Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.1 Bogotá Jan./Mar. 2020
https://doi.org/10.22516/25007440.376
Review articles
Eosinophilic colitis: a seldom suspected diagnosis
1Centro de Enfermedades Hepáticas y Digestivas CEHYD S.A.S. Bogotá, Colombia
2Centro de Enfermedades Hepáticas y Digestivas CEHYD S.A.S. Bogotá, Colombia
Eosinophilic gastrointestinal disorders (EGID) are a group of disorders that compromise the gastrointestinal tract. The best known is eosinophilic esophagitis while eosinophilic colitis which was first reported in the literature in 1959 is less well-known. Eosinophilic colitis is characterized by functional digestive disorders, most importantly diarrhea. Although there are no clear diagnostic criteria, blood should be tested for eosinophils and biopsies taken by colonoscopies should be studied for histological findings of eosinophilic infiltration.
Eosinophilic colitis especially affects neonates and young adults and has been linked to genetic and allergic causes. Initial treatment consists of the suspension of allergens. Prednisolone is used to treat the disorder, and medications such as budesonide and immunomodulators can be used in refractory cases to achieve adequate response. We present an update.
Keywords: Colitis; eosinophilic; diarrhea; colonoscopy; biopsies
La enfermedad gastrointestinal eosinofílica (EGIE) agrupa diversas patologías que pueden comprometer el tracto gastrointestinal. La más conocida de ellas es la esofagitis eosinofílica, mientras que la menos distinguida es la colitis eosinofílica (CE), que fue informada por primera vez en la literatura de 1959.
La CE se caracteriza por la existencia de trastornos funcionales digestivos y la diarrea se constituye en el más importante de estos. Aunque no existen unos criterios diagnósticos claros, se considera que los pacientes deben presentar hemogramas con eosinofilia y hallazgos histológicos de infiltración eosinofílica, los cuales son determinados por el estudio histológico de las biopsias tomadas mediante la colonoscopia.
Así pues, la CE afecta especialmente a neonatos y adultos jóvenes, y se ha relacionado con causas genéticas y alérgicas. El tratamiento inicial consiste en la suspensión de los alérgenos. Dentro del arsenal farmacológico, se emplea la prednisolona, así como medicamentos entre los que se incluyen la budesonida y los inmunomoduladores en los casos refractarios, con lo cual se logra una adecuada respuesta. Presentamos una actualización de este tema.
Palabras clave: Colitis; eosinofílica; diarrea; colonoscopia; biopsias
Introduction
The first study of eosinophilic gastrointestinal disease (EGID) was published in Germany by Kaijser in 1937. 1 In 1959, the first publication on this pathology in the English-language literature was a case study of eosinophilic colitis (EC). 2
EGID etiology is classified into primary and secondary depending on the pathogenesis. It is also categorized into immunoglobulin E (IgE) mediated EGID and that which is not mediated by IgE. Similarly, it can be divided into eosinophilic esophagitis (EE), eosinophilic gastroenteritis (GE) and eosinophilic colitis (EC) based on the segment that is involved. 3
EGID and EC are rare diseases and about which little is known, and for which no clear histological criteria have been established. Consequently, diagnosis and incidence are difficult to determine. In general, patients present three characteristics: blood counts with 5% to 35% eosinophils (Although, up to 23% of cases have normal blood counts.), eosinophilic infiltration of the gastrointestinal tract, and functional abnormalities. 4-6
According to a global registry published in 2002, EGID mainly affects the pediatric population although its occurrence has been reported in individuals of up to 68 years of age. 7 Recent research into EE, the most widely studied variety, has revealed that its incidence is increasing. 8,9 Its prevalence has been found to be 22.7 per 100,000 people in population studies from North America, Europe, and Australia. 9 In the case of the United States, a prevalence of 25.9 per 100,000 inhabitants has been reported. 10
EC, the least frequent type of EGID, seems to have a bimodal distribution. It affects neonates with a relatively high prevalence but also affects a separate group of young adults among whom its prevalence is lower. 11 A recent review states that EC is exceptionally rare although it is estimated that this disease may be more common than is assumed. 12,13
Epidemiology and etiology
A 5-year review found the prevalence of EC in the United States to be 2.1 per 100,000 people and that this disease is more common among adults than children. 14 Similarly, it established that EC presents a bimodal distribution: occurring in infants and young children and also in adults between 30 and 50 years old.
Although EC’s etiology is unclear, important genetic and allergic components have been identified. About 16% of patients have a family history of similar illnesses, while 80% report a history of atopic disease, and up to 62% have intolerance of some type of food. 12,15
Histological findings of mast cell accumulations and loss of granular pattern in colonic tissue in children suggest that IgE plays a predominant role. In adults, unusual anaphylaxis related to a particular type of food indicates the existence of a mechanism associated with CD4 + Th2 lymphocytes. 16
Diagnosis
Symptoms presented by a patient with EC depend on the layer of the colon that is compromised. When the mucosa is infiltrated by eosinophils, patients develop abdominal pain, nausea, vomiting, diarrhea, and malnutrition. Patients with transmural compromises present motility disorders and intestinal obstruction, and those whose serous layer is compromised may present eosinophilic ascites. 17,18
Although no global consensus EC diagnostic criteria exist yet, it is considered that diagnosis requires gastrointestinal symptoms, eosinophilia found in a blood test, and a histological finding of eosinophilic infiltration (Figure 1) of one or more segments of the colon. Some authors also say that other causes of EC should be excluded before EC is diagnosed. 15,18
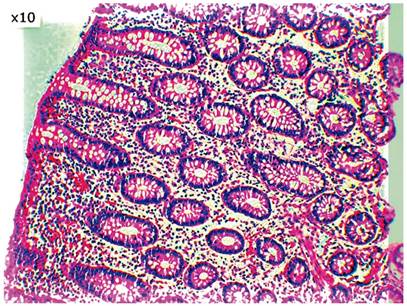
Figure 1 Eosinophilic infiltration of the lamina propria. Image courtesy of Dr. Jorge Monroy, Chief of Pathology at the Central Police Hospital.
Endoscopically, up to 50% of patients have normal colonoscopies. Nonspecific macroscopic changes are seen particularly in the ascending colon and rectum. 19
Histologically, groups of eosinophils infiltrate the lamina propria with an extension to the submucosa through the muscularis propria (Figures 2A and 2B) with an eosinophilic gradient from proximal to distal. The highest concentration of eosinophils (up to 35 per high power field) is usually found in the cecum. 20 A majority of authors accept 20 or more eosinophils per high power field as diagnostic. 20
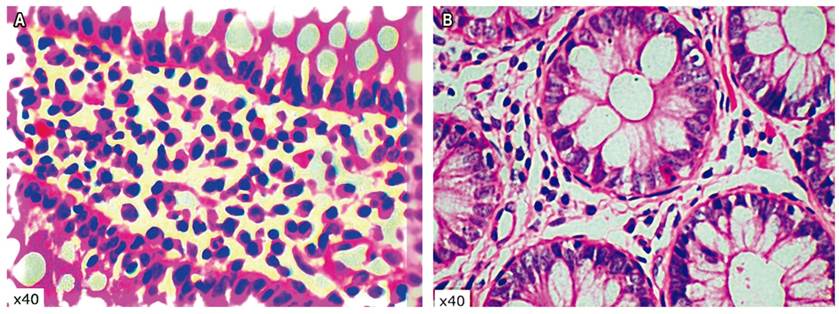
Figure 2 A. Dense mononuclear inflammatory infiltrate with abundant eosinophils in the lamina propria. B. Eosinophil-permeated epithelium. Images courtesy of Dr. Jorge Monroy, Chief of Pathology at the Central Police Hospital.
Key differential diagnoses include eosinophilic infiltration of the colon due to parasitic colitis, EG, inflammatory bowel disease (IBD), drug colitis caused by non-steroidal anti-inflammatory drugs (NSAIDs) such as rifampin, carbamazepine, tacrolimus, and other conditions. 15,18,19
Unusual causes of EC include leukemia, lymphoma, vasculitis such as Churg-Strauss syndrome, and polyarteritis nodosa. 12,21 There have also been reports cases of EC progressing to ulcerative colitis after several months, 21 and cases related to scleroderma and its appearance after liver transplantation in children. 22
Treatment
Childhood EC generally has a benign course and symptoms resolve within a few days after allergens are discontinued. One allergen is cow’s milk. In this scenario, breastfeeding should continue, but consumption of cow’s milk by the mother should be suspended. 11 Before adults start steroid treatment with steroids, parasitic infections should be ruled out with blood and stool tests. 12,19
The use of 1-2 mg/kg/d of prednisolone for 8 weeks followed by administration of decreasing doses has been effective in 80% to 100% of both pediatric and adult patients according to non-randomized studies. 12,18
Immunomodulators (azathioprine and 6-mercaptopurine) and budesonide have been shown to be useful in refractory, severe, or steroid-dependent cases. 17,23 Sodium cromoglycate, a leukotriene antagonist, has been relatively effective for treating EG, but its role in EC has not yet been evaluated.
Some authors have reported the use of ketotifen, omalizumab (monoclonal antibody against IgE), mepolizumab (monoclonal antibody against interleukin-5), infliximab, and proton pump inhibitors (PPIs), but there is less evidence for the effectiveness of these drugs. 19,20,24
EC in adults is considered a chronic disorder with periods of activity and remission. Long-term follow-ups have shown that up to 30% of patients have spontaneous remissions, 60% respond to steroids or diet, and up to 10% have refractory disease. 12,18
Conclusions
The diagnosis of EC should be considered part of the study of patients with chronic diarrhea. For this purpose, colonoscopy with staged biopsies is necessary. Although there is no consensus regarding diagnostic criteria, the existence of EC should be suspected in people with gastrointestinal symptoms whose blood tests show eosinophilia and whose histological findings corroborate the diagnosis.
Although EC’s prevalence is considered to be low, insufficient records and little-suspected records may mask its real prevalence. Consequently, it is of great importance to carry out studies needed for proper diagnosis and treatment of these patients.
Acknowledgements
We would especially like to thank Dr. Jorge Monroy, chief of Pathology at the Central Police Hospital, for histological photographs
REFERENCES
1. Kaiser R. Zur Kenntnis der allergischen affektionen des verdauungskanals vom standput des chirurgen aus. Archiv fur Klinische Chirugie. 1937;188:36-64. [ Links ]
2. Dunstone GH. A case of eosinophilic colitis. Br J Surg. 1959;46(199):474-6. https://doi.org/10.1002/bjs.18004619913 [ Links ]
3. Rodríguez R, Bohórquez MA, González I, Torregroza G. Desórdenes eosinofílicos gastrointestinales (DEGI): presentación de dos casos. Rev Colomb Gastroenterol. 2007;22(2):138-148. [ Links ]
4. Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR. Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut. 1990;31(1):54-8. https://doi.org/10.1136/gut.31.1.54 [ Links ]
5. Yan BM, Shaffer EA. Primary eosinophilic disorders of the gastrointestinal tract. Gut. 2009;58(5):721-32. https://doi.org/10.1136/gut.2008.165894 [ Links ]
6. Okpara N, Aswad B, Baffy G. Eosinophilic colitis. World J Gastroenterol. 2009;15(24):2975-2979. https://doi.org/10.3748/wjg.15.2975 [ Links ]
7. Guajardo JR, Plotnick LM, Fende JM, Collins MH, Putnam PE, Rothenberg ME. Eosinophil-associated gastrointestinal disorders: a world-wide-web based registry. J Pediatr. 2002;141(4):576-81. https://doi.org/10.1067/mpd.2002.127663 [ Links ]
8. Dellon ES. Diagnosis and management of eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2012;10(10):1066-78. https://doi.org/10.1016/j.cgh.2012.06.003 [ Links ]
9. Arias Á, Pérez-Martínez I, Tenías JM, Lucendo AJ. Systematic review with meta-analysis: the incidence and prevalence of eosinophilic oesophagitis in children and adults in population-based studies. Aliment Pharmacol Ther. 2016;43(1):3-15. https://doi.org/10.1111/apt.13441 [ Links ]
10. Mansoor E, Cooper GS. The 2010-2015 Prevalence of Eosinophilic Esophagitis in the USA: A Population-Based Study. Dig Dis Sci. 2016;61(10):2928-2934. https://doi.org/10.1007/s10620-016-4204-4 [ Links ]
11. Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004;113(1):11-28. https://doi.org/10.1016/j.jaci.2003.10.047 [ Links ]
12. Alfadda AA, Storr MA, Shaffer EA. Eosinophilic colitis: epidemiology, clinical features, and current management. Therap Adv Gastroenterol. 2011;4(5):301-9. https://doi.org/10.1177/1756283X10392443 [ Links ]
13. Shaikh TP, Ansari S, Deolekar S, Mandhane N, Karandikar S. Eosinophilic colitis in 36 years old female: a case presentation with review of literature. Revista Internacional de Informes Científicos. 2015;1(3):172-176. https://doi.org/10.18203/issn.2454-2156.IntJSciRep20150354 [ Links ]
14. Mansoor E, Saleh MA, Cooper GS. Prevalence of Eosinophilic Gastroenteritis and Colitis in a Population-Based Study, From 2012 to 2017. Clin Gastroenterol Hepatol. 2017;15(11):1733-1741. https://doi.org/10.1016/j.cgh.2017.05.050 [ Links ]
15. Coste P, Campos C, Sauma J. Colitis eosinofílica: presentación endoscópica inusual. Endoscopia. 2016;28(4):166-169. https://doi.org/10.1016/j.endomx.2016.08.001 [ Links ]
16. Prussin C. Eosinophilic gastroenteritis and related eosinophilic disorders. Gastroenterol Clin North Am. 2014;43(2):317-27. https://doi.org/10.1016/j.gtc.2014.02.013 [ Links ]
17. Dionísio de Sousa IJ, Bonito N, Pais A, Gervásio H. Eosinophilic colitis. BMJ Case Rep. 2016;2016. pii: bcr2016214496. https://doi.org/10.1136/bcr-2016-214496 [ Links ]
18. Alhmoud T, Hanson JA, Parasher G. Eosinophilic Gastroenteritis: An Underdiagnosed Condition. Dig Dis Sci. 2016;61(9):2585-92. https://doi.org/10.1007/s10620-016-4203-5 [ Links ]
19. Gaertner WB, Macdonald JE, Kwaan MR, Shepela C, Madoff R, Jessurun J, et al. Eosinophilic colitis: university of Minnesota experience and literature review. Gastroenterol Res Pract. 2011;2011:857508. https://doi.org/10.1155/2011/857508 [ Links ]
20. Hua S, Cook D, Walker MM, Talley NJ. Pharmacological treatment of eosinophilic gastrointestinal disorders. Expert Rev Clin Pharmacol. 2016;9(9):1195-209. https://doi.org/10.1080/17512433.2016.1190268 [ Links ]
21. Mamachen A, Al-Hanayneh M, Bilal M, Merwat S, Hashmi A. Eosinophilic Colitis-”Not as rare”. Dig Liver Dis. 2017;49(7):826-828. http://dx.doi.org/10.1016/j.dld.2017.04.014 [ Links ]
22. Lee JH, Park HY, Choe YH, Lee SK, Lee SI. The development of eosinophilic colitis after liver transplantation in children. Pediatr Transplant. 2007;11(5):518-23. https://doi.org/10.1111/j.1399-3046.2007.00693.x [ Links ]
23. Kefeli A, Yeniova AÖ, Başyiğit S, Güneş N. Eosinophilic colitis presenting with lower gastrointestinal bleeding: An uncommon entity with a rare presentation. Turk J Gastroenterol. 2015;26(5):440-1. https://doi.org/10.5152/tjg.2015.0180 [ Links ]
24. Uppal V, Kreiger P, Kutsch E. Eosinophilic Gastroenteritis and Colitis: a Comprehensive Review. Clin Rev Allergy Immunol. 2016;50(2):175-88. https://doi.org/10.1007/s12016-015-8489-4 [ Links ]
Received: March 17, 2019; Accepted: September 17, 2019











 text in
text in 


