Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.1 Bogotá jan./mar. 2020
https://doi.org/10.22516/25007440.363
Original articles
Prevalence and histological characteristics of tiny rectal and sigmoid polyps in a Colombian population
1Internista, Fellow de gastroenterología; Universidad Nacional de Colombia, Hospital Universitario de Colombia. Bogotá, Colombia
2Profesor titular de Medicina, Unidad de Gastroenterología, Universidad Nacional de Colombia; Hospital Universitario Nacional de Colombia, gastroenterólogo en Clínica Fundadores. Bogotá, Colombia
3Profesor asociado de Medicina, Unidad de Gastroenterología, Universidad Nacional de Colombia; Hospital Universitario Nacional de Colombia. Bogotá, Colombia
Introduction:
Because colorectal cancer (CRC) originates from adenomatous and serrated polyps, it is recommended that all colonic polyps be resected and sent to pathology. However, there is controversy over this recommendation in the case of rectal and sigmoid polyps measuring less than 5 mm. Strategies using advanced NBI endoscopes to either “resect and discard” or leave “in situ” have been proposed. Concordance with histopathology of over 90% has been achieved. No prospective studies of the prevalence and histological characteristics of these rectal and sigmoid polyps had been done with white light in this country, so we undertook this study.
Materials and methods:
This is an analytical and prospective prevalence study. Screening colonoscopies performed in the gastroenterology unit of Clínica Fundadores in Bogotá between January and July 2018 were included.
Results:
Seven hundred nineteen patients were included. The prevalence of tiny polyps in the rectum and sigmoid colon was 27% (95% CI: 23.7 to 30.2%). Fifty percent were adenomatous, but eight cases had high grade dysplasia. Among the tiny polyps, three were neuroendocrine tumors. There was no cancer in any of the lesions.
Conclusions:
Half of the tiny polyps found were adenomatous, and eight (0.83%) had high grade dysplasia. We recommend resecting all tiny polyps until local studies conducted with NBI or other technology demonstrate the ability to discriminate between the more than 90% hyperplastic polyps (leaving them in situ) and adenomatous polyps (resect them).
Keywords: Tiny polyps; polyps; adenomas
Introducción:
el cáncer de colon y recto (CCR) se origina a partir de pólipos adenomatosos y serrados. Por tanto, se recomienda que todos los pólipos colónicos sean resecados y enviados a patología. Sin embargo, en los pólipos diminutos (<5 mm) del recto y del sigmoides existe controversia sobre esta conducta, razón por la cual se ha planteado la estrategia de resecar y descartar o dejar in situ, a partir de la utilización de endoscopios avanzados (con una imagen de banda angosta [Narrow Band Imaging, NBI] u otras), y se logre concordancia con la histopatología, superior al 90 %. En nuestro medio, no hay estudios prospectivos con luz blanca sobre la prevalencia y las características histológicas de estos pólipos en el recto y el sigmoides. Por esta razón, se desarrolló este trabajo.
Materiales y métodos:
estudio de prevalencia analítica, prospectivo. Se incluyeron las colonoscopias de tamización realizadas en la Unidad de Gastroenterología de la Clínica Fundadores de Bogotá, entre enero y julio de 2018.
Resultados:
se incluyeron 719 pacientes. La prevalencia de pólipos diminutos en el recto y el sigmoides fue del 27 % (intervalo de confianza [IC], 95 %: 23,7-30,2 %). El 50 % eran pólipos adenomatosos, mientras que en 8 casos se presentó una displasia de alto grado (DAG). Entre los pólipos diminutos, 3 fueron tumores neuroendocrinos. No hubo cáncer en ninguna de las lesiones.
Conclusiones:
la mitad de los pólipos diminutos encontrados fueron adenomatosos y 8 (0,83 %) tuvieron DAG. Recomendamos resecar todos los pólipos diminutos hasta que los estudios locales realizados con NBI u otra tecnología demostrasen la capacidad para discriminar en más del 90 % los pólipos hiperplásicos (dejarlos in situ) o adenomatosos (resecarlos).
Palabras clave: Pólipos diminutos; pólipos; adenomas
Introduction
Colon cancer (CC) is the third most common cancer and the fourth leading cause of cancer death throughout the world. 1 In Colombia it is also the fourth leading cause of cancer mortality. 2 Morphologically, colorectal polyps (CRP) are categorized on the basis of the Paris classification into sessile, flat, and pedicled polyps. 3 Histologically, they can be either non-neoplastic including hyperplastic, hamartomatous and inflammatory, or adenomatous or serrated. These last two constitute precancerous lesions that can cause CC. 4,5
Adenomas are considered advanced when they are larger than 10 mm and have a villous component and/or high-grade dysplasia. 5 Currently, it is recommended that all the polyps found should be resected and sent to pathology, 6,7 but this recommendation is controversial for tiny polyps which measure less than 5 mm. Tiny polyps have a low potential for malignancy, 8 and they represent 70 to 80% of all polyps found. 5-9
Recently, a strategy of resect and discard rather than resect and send to pathology has been recommended. The majority of CRP are tiny polyps which create a high volume for pathology services and generate high economic costs. 10 In the United States, the annual cost of histological study of CRPs is estimated to be $730 million. 10 Due to the costs of histopathological analysis of rectosigmoid polyps and their low potential for malignancy, the use of advanced endoscopes such as narrow band imaging (NBI), Flexible Spectral Imaging Color Enhancement (FICE), iScan, or Blue Light Imagining (BLI) has been emphasized for endoscopic characterization, for distinguishing neoplastic (adenomas) from non-neoplastic (hyperplastic) polyps, and for guiding decisions about whether to resect and send them to pathology (neoplastic) or to leave them in situ (hyperplastic). 11-14
High level of agreement between endoscopists who are experts in these advanced endoscopes and the pathologists of an institution plus positive and negative predictive values are over 90% for distinguishing between these two types of polyps should guide decisions about whether to resect them (adenomas) or leave them in-situ 13,14
However, advanced endoscopes and endoscopists with levels of expertise high enough to interpret vascular, surface glandular morphology, and color different patterns are not always available in every location for distinguishing among hyperplastic polyps, adenomatous polyps and invasive carcinoma. 13
Considering that no prospective studies of the use of new technologies for examining tiny polyps of the rectum and sigmoid have been done here in Colombia, we decided to carry out this initial study. Our objective is to use high definition white light endoscopy to determine the prevalence of tiny polyps in the rectum and the sigmoid and to study their histological characteristics.
Our results could impact future use of advanced endoscopes for routine management of these lesions and be used for recommendations about whether traditional or white light endoscopes should be used.
Materials and methods
This is a prospective, analytical, cross-sectional prevalence study carried out during the period between January and June 2018 in the Gastroenterology Unit of Clínica Fundadores, a third-level institution attached to the Gastroenterology postgraduate course of the National University of Colombia.
The main objective of the study was to determine the prevalence and histological characteristics of tiny rectal and sigmoid polyps in patients undergoing diagnostic and screening colonoscopies. The study population consisted of adults who underwent a total colonoscopy and had tiny polyps in the rectum and/or sigmoid colon who also agreed to participate in the study.
Exclusion criteria were a history of CC, colon surgery due to any cause, inflammatory bowel disease, polyposis syndrome, hereditary non-polyposis CC, use of anticoagulant, and refusal to participate in the study. People taking anticoagulants were excluded due to the risk of bleeding after resection of polyps. Those with Boston colon preparation scores of less than six were also excluded. 15
Colonoscopy was performed using Olympus 145, Olympus 160 and pediatric colonoscopes with patients in the supine position. This technique was developed by William Otero, one of the authors, and has had a high intubation rate for the cecum, less discomfort for patients, less time to reach, the cecum, and less need for sedation in our institution. This agrees with what was recently published by Zhao et al. 16
Julián Parga and Johanna Gastelbondo, in the final year of their Gastroenterology fellowships at the National University, performed 80% of the colonoscopies, all of which were supervised by William Otero.
Fifty percent of the procedures were performed without sedation, but patients who expressly requested sedation and those who had no tolerance for the examination were sedated (selective sedation). Sedation was always administered by an anesthesiologist with propofol and remifentanil. The colon was prepared with polyethylene glycol (PEG) in divided doses and in accordance with the recommendations of the American Society for Gastrointestinal Endoscopy (ASGE). 17
Polyps were considered to be tiny when then measured less than 5 mm. 18,19 Polyp measurement was empirically estimated with an open clamp next to the polyp.
After measurement, tiny polyps were resected with biopsy forceps with a 6 mm opening when fit within the forceps which allowed the procedure to be accomplished in a single attempt. A cold loop was used if position or size prevented polyps from fitting into the forceps. 18,19
All polyps were recovered, soaked in 10% formalin, and sent to pathology. Study variables were recorded in a data collection instrument designed for this study. Weight was classified according to widely used scales. 20
Statistical analysis
The sample size was estimated using a reference polyp prevalence of 30%, an alpha (α) error of 5%, and a 95% confidence interval. This generated a need for a minimum sample of 235 patients. In addition, frequency tables for each variable were used to calculate the prevalence of qualitative variables and measures of central tendency and dispersion for quantitative variables.
Bivariate analysis of the presence of polyps and each other variable used recategorized ordinal variables. The chi-square test was used to evaluate associations between and among qualitative variables. Fisher’s exact test was used for cases in which more than 10% of the expected frequencies were less than five, Fisher’s T test was used to compare the age and number of polyps.
The prevalence ratio (PR) and confidence interval were used to explore possible associations of the presence of polyps with other variables taken as independent. All tests were performed with a significance level of 5% in which values of p <0.05 were considered to be statistically significant evidence.
Results
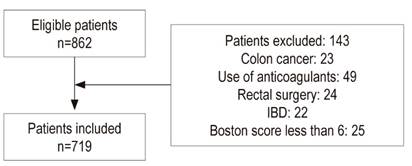
Between January and June 2018, 862 eligible colonoscopies were performed. Using the inclusion and exclusion criteria, 143 patients were excluded for various reasons and 719 were included (Figure 1).
Patients’ average age was 60.9 years, 13.9% were less than 50 years old, 81.6% of them were between 50 and 75 years old, 4.5% were over 75 years old, and 63.7% were women.
Table 1 shows findings related to patients’ weight: 48.4% were overweight and 32.7% had normal body mass indexes. The prevalence of hypothyroidism was 28.7%, that of high blood pressure was 30%, and that of type 2 diabetes was 8.9%.
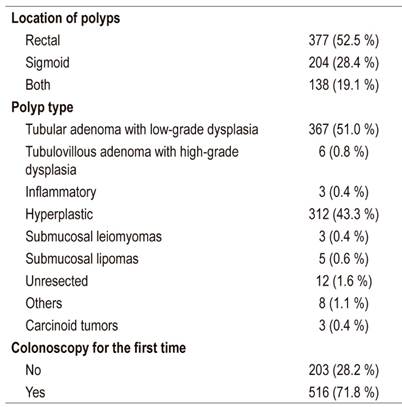
Tiny polyps were found in 194 patients (27%, 95% CI: 23.7% to 30.2%), and 52.5% of polyps were found in the rectum while 28.4% were found in the sigmoid colon. The types of polyps were hyperplastic (41.3%), tubular adenomas with low-grade dysplasia (51%), tubulovillous adenoma with high-grade dysplasia (0.8%), inflammatory (0.4%), submucosal leiomyomas (0.4%), submucosal lipomas (0.6%) and carcinoid tumors (0.4%). Most patients (71.8%) underwent colonoscopy for the first time. There were no complications related to resection of polyps with biopsy forceps or with a cold loop (Table 2).
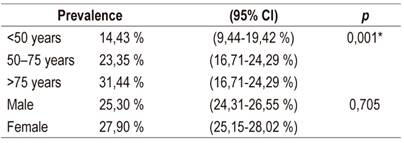
The prevalence of polyps was 14.43% for patients under 50 years of age (95% CI: 9.44% to 19.42%); 23.35% for those between 50 and 75 years of age (95% CI: 16.71% to 24.29%), and 31.44% for those over 75 (95% CI: 20.63% to 33.12%). Significant differences were found in these prevalences (p = 0.001). In men, the prevalence was 25.3%, and in women it was 27.9% (p = 0.705) (Table 3).
Table 1 Demographic characteristics of the study population.

BMI: body mass index; GII: grade II (severe); GIII: grade III (morbid)
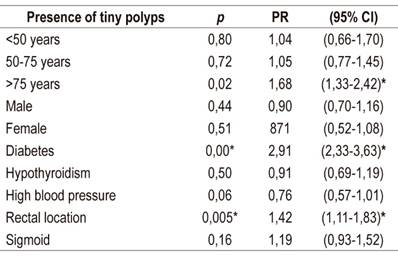
Associations between the presence of polyps and obesity, location, age and quality of preparation were determined using the chi-square test. A significant relationship was found with the location of polyps in the rectum (95% CI: 1.11% to 1.83; p: 0.005) (Table 4). In contrast, diabetes mellitus was positively associated with findings of polyps, with a prevalence ratio of 2.9 (95% CI: 2.33-3.63). Similarly, ages over 75 were positively associated with a prevalence ratio of 1.68 (95% CI: 1.33 to 2.42).
Discussion
We found tiny polyps 27% of the patients analyzed which is similar to prevalences previously published in international studies. (5) Of these, 51.8% were adenomatous with low-grade dysplasia, comparable to the findings of 51% and 54% in two large investigations that included more than 15,000 patients each. 21,22
Of the 719 polyps found, six (0.83%) qualified as high-grade dysplasia. Previous studies have consistently shown that high-grade dysplasia is very rare in this type of lesion with a prevalence between 0.2% and 1.7%. 23,24 Cancer was not found in any of these polyps. The series with the largest numbers of patients have also shown a very low probability of cancer with ranges from 0.0% to 0.8%. 22-26
On the other hand, previous studies have documented that small polyps become advanced lesions at a rate of 3.7% to 4.2% per year. 8 Given this low rate of malignant transformation, controversy has arisen over the impact that resection of these polyps may have on the incidence of CRC. 22 Two European studies dome more than 25 years ago with follow-ups at two and three years found that no tiny polyp reached sizes over 5 mm and did not become either high-grade dysplasia or CRC. 6,26,27
Nevertheless, the true natural history of polyps is unknown since the only way to determine it would be to leave them in situ and perform long-term follow-ups. 22,28 Results are awaited from a recent Canadian study of patients with a specific profile who participated in a study of this nature to determine the incidence of CRC when adenomatous or serrated polyps are left in situ. 29
Until results of that or a similar study become available, arguments about the risk of tiny polyps in the rectum and sigmoid colon becoming malignant will remain theoretical.
In our study there were no immediate or late complications related to polyp resection which is consistent with other prospective studies. 30,31 When bleeding occurred, the amount was minimal, often resolved spontaneously, or was controlled by endoscopic hemostasis by injecting 1:100,000 diluted epinephrine.
We consider the minimal or null rate of complications related resection and the good safety profile of eliminating polyps measuring less than 5 mm to be one more argument for resecting these polyps rather than leaving them in situ which bears a latent risk of CC if they increase in size.
The European Society of Gastrointestinal Endoscopy (ESGE) recommends that all tiny polyps of the rectum and sigmoid be resected except when advanced endoscopes find that they are hyperplastic with high certainty. 32. Whether they are left in situ will depend on high certainty of the optical diagnosis. The ASGE has also made similar recommendations, and a group of experts has recently ratified this strategy. 10,33 In fact, it has been implemented in medical centers in a few countries. 34
Recently, the DISCARD (Detect InSpect ChAracterise Resect and Discard) protocol with which only well characterized, adenomatous and serrated polyps of the rectum and sigmoid colon which have been differentiated from hyperplastic polyps are resected. 35 However, we consider that these strategies, including the DISCARD protocol, cannot yet be implemented in our country with sufficient confidence because NBI is required for demonstration of correlation between morphology and histology.
Furthermore, among endoscopists there is a 10-fold variability in the number of adenomas detected per patient. This implies that some of these specialists may leave some adenomas in situ. 36 Although resection of tiny polyps may increase costs, histopathological evaluation remains important because the presence of adenomas can determine the risk for CC and influence intervals of colonoscopic monitoring. 37
In fact, a relatively recent study has shown that for every 1% absolute increase in the Adenoma Detection Rate (ADR), the risk of CRC decreases by 3%. 38 Endoscopists with high ADRs are probably those who identify and eliminate even the smallest polyps which helps in the prevention of CRC.
In our study, there were three neuroendocrine tumors (0.4%). In agreement with other published studies, tiny neuroendocrine tumors constitute incidental findings in screening colonoscopies in which there are also tiny lesions. 39,40,41.
Taken together, the main results of this study, specifically that more than half of the tiny polyps were adenomatous, that six (0.8%) presented high-grade dysplasia (advanced lesions), and that were neuroendocrine tumors, pose the need to resect these lesions when high definition white light colonoscopy is performed.
Although high-grade dysplasia in lesions that are larger than 10 mm may warrant the review of an expert gastrointestinal pathologist, 42 this type of specialist is not usually available in many places including at this institution. Thus, when three to eight 5-8 mm adenomas are identified, the guidelines recommend a follow-up colonoscopy in three years. 43 Tiny CRPs fall into this category and this constitutes another argument to characterize them histologically.
Currently, it is not possible to predict which polyps will remain stable and which will progress since this requires NBI and determination of the local correlation between the morphology found with this technology and histological findings. If the agreement were to be high, it would suffice only to resect those with an adenomatous component. Although it is rare for tiny polyps to have high-grade dysplasia, in this study 0.8% did which confers more risk of CRC. Furthermore, the presence of adenomas that by definition have low-grade dysplasia implies a risk of growth and long-term neoplastic alterations.
Acknowledgements
We would like to thank Dr. Johana Gastelbondo for her interest in identifying eligible patients, performing colonoscopies, and providing information for the database. We thank Dr. Diego Cano for his interest in identifying eligible patients, providing information for the database and carefully observing colonoscopies. We thank Liliana Oino, the biomedical engineer who is the administrative coordinator of the Gastroenterology Unit and the Teaching Assistance Agreement between the Clínica Fundadores and the Universidad Nacional for her permanent enthusiasm and participation in identifying eligible patients, and monitoring data entry for this study. We thank doctors Hernán Ballén, Elder Otero and Álvaro Rodríguez, for their enthusiasm and interest in identifying eligible patients
REFERENCES
1. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3(4):524-548. https://doi.org/10.1001/jamaoncol.2016.5688 [ Links ]
2. Gil FL, Torres M, Riveros SV, Castaño R, Ibáñez H, Huertas MM, et al. Guía de práctica clínica para la tamización del cáncer colorrectal - 2015. Rev Col Gastroenterol. 2015;30(1 Suppl ):67-74. [ Links ]
3. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003;58(6 Suppl):S3-43. https://doi.org/10.1016/S0016-5107(03)02159-X [ Links ]
4. Rex DK, Alikhan M, Cummings O, Ulbright TM. Accuracy of pathologic interpretation of colorectal polyps by general pathologists in Community practice. Gastrointest Endosc. 1999;50(4):468-74. https://doi.org/10.1016/S0016-5107(99)70067-2 [ Links ]
5. Pickhardt PJ, Kim DH. Colorectal cancer screening with CT colonography: key concepts regarding polyp prevalence, size, histology, morphology, and natural history. AJR Am J Roentgenol. 2009;193(1):40-6. https://doi.org/10.2214/AJR.08.1709 [ Links ]
6. Winawer SJ, Zauber AG, Ho MN, O’Brien MJ, Gottlieb LS, Sternberg SS, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329(27):1977-81. https://doi.org/10.1056/NEJM199312303292701 [ Links ]
7. Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011;154(1):22-30. https://doi.org/10.7326/0003-4819-154-1-201101040-00004 [ Links ]
8. Brenner H, Altenhofen L, Stock C, Hoffmeister M. Natural history of colorectal adenomas: birth cohort analysis among 3.6 million participants of screening colonoscopy. Cancer Epidemiol Biomarkers Prev. 2013;22(6):1043-51. https://doi.org/10.1158/1055-9965.EPI-13-0162 [ Links ]
9. Regula J, Rupinski M, Kraszewska E, Polkowski M, Pachlewski J, Orlowska J, et al. Colonoscopy in colorectal-cancer screening for detection of advanced neoplasia. N Engl J Med. 2006;355(18):1863-72. https://doi.org/10.1056/NEJMoa054967 [ Links ]
10. Patel S, Scott FI, McGill S, Kaltenbach TR, Ahnen D, Das A, et al. 945 Cost Effectiveness Analysis Evaluating Real-Time Characterization of Diminutive Colorectal Polyp Histology Using Narrow Band Imaging (NBI): Implications for the Resect and Discard Strategy. Gastrointestinal endoscopy 2017;85(5): AB116-AB117. https://doi.org/10.1016/j.gie.2017.03.190 [ Links ]
11. Kessler WR, Imperiale TF, Klein RW, Wielage RC, Rex DK. A quantitative assessment of the risks and cost savings of forgoing histologic examination of diminutive polyps. Endoscopy. 2011;43(8):683-91. https://doi.org/10.1055/s-0030-1256381 [ Links ]
12. Hassan C, Pickhardt PJ, Rex DK. A resect and discard strategy would improve cost-effectiveness of colorectal cancer screening. Clin Gastroenterol Hepatol. 2010;8(10):865-9, 869.e1-3. https://doi.org/10.1016/j.cgh.2010.05.018 [ Links ]
13. Rex DK, Kahi C, O’Brien M, Levin TR, Pohl H, Rastogi A, et al. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc . 2011;73(3):419-22. https://doi.org/10.1016/j.gie.2011.01.023 [ Links ]
14. Kamiński MF, Hassan C, Bisschops R, Pohl J, Pellisé M, Dekker E, et al. Advanced imaging for detection and differentiation of colorectal neoplasia: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2014;46(5):435-49. https://doi.org/10.1055/s-0034-1365348 [ Links ]
15. Lai EJ, Calderwood AH, Doros G, Fix OK, Jacobson BC. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc . 2009;69(3 Pt 2):620-625. https://doi.org/10.1016/j.gie.2008.05.057 [ Links ]
16. Zhao S, Yang X, Meng Q, Wang S, Fang J, Qian W, et al. Impact of the supine position versus left horizontal position on colonoscopy insertion: a 2-center, randomized controlled trial. Gastrointest Endosc . 2019;89(6):1193-1201.e1. https://doi.org/10.1016/j.gie.2019.01.009 [ Links ]
17. ASGE Standards of Practice Committee, Saltzman JR, Cash BD, Pasha SF, Early DS, Muthusamy VR, et al. Bowel preparation before colonoscopy. Gastrointest Endosc . 2015;81(4):781-94. https://doi.org/10.1016/j.gie.2014.09.048 [ Links ]
18. Lee J. Resection of Diminutive and Small Colorectal Polyps: What Is the Optimal Technique? Clin Endosc. 2016;49(4):355-358. https://doi.org/10.5946/ce.2016.063 [ Links ]
19. Paggi S, Radaelli F, Repici A, Hassan C. Advances in the removal of diminutive colorectal polyps. Expert Rev Gastroenterol Hepatol. 2015;9(2):237-44. https://doi.org/10.1586/17474124.2014.950955 [ Links ]
20. Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, et al. American Association of Clinical Endocrinologistis and American College of Endocrinology Comprehensive Clinical Practice Guidelines for Medical Care of Patients with Obesity. Endocr Pract. 2016;22 Suppl 3:1-203. https://doi.org/10.4158/EP161365.GL [ Links ]
21. Hassan C, Repici A, Zullo A, Kanakadandi V, Sharma P. Colonic polyps: are we ready to resect and discard? Gastrointest Endosc Clin N Am. 2013;23(3):663-78. https://doi.org/10.1016/j.giec.2013.03.005 [ Links ]
22. Ponugoti PL, Cummings OW, Rex DK. Risk of cancer in small and diminutive colorectal polyps. Dig Liver Dis. 2017;49(1):34-37. https://doi.org/10.1016/j.dld.2016.06.025 [ Links ]
23. Lieberman D, Moravec M, Holub J, Michaels L, Eisen G. Polyp size and advanced histology in patients undergoing colonoscopy screening: implications for CT colonography. Gastroenterology. 2008;135(4):1100-5. https://doi.org/10.1053/j.gastro.2008.06.083 [ Links ]
24. Gupta N, Bansal A, Rao D, Early DS, Jonnalagadda S, Wani SB, et al. Prevalence of advanced histological features in diminutive and small colon polyps. Gastrointest Endosc . 2012;75(5):1022-30. https://doi.org/10.1016/j.gie.2012.01.020 [ Links ]
25. Odom SR, Duffy SD, Barone JE, Ghevariya V, McClane SJ. The rate of adenocarcinoma in endoscopically removed colorectal polyps. Am Surg. 2005;71(12):1024-6. [ Links ]
26. Church JM. Clinical significance of small colorectal polyps. Dis Colon Rectum. 2004;47(4):481-5. https://doi.org/10.1007/s10350-003-0078-6 [ Links ]
27. Hofstad B, Vatn MH, Andersen SN, Huitfeldt HS, Rognum T, Larsen S, et al. Growth of colorectal polyps: redetection and evaluation of unresected polyps for a period of three years. Gut. 1996;39(3):449-56. https://doi.org/10.1136/gut.39.3.449 [ Links ]
28. Bird-Lieberman E, East JE. Diminutive polyps and future colorectal cancer risk perception: how low do we need to go? Endoscopy . 2018;50(3):197-199. https://doi.org/10.1055/s-0044-100493 [ Links ]
29. von Renteln D, Bouin M, Barkun AN, Weber A, Robertson DJ, Anderson JC, et al. Patients’ willingness to defer resection of diminutive polyps: results of a multicenter survey. Endoscopy . 2018;50(3):221-229. https://doi.org/10.1055/s-0043-121221 [ Links ]
30. Paspatis GA, Tribonias G, Konstantinidis K, Theodoropoulou A, Vardas E, Voudoukis E, et al. A prospective randomized comparison of cold vs hot snare polypectomy in the occurrence of postpolypectomy bleeding in small colonic polyps. Colorectal Dis. 2011;13(10):e345-8. https://doi.org/10.1111/j.1463-1318.2011.02696.x [ Links ]
31. Ichise Y, Horiuchi A, Nakayama Y, Tanaka N. Prospective randomized comparison of cold snare polypectomy and conventional polypectomy for small colorectal polyps. Digestion. 2011;84(1):78-81. https://doi.org/10.1159/000323959 [ Links ]
32. Ferlitsch M, Moss A, Hassan C, Bhandari P, Dumonceau JM, Paspatis G, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy . 2017;49(3):270-297. https://doi.org/10.1055/s-0043-102569 [ Links ]
33. Lieberman D, Brill J, Canto M, DeMarco D, Fennerty B, Gupta N, et al. Management of Diminutive Colon Polyps Based on Endoluminal Imaging. Clin Gastroenterol Hepatol . 2015;13(11):1860-6; quiz e168-9. https://doi.org/10.1016/j.cgh.2015.07.011 [ Links ]
34. Sikong Y, Lin X, Liu K, Wu J, Lin W, Wei N, et al. Effectiveness of systematic training in the application of narrow-band imaging international colorectal endoscopic (NICE) classification for optical diagnosis of colorectal polyps: Experience from a single center in China. Dig Endosc. 2016;28(5):583-91. https://doi.org/10.1111/den.12600 [ Links ]
35. Atkinson NS, East JE. Optical biopsy and sessile serrated polyps: Is DISCARD dead? Long live DISCARD-lite! Gastrointest Endosc . 2015;82(1):118-21. https://doi.org/10.1016/j.gie.2015.01.059 [ Links ]
36. Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med . 2006;355(24):2533-41. https://doi.org/10.1056/NEJMoa055498 [ Links ]
37. Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson DA, Levin TR. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology . 2012;143(3):844-857. https://doi.org/10.1053/j.gastro.2012.06.001 [ Links ]
38. Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med . 2014;370(14):1298-306. https://doi.org/10.1056/NEJMoa1309086 [ Links ]
39. Basuroy R, Haji A, Ramage JK, Quaglia A, Srirajaskanthan R. Review article: the investigation and management of rectal neuroendocrine tumours. Aliment Pharmacol Ther. 2016;44(4):332-45. https://doi.org/10.1111/apt.13697 [ Links ]
40. Kaminski M, Polkowski M, Regula J: Prevalence and endoscopic features of rectal neuroendocrine tumors (carcinoids) among 50148 participants of the Polish colorectal-cancer screening programme. Gut . 2007;56(suppl III):A310. [ Links ]
41. Scherübl H. Rectal carcinoids are on the rise: early detection by screening endoscopy. Endoscopy . 2009;41(2):162-5. https://doi.org/10.1055/s-0028-1119456 [ Links ]
42. Rex DK, Hassan C, Bourke MJ. The colonoscopist’s guide to the vocabulary of colorectal neoplasia: histology, morphology, and management. Gastrointest Endosc . 2017;86(2):253-263. https://doi.org/10.1016/j.gie.2017.03.1546 [ Links ]
43. Shah TU, Voils CI, McNeil R, Wu R, Fisher DA. Understanding gastroenterologista adherence to polyp surveillance guidelines. Am J Gastroenterol. 2012;107(9):1283-7. https://doi.org/10.1038/ajg.2012.59 [ Links ]
Received: January 28, 2019; Accepted: March 27, 2019











 texto em
texto em