dolor 15 minutos después de haber despertado luego del examen. Asimismo, no se hallaron diferencias estadísticamente significativas según la indicación del examen, la presencia o intensidad de dolor al momento del procedimiento, la edad, el sexo o el diagnóstico. El riesgo relativo (RR) de dolor inmediato fue 4,8 veces superior, cuando la insuflación se realizó con aire en vez de CO2 (RR = 4,8; intervalo de confianza [IC], 95 %: 2,3 a 9,2; p <0,001). Entre tanto, el riesgo de distensión abdominal en el grupo con aire fue 2,6 veces superior, en comparación con el grupo insuflado con CO2 (RR = 2,6; IC, 95 %: 1,8 a 3,9; p <0,001). El CO2 redujo la probabilidad y la magnitud de la distensión abdominal y de los dolores inmediatos, posteriores a la colonoscopia o a la CPRE. No hubo complicaciones en ninguno de los 126 pacientes.
Conclusiones:
el dolor y la distensión abdominal se presentan con menor frecuencia e intensidad cuando se usa CO2 como agente insuflante. Ninguno de los procedimientos presentó complicaciones mayores.
Palabras clave: Colonoscopia; dióxido de carbono; colangiopancreatografía retrógrada endoscópica; aire; circunferencia abdominal; dolor
Introduction
Air insufflation is the most widely used method of expanding the lumen of the colon for procedure. It has been used since the advent of colonoscopy in the 1960s, but it is one of the most obvious causes of patients’ discomfort during and after the procedure. 1
The search for solutions to this annoying issue in this frequently used and broadly indicated procedure has led to two alternatives to air insufflation: the use of water and the use of carbon dioxide (CO2). 2,3
CO2 causes less pain than air because it is absorbed 160 times faster than nitrogen and 13 times faster than oxygen, both of which are major components of air. CO2’s first published use as an insufflating agent was for colonoscopy in a 1984 study by Hussein et al. who showed its advantages over air insufflation. 2
Multiple studies have compared air use with CO2 use for diverse insufflation variables such as the frequency and total duration of bathroom use for each patient following a procedure. CO2 was shown to result in less frequent and shorter trips to the bathroom. CO2’s advantages increase the acceptance of colonoscopy by patients and enhance its use as the best screening method for colorectal cancer, inflammatory bowel disease and other pathologies. 4-7
Abdominal bloating and flatulence, also reported by patients, can be measured objectively by the difference between a patient’s abdominal circumference prior to the procedure and after the procedure. It is also less with the use of CO2. 6
Endoscopic retrograde cholangiopancreatography (ERCP) has also been modified during its 50 years of existence to make it increasingly safe. 8 One change that has made it safer and more tolerable has been the use of CO2. 8-12
There are no known comparative studies of Colombian patients that use multivariate analyses to calculate the magnitude of the effect on pain and immediate abdominal distension of the use of CO2 instead of air and which have sufficient power and which statistically adjust for relevant confounding variables related to the procedure.
Consequently, the objective of this study is to measure abdominal pain and bloating following colonoscopy and ERCP according to the insufflating agent, and then to compare the results for CO2 with those for air and to evaluate associated factors.
Materials and methods
This is an observational, prospective, longitudinal and analytical cohort study. A minimum sample size of 80 individuals was calculated to detect a change in the visual analogue scale of one point with a power of 90% and an α significance level of 0.05.
Records of forty-three ERCPs and 20 colonoscopies performed using CO2 insufflation were collected and matched with equal numbers of control cases who had been insufflated with ambient air. In total, 86 ERCP and 40 colonoscopies were included in this study. All procedures were performed at the Union of Surgeons SAS, a center for advanced diagnostic and therapeutic digestive endoscopy located in Manizales, Colombia.
The same colonoscopy and ERCP equipment was used for all patients, and the same propofol sedation protocol was used for all patients. Univariate analysis was performed to characterize patients clinically and demographically. Bivariate analysis was performed to assess differences between pain scores and abdominal girths before and after the procedure and to analyze the comparability of the two groups (CO2 vs. ambient air) using chi-square or Fisher exact tests on qualitative variables. Similarly, parametric and non-parametric tests to identify distributions of numerical variables were developed.
Multivariate analysis to calculate the relative risk (RR) of abdominal distension and pain after procedure was then performed. The insufflating agent adjusted for other variables with statistical and epidemiological criteria was analyzed as an explanatory variable by using a binomial regression model. 13,14,15
Prior review and approval of an institutional ethics committee was obtained for this study, and it was classified as a minimal risk investigation that is in accordance with the principles established in the Helsinki Declaration, the guidelines of the Council of International Organizations of Medical Sciences (CIOMS), and in Resolution 008430 of October 4, 1993.
Results
One hundred twenty-six records of 83 women (65.9%) and 43 men (34.1%) between 14 and 93 years of age (mean age of 59.6 ± 18.1 years) were analyzed. Forty colonoscopies and 86 ERCP were recorded. The most frequent reasons for performing colonoscopy were rectal and abdominal pain, while the most frequent reasons for ERCP were choledocholithiasis, removal and placement of stents, shunts, and dilation of stenosis (Figure 1).
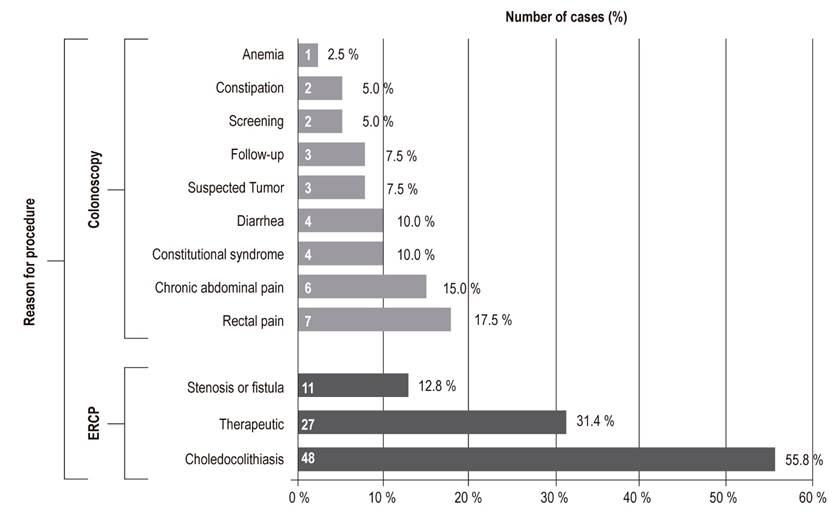
Figure 1 Principal Reasons for ERCP and colonoscopy. ERCP: endoscopic retrograde cholangiopancreatography.
Clinical Results following Colonoscopy and ERCP
Abdominal Pain prior to and after Procedure
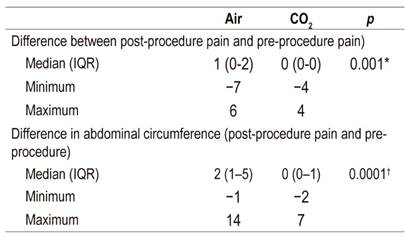
A higher percentage of patients had no before the procedure (79.4%) than after (59.5%). Scores associated with moderate to severe pain (Greater than 3) were more frequent after the procedure. A statistically significant difference was found between pain prior to procedure and pain after procedure (Wilcoxon test, p = 0.0004). The differences between pain prior to procedure and pain 15 minutes after procedure according to the insufflating agent were statistically significant when analyzed separately (Table 1).
Post-procedure and Pre-procedure Abdominal Circumference
Patients’ abdominal circumferences after procedure were smaller in the group insufflated with CO2. The difference was statistically significant way (p = 0.0001). When analyzed alone, differences for colonoscopies (p = 0.015) and ERCP (p = 0.0001) were also statistically significant.
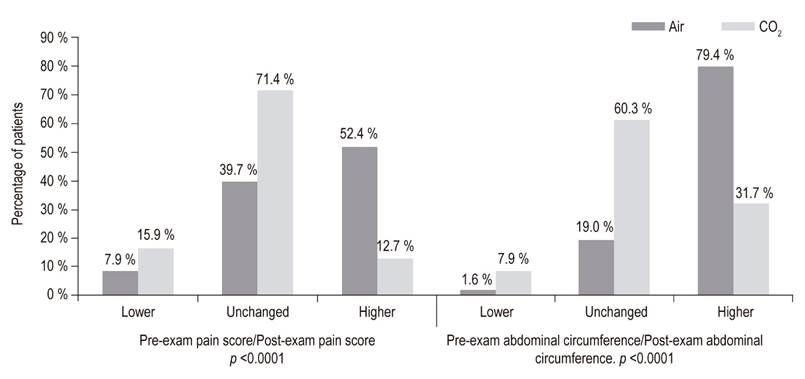
Analysis of the probability of a qualitative change between post-procedure and pre-procedure measurements found that the difference between the two insufflating agents was most clearly evident 15 minutes after patients woke up following procedures. While pain and abdominal circumference did not change or improve over time in the majority of patients in the CO2 insufflated group, they tended to increase in the air insufflated group (Figure 2).
Comparison of pain and abdominal circumference before and after procedure, according to the insufflating agent
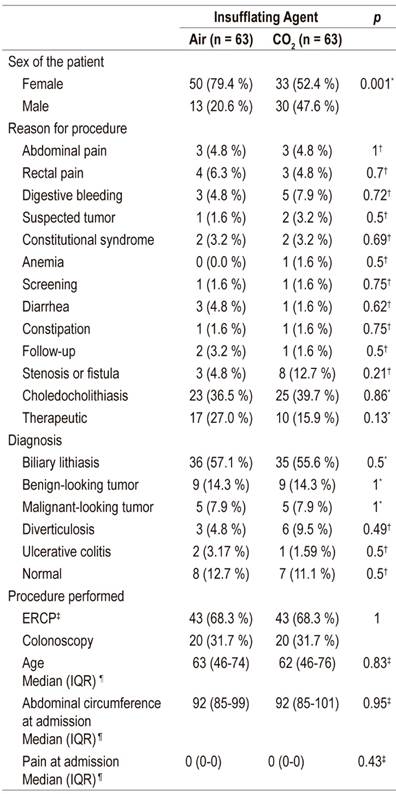
Group comparability
There were no statistically significant differences for these indications. Records were matched so that the number of ERCPs and colonoscopies were exactly the same for each insufflating agent. Similarly, there were no losses of information that altered the comparability of the groups. The only statistically significant difference found was for the gender distribution (Table 2).
Multivariate Analysis
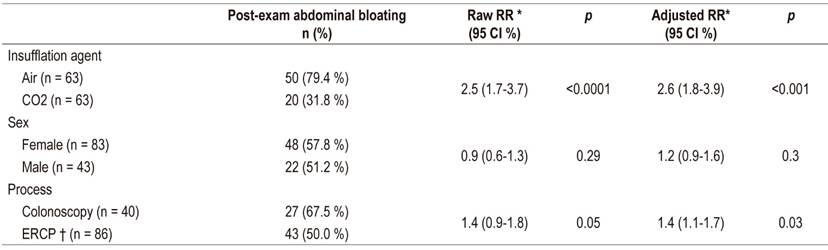
A multivariate model was used to control for the confounding effect of sex, the presence of pain at the time of the exam, the type of procedure, and the reason for the procedure. Any increase in the pain score with respect to the admission score was considered to be post-procedure pain, and any increase in the abdominal circumference was considered to be abdominal distension.
Statistically significant differences were found regarding post-procedure pain according to the insufflating agent (Table 3). The probability of the procedure triggering or worsening pain in air-insufflated patients was 4.8 times greater than the probability in CO2-insufflated patients. This was statistically significantly (95% CI: 2.3 to 9.2; p <0.001) regardless of the type of procedure, the sex of the patient, the reason for the procedure or the presence of pain at admission to the procedure room. It was also observed that the risk of pain after colonoscopy was 1.5 times the risk of pain after ERCP (95% CI: 1.1 to 2.1; p = 0.03).
Table 3 Multivariate analysis of the effect of the insufflating agent on the incidence of pain following colonoscopy and ERCP.
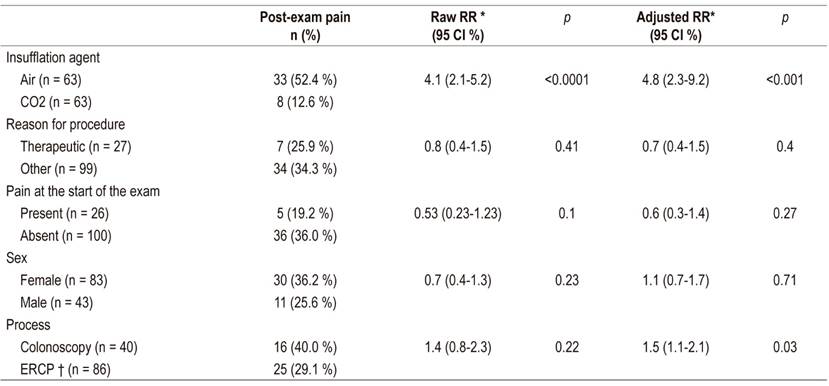
* RR: Relative risk; † ERCP: endoscopic retrograde cholangiopancreatography
Evaluation of the probability that the abdominal circumference would remain enlarged at the end of the procedure found a statistically significant difference according to the insufflating agent and the type of procedure (Table 4). The persistence of increased abdominal circumference was 2.6 times in the group insufflated with air than in the CO2 group (95% CI: 1.8 to 3.9; p <0.001). It was also 1.4 times higher for colonoscopy than for ERCP (95% CI: 1.1 to 1.7, p = 0.03).
Discussion
This analysis’ results regarding abdominal pain and bloating at the time of patient recovery favor use of CO2 as the insufflating agent. Pain was found to occur in 1 out of 8 air-insufflated patients in the period immediately following colonoscopy which is consistent with other studies’ findings. 18,19 Pain was found in 4 out of 10 air-insufflated ERCP patients.
Pain in the immediate post-ERCP period has also been shown to occur less frequently and to be less intense for colonoscopy for either insufflating agent. 8-11,20 This can be explained by the fact that the amount of air or CO2 required to distend the colon area is greater than that required to distend the duodenum for performance of ERCP.
The comparison between changes in the intensity and incidence of pain in all analysis subgroups was statistically significant in favor of the use of CO2 as a strategy to improve the tolerability of the diagnostic procedure, as has been observed in other randomized experimental studies. 1-5
Recent metaanalyses in European and North American populations have also shown evidence of strong statistical association between the use of air insufflation and higher incidence and intensity of immediate and mediate pain. 9,10,12
Similarly, consist with other published studies, abdominal distension was significantly less in our CO2 insufflated group than in the group insufflated with air. 3,6.
The incidence of complications from both procedures does not exceed 0.2% which explains their absence in this study. 21-23
There are no other known, comparable results from Colombia regarding the magnitude of the effect of using CO2 insufflation rather than air insufflation. Although not part of an experimental study, these results provide sufficient evidence that is consistent with the current state of the art in favor of the use of CO2 in colonoscopy and ERCP. CO2 insufflation should be used as a strategy to decrease the incidence and intensity of pain and abdominal bloating in scheduled colonoscopies and ERCP here in Colombia.
Referencias
1. De-Quadros LG, Kaiser-Júnior RL, Felix VN, Villar L, Campos JM, Nogueira VQ, et al. Colonoscopy: randomized comparative study of insufflation with carbon dioxide versus air. Arq Bras Cir Dig. 2017;30(3):177-181. https://doi.org/10.1590/0102-6720201700030004 [ Links ]
2. Kim HG. Painless Colonoscopy: Available Techniques and Instruments. Clin Endosc. 2016;49(5):444-448. https://doi.org/10.5946/ce.2016.132 [ Links ]
3. Chen SW, Hui CK, Chang JJ, Lee TS, Chan SC, Chien CH, et al. Carbon dioxide insufflation during colonoscopy can significantly decrease post-interventional abdominal discomfort in deeply sedated patients: A prospective, randomized, double-blinded, controlled trial. J Gastroenterol Hepatol. 2016;31(4):808-13. https://doi.org/10.1111/jgh.13181 [ Links ]
4. Hsu WF, Hu WH, Chen YN, Lai HH, Chen MK, Chang LC, et al. Carbon dioxide insufflation can significantly reduce toilet use after colonoscopy: a double-blind randomized controlled trial. Endoscopy. 2014;46(3):190-5. https://doi.org/10.1055/s-0034-1365016 [ Links ]
5. Falt P, Šmajstrla V, Fojtík P, Hill M, Urban O. Carbon dioxide insufflation during colonoscopy in inflammatory bowel disease patients: a double-blind, randomized, single-center trial. EurJ Gastroenterol Hepatol . 2017;29(3):355-359. https://doi.org/10.1097/MEG.0000000000000791 [ Links ]
6. Kiriyama S, Naitoh H, Fukuchi M, Yuasa K, Horiuchi K, Fukasawa T, et al. Evaluation of abdominal circumference and salivary amylase activities after unsedated colonoscopy using carbon dioxide and air insufflations. J Dig Dis. 2015;16(12):747-51. https://doi.org/10.1111/1751-2980.12302 [ Links ]
7. Sajid MS, Caswell J, Bhatti MI, Sains P, Baig MK, Miles WF. Carbon dioxide insufflation vs conventional air insufflation for colonoscopy: a systematic review and meta-analysis of published randomized controlled trials. Colorectal Dis. 2015;17(2):111-23. https://doi.org/10.1111/codi.12837 [ Links ]
8. Cotton PB. Fifty years of ERCP: a personal review. Gastrointest Endosc. 2018;88(2):393-396. https://doi.org/10.1016/j.gie.2018.04.013 [ Links ]
9. Memon MA, Memon B, Yunus RM, Khan S. Carbon Dioxide Versus Air Insufflation for Elective Colonoscopy: A Meta-Analysis and Systematic Review of Randomized Controlled Trials. Surg Laparosc Endosc Percutan Tech. 2016;26(2):102-16. https://doi.org/10.1097/SLE.0000000000000243 [ Links ]
10. Zhang WY, Jiang XP, Miao L, Chen FC, Huang ZM, Huang XL. Efficacy and safety of carbon dioxide insufflation versus air insufflation for endoscopic retrograde cholangiopancreatography: A meta-analysis update. Clin Res Hepatol Gastroenterol. 2017;41(2):217-229. https://doi.org/10.1016/j.clinre.2016.10.001 [ Links ]
11. Muraki T, Arakura N, Kodama R, Yoneda S, Maruyama M, Itou T, et al. Comparison of carbon dioxide and air insufflation use by non-expert endoscopists during endoscopic retrograde cholangiopancreatography. Dig Endosc. 2013;25(2):189-96. https://doi.org/10.1111/j.1443-1661.2012.01344.x [ Links ]
12. Shi H, Chen S, Swar G, Wang Y, Ying M. Carbon dioxide insufflation during endoscopic retrograde cholangiopancreatography: a review and meta-analysis. Pancreas. 2013;42(7):1093-100. https://doi.org/10.1097/MPA.0b013e3182909da5 [ Links ]
13. Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79(3):340-9. https://doi.org/10.2105/AJPH.79.3.340 [ Links ]
14. Kovalchik SA, Varadhan R, Fetterman B, Poitras NE, Wacholder S, Katki HA. A general binomial regression model to estimate standardized risk differences from binary response data. Stat Med. 2013;32(5):808-21. https://doi.org/10.1002/sim.5553 [ Links ]
15. McInturff P, Johnson WO, Cowling D, Gardner IA. Modelling risk when binary outcomes are subject to error. Stat Med. 2004;23(7):1095-109. https://doi.org/10.1002/sim.1656 [ Links ]
16. Ministerio de Salud de la República de Colombia. Resolución número 8430 de 1993: por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá; 1993. [ Links ]
17. Lolas F. Aspectos éticos de la investigación biomédica. Conceptos frecuentes en las normas escritas. Rev Med Chile. 2001;129(6):680-684. https://doi.org/10.4067/S0034-98872001000600014 [ Links ]
18. Liu X, Liu D, Li J, Ou D, Zhou Z. Safety and efficacy of carbon dioxide insufflation during colonoscopy. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2009;34(8):825-9. [ Links ]
19. Díez-Redondo P, Gil-Simón P, Alcaide-Suárez N, Atienza-Sánchez R, Barrio-Andrés J, De-la-Serna-Higuera C, et al. Comparison between insufflation with air or carbon dioxide during the colonoscopy in sedated patients with propofol. Rev Esp Enferm Dig. 2012;104(8):411-7. https://doi.org/10.4321/S1130-01082012000800004 [ Links ]
20. Cheng Y, Xiong XZ, Wu SJ, Lu J, Lin YX, Cheng NS, et al. Carbon dioxide insufflation for endoscopic retrograde cholangiopancreatography: A meta-analysis and systematic review. World J Gastroenterol. 2012;18(39):5622-31. https://doi.org/10.3748/wjg.v18.i39.5622 [ Links ]
21. Ibáñez J, Vanaclocha-Espí M, Pérez Sanz E, Valverde MJ, Sáez-Lloret I, Barceló AM, et al. Complicaciones graves en las colonoscopias de cribado del cáncer colorrectal en la Comunidad Valenciana. Gastroenterol Hepatol. 2018;41(9):553:561. https://doi.org/10.1016/j.gastre.2018.11.008 [ Links ]
22. Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102(8):1781-8. https://doi.org/10.1111/j.1572-0241.2007.01279.x [ Links ]
23. Katsinelos P, Lazaraki G, Chatzimavroudis G, Gkagkalis S, Vasiliadis I, Papaeuthimiou A, et al. Risk factors for therapeutic ERCP-related complications: an analysis of 2,715 cases performed by a single endoscopist. Ann Gastroenterol. 2014;27(1):65-72. [ Links ]
Received: December 18, 2018; Accepted: May 03, 2019











 texto em
texto em