Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957versão On-line ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.2 Bogotá abr./jun. 2020
https://doi.org/10.22516/25007440.364
Original articles
Evaluation of sustained responses to infiltration of local anesthetic in patients with chronic abdominal wall pain
1 Residente de último año de medicina interna, Universidad Nacional de Colombia. Bogotá D. C., Colombia
2 Profesor Titular de Medicina, coordinador de Gastroenterología, Universidad Nacional de Colombia, Hospital Universitario Nacional de Colombia. Gastroenterólogo, Centro de Gastroenterología y Endoscopia. Bogotá D. C., Colombia
3 Epidemiólogo clínico, Universidad Nacional de Colombia. Bogotá D. C., Colombia
4 Docente Universidad Nacional de Colombia, Hospital Universitario Nacional. Gastroenterólogo, Centro de Gastroenterología y Endoscopia. Bogotá D. C., Colombia
Introduction:
Chronic abdominal pain is frequently encountered at outpatient clinics where the traditional approach is to investigate visceral pathologies. Fifty percent of these patients are finally found to have abdominal wall pain which is generally secondary to entrapment of the anterior cutaneous nerve. This entity is identified by Carnett’s sign. The treatment of choice is to infiltrate the painful points with lidocaine following which there is significant improvement in 85% to 90% of these patients. The duration of post-infiltration improvement is unknown. The objective of this work is to determine sustained response in one and two-year follow-up examinations.
Materials and Methods:
This is a retrospective cohort study conducted in the gastroenterology unit of the Clínica Fundadores. We included adult patients over 18 years of age who had received local injection treatment with 2% lidocaine without epinephrine and who had answered a telephone survey to assess the intensity of pain on an analogous scale.
Results:
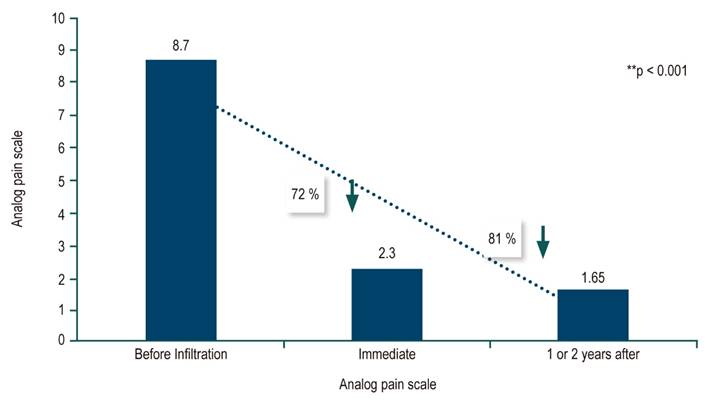
Of the 360 eligible patients identified, 324 patients (90%) were interviewed by telephone. The average age of those interviewed was 57 years, and 87% were women. The average pain level prior to infiltration was 8.7 points. Following infiltration, the average intensity was 2.38 points (p <0.05). In 71% of patients, average pain intensity at a two year follow-up examination was 1.65 points (p <0.05), an 81% improvement in intensity (p = 0.001). Fibromyalgia had a positive association with sustained improvement in pain (p = 0.008).
Conclusions:
Infiltration of the abdominal wall with a local anesthetic produces a sustained response for up to two years in patients with chronic abdominal wall pain.
Keywords: Pain; infiltration; sustained response; Carnett’s sign
Introducción:
el dolor abdominal crónico es frecuente en consulta externa. El enfoque tradicional es investigar patologías viscerales. El 50 % de esos pacientes finalmente tiene dolor crónico de la pared abdominal (DCPA), generalmente secundario a atrapamiento del nervio cutáneo anterior. Esta entidad se identifica con el signo de Carnett. El tratamiento de elección es infiltrar con lidocaína los puntos dolorosos. Con una postinfiltración hay una mejoría significativa en el 85 %-90 % de los pacientes. Se desconoce la duración de la mejoría postinfiltración. El objetivo de este trabajo es determinar la respuesta sostenida en seguimientos a 1 y 2 años.
Materiales y métodos:
estudio de cohorte, retrospectivo, realizado en la unidad de gastroenterología de la Clínica Fundadores. Se incluyeron pacientes adultos mayores de 18 años que hubieran recibido tratamiento con inyección local con lidocaína al 2 % sin epinefrina y que hubieran respondido una encuesta telefónica para evaluar la intensidad del dolor en una escala análoga.
Resultados:
se identificaron 360 elegibles y, finalmente, atendieron la entrevista telefónica 324 pacientes (90 %). El 87 % era de sexo femenino. La edad promedio de la población era de 57 años. En la preinfiltración el dolor promedio era 8,7 puntos. En la postinfiltración los pacientes tuvieron una mejoría con una intensidad promedio de 2,38 (p < 0,05). En el 71 % de los pacientes la intensidad del dolor en el seguimiento hasta 2 años tuvo una intensidad promedio de 1,65 (p < 0,05), que representa una mejoría del 81 % en la intensidad (p = 0,001). La fibromialgia tuvo una asociación positiva con la mejoría sostenida del dolor (p = 0,008).
Conclusiones:
en los pacientes con DCPA, la infiltración de la pared con anestesia local produce una respuesta sostenida hasta 2 años después del tratamiento.
Palabras clave: Dolor; infiltración; respuesta sostenida; Carnett
Introduction
Chronic abdominal pain is a frequent reason for outpatient consultation and occasionally for emergency consultation. 1,2 It has very important implications for individual and for health care system costs. 3,4 Doctors traditionally consider the origin of abdominal pain to be the viscera and intra-abdominal structures and subject patients to multiple examinations and interventions including endoscopy, colonoscopy, ultrasound, CT scans, laparoscopy and even surgery. 4 Excessive costs associated with these procedures can be avoided if the initial approach takes into account the possibility that the pain originates in the structures of the abdominal wall including entrapment of anterior cutaneous nerves. 4-6 Pain can also originate in thoracic structures and endocrine disorders, and there is even centrally mediated chronic abdominal pain, a functional pathology that is difficult to diagnose and treat. 7
Various studies, including one carried out in Colombia, 1 have found that the final diagnosis of up to 50% of these patients is chronic abdominal wall pain (CAWP). The Colombian study found that infiltration of the abdominal wall with 2% lidocaine without epinephrine improved 91% of patients and reduced costs derived from unnecessary studies by 90% when doctors considered this diagnostic possibility. Various international studies have also demonstrated the economic impact of avoiding higher costs through correct diagnoses of this entity. 5,8
The most common cause of CAWP is irritation of the last 7 intercostal nerve roots that innervate the abdominal wall at angles close to the lateral border of the rectus muscles and the skin. 9,10 This anatomical arrangement predisposes the respective nerves to irritation, entrapment or ischemia when there is pressure on the abdominal wall increases due to extra-abdominal causes such as tight clothing, belts or obesity or to intra-abdominal causes such as distension. Also, it is likely that muscle contraction during exercise may contribute. 11-13
CAWP is diagnosed by checking for Carnett’s sign. 9,10 Studies have shown its diagnostic sensitivity to be 88% while its specificity is 97%. 14 A understanding of CAWP has advanced, treatment with infiltration of local anesthesia into the abdominal wall has become more common. It results in 80% improvement of pain with one session and 91% with two or more sessions. 11-13 A randomized, placebo-controlled clinical trial demonstrated the superiority of lidocaine infiltration over infiltration of a placebo. 15 The efficacy of lidocaine may be related to the release of endogenous opioids at sites close to the nerve. This decreases pain and may also break the cycle of pain production by interfering with persistent release of acetylcholine with which the surrounding muscles generate sustained contractions. 16-18 In refractory cases, local surgical treatment has resorted to removal of the cutaneous nerve involved. 19
To date, the only research into CAWP in Colombia and Latin America have been carried out at the National University of Colombia, 1,4 and only the immediate response to treatment with infiltration of anesthesia has been evaluated. Nevertheless, duration of the sustained response over time had not been evaluated, and there are very few studies of this issue in the world literature. For these reasons, we decided to carry out this study to determine how well improvement of pain is sustained for up to two years after the infiltration.
Materials and methods
This is a retrospective cohort study. All adult patients with CAWP who received treatment with infiltration of painful points in the gastroenterology unit of the Fundadores Clinic in Bogotá D.C. between 2017 and 2018 were included. Although diagnosis of CAWP and treatment through infiltration of the abdominal wall have been routine in this service since 2008, and there are consistent records of all patients, those who were seen in the last 2 years were chosen to reduce the possibility that they did not remember the evolution of their pain (memory bias). The informed consent forms and authorizations for infiltration filled out by patients with CAWP were identified in the service’s database. All patients were informed of the nature of the study and subsequently authorized participation in this investigation. The patients were contacted by telephone by the main investigator (JM), and the objective of the investigation was explained. An analogous scale of pain from 0 to10 was used to rate whether pain had improved. A score of zero (0) indicated an absence of pain while a score of ten 10 indicated pain of the greatest intensity. The number of sessions required for injections, other treatments used such as oral analgesics and non-steroid anti-inflammatory drugs (NSAIDs), and patient comorbidities were recorded.
The information collection form registered pain over time as follows: for patients seen in 2017, the evolution of pain discussed occurred 12 to 24 months after treatment while patients seen in 2018 were evaluated less than 12 months after treatment. The objective of the study (end point) was to determine the average intensity of pain. Improvement was stratified as less than 50%, from 50% to 80%, and over 80%. The data collected on the pain and patient characteristics were recorded on the data collection form designed for this study. The protocol and informed consent for this research were approved by the Ethics and Research Committee of the Clínica Fundadores and the Faculty of Medicine of the National University of Colombia.
Patients with active cancer, ascites, cirrhosis, decompensated heart failure (liver pain due to passive congestion), nephrotic syndrome and those treated with anticoagulants were excluded.
Statistical Analysis
Data were analyzed with Excel and SPSS. The chi square (χ2) test and Wilcoxon test were used for comparison of proportions, and p <0.05 was considered statistically significant.
Results
We identified 360 eligible CAWP patients who had received treatment with 2% lidocaine infiltrations without epinephrine in 2017 and 2018. Finally, 324 patients (90%) were successfully interviewed by attended. Eighty-seven percent were female. The average age of the population was 57 years. Pain was assessed with a 0 to 10 point analog scale. Before infiltration, the mean pain of the patients included was 8.7 points. Following infiltration, 72% of the patients improved immediately. Their average pain was 2.38 (p <0.05). One and two years after treatment, 71% of the patients had an average pain of 1.65. This corresponds to a decrease in pain intensity of 81% (p <0.05) (Figure 1).
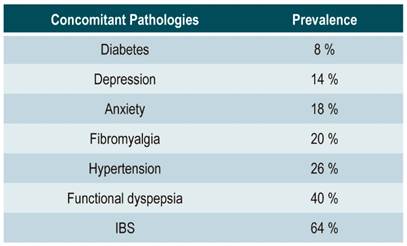
A minimum of two injections were required to achieve the highest degree of immediate pain response, but was not reflected in long term responses which did not depend on the number of injection sessions (p = 0.67). There was no significant difference in responses to infiltration between men and women (p = 0.9). Immediate pain relief was more common in patients who were older than 60 years than those who were 60 years old and younger (p <0.05). This relationship was not reflected in long-term improvement. Comorbidities found are shown in Table 1.
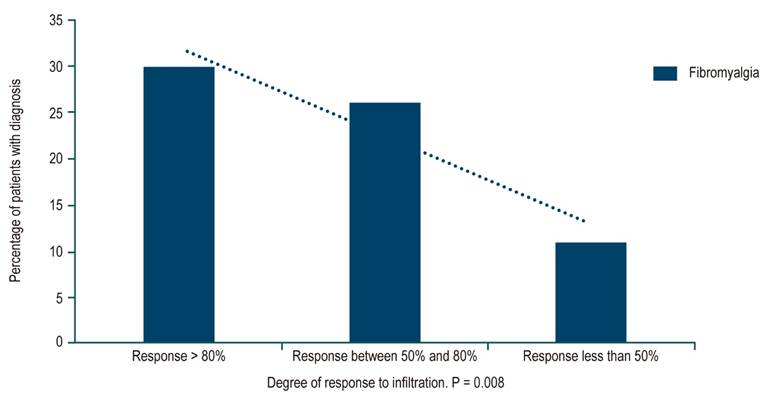
Fibromyalgia, which affected 20% of the patients, was the only comorbidity that was associated with immediate and sustained improvement in pain up to two years after infiltration (p <0.05) (Figure 2).
Diabetes was significantly associated with better immediate responses to lidocaine infiltration (p = 0.01) but had no statistical impact on sustained responses up to 2 years. Other comorbidities were not related to positive responses to infiltration, but functional dyspepsia was related to lower immediate responses to infiltration (p <0.029) although it had no impact on long-term improvement.
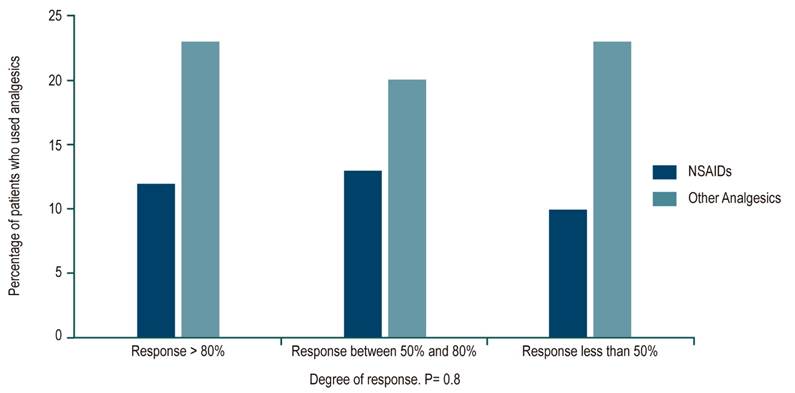
We found that 12% of patients used oral NSAIDs to control abdominal pain, and 23% used other analgesics such as acetaminophen, hyoscine or dipyrone. There were no significant relationships with the degree of immediate or long-term pain improvement (Figure 3).
Discussion
This two-year follow-up study found that 71% of patients maintained sustained pain improvement of more than 80% of the initial intensity recorded before infiltration site(s) of pain. The initial pain score on the analogue scale was 8.7 while it was 1.65 in follow-up interviews up to two years later after only one injection session. Similar results have been published in other studies. 18-22 A study of 140 patients followed for three months by Kuan et al. found that pain intensity decreased by 72% with respect to the initial pain. 20 Another study with a 1.5 year follow-up of 140 patients by Boelens et al. found that the success rate at the end of the observation period was 80%. 21 In that study, anterior cutaneous neurectomies were performed on several refractory patients. Nazareno et al. followed up 99 patients for 25 months following infiltration and found that pain improved by 77% over the initial score. 22 The literature reports that neurectomies have an immediate success rate of 70% and 61% long term (2.5 years) success rate. 19 Our present study of lidocaine infiltration and other similar studies have documented long-term success rates ranging from 71% to 80%. Therefore, we assume that infiltration with anesthesia is preferable to anterior cutaneous neurectomies.
In our study it is striking that 90% of the patients improved immediately after injections, and that relief persisted over time in 72% of them. This is comparable to results in other publications. 1 Differences between initial improvements and those observed months later can be explained by forgetfulness bias and/or the fact that some people are not able to distinguish recurrent pain from functional dyspepsia and pain secondary to IBS (40% and 64% of patients, respectively). These frequencies were higher than those in the study by Constanza et al. who reported pain from functional dyspepsia in 8.3% and pain secondary to IBS in 21.8% of their patients. 5 This difference can be explained by the fact that a large part of the patients seen in primary care at our large gastroenterology clinic are referred for a diagnosis of dyspepsia and IBS. Another possibility is that pain referred to at the time of the survey is secondary to a new episode of entrapment of other anterior cutaneous nerves.
Our study found that 20% of the patients had a diagnosis of fibromyalgia established by rheumatology which is higher than those previously reported in the literature in studies of patients with abdominal wall pain. 23 The positive associations between fibromyalgia, immediate improvement, and sustained improvement raise the possibility that apparent points of CAWP in some patients are in fact due to fibromyalgia. 24 However, studies of patients with fibromyalgia are needed to determine whether CAWP is more frequent among these patients than in a control group without fibromyalgia. Other comorbidities such as arterial hypertension, anxiety, depression and IBS did not significantly influence the response to wall infiltration.
Conclusions
Our review of the world literature found that our study has the largest number of patients included and also has the longest follow-up times. We found that 72% of our patients had an 80% improvement in pain intensity in the long term. Likewise, this study demonstrated that a relatively simple and inexpensive intervention (2% lidocaine infiltration without epinephrine) impacts the well-being of patients and lowers the health care costs by avoiding unnecessary expenses due to irrelevant diagnostic tests and the chain of futile and expensive treatments. 4
Acknowledgements
We would like to thank Dr. Hernán Ballén, Dr. Elder Otero and Dr. Álvaro Rodríguez who are all gastroenterologists in the gastroenterology unit of Clínica Fundadores. We also greatly appreciate the help of all the internal medicine residents at the National University of Colombia for their enthusiasm in identifying, monitoring, and treating multiple patients in this study. We give our very special thanks to Liliana Oino, the biomedical engineer and administrative coordinator of the Gastroenterology Unit and to the teaching-assistance agreement of Clínica Fundadores
REFERENCES
1. Otero W, Ruiz X, Otero E, Gómez M, Pineda LF. Dolor crónico de la pared abdominal: una entidad poco reconocida con gran impacto en la práctica médica. Rev Col Gastroenterol. 2007;22(4):261-71. [ Links ]
2. Rivero M, Moreira V, Riesco JM, Rodríguez MA, Garrido E, Milicua JM. Dolor originado en la pared abdominal: una alternativa diagnóstica olvidada. Gastroenterol Hepatol. 2007;30(4):244-50. https://doi.org/10.1157/13100598 [ Links ]
3. Paajanen H. Does laparoscopy used in open exploration alleviate pain associated with chronic intractable abdominal wall neuralgia? Surg Endosc. 2006;20(12):1835-8. https://doi.org/10.1007/s00464-005-0744-y [ Links ]
4. Otero W, Martínez E, Lúquez A. El costo de ignorar el signo de Carnett, reporte de caso y revisión de literatura. Rev Col Gastroenterol. 2017;32(1):75-81. [ Links ]
5. Constanza CD, Longstreth GF, Liu AL. Chronic abdominal wall pain: clinical feature, health care costs and long term outcome. Clin Gastroenterol Hepatol. 2004;2(5):395-9. https://doi.org/10.1016/S1542-3565(04)00124-7 [ Links ]
6. Sparkes V, Prevost T, Hunter JO. Derivation and identification of questions that act as predictors of abdominal pain of musculoskeletal origin. Eur J Gastroenterol Hepatol. 2003;15(9):1021-7. https://doi.org/10.1097/00042737-200309000-00013 [ Links ]
7. Keefer L, Drossman DA, Guthrie E, Simrén M, Tillisch K, Olden K, Whorwell PJ. Centrally Mediated Disorders of Gastrointestinal Pain. Gastroenterology. 2016;150(6):1408-19. https://doi.org/10.1053/j.gastro.2016.02.034 [ Links ]
8. Thomson C, Goodman R, Rowe WA. Abdominal wall syndrome: a costly diagnosis of exclusion. Gastroenterology. 2001;120(5):637A. https://doi.org/10.1016/S0016-5085(08)83167-8 [ Links ]
9. Carnett JB. Intercostal neuralgia as a cause of abdominal pain and tenderness. Surg Gynecol Obstet. 1926;42:625-32. [ Links ]
10. Carnett JB, Bates W. Carnett JB, Bates W. The treatment of intercostal neuralgia of the abdominal wall. Annals of Surgery. 1933;98(5):820-829. https://doi.org/10.1097/00000658-193311000-00002 [ Links ]
11. Abdominal wall pain easily differentiated from visceral origin. Gastroenterology Observer. 1990;9(6):1-8. [ Links ]
12. Koop H, Koprdova S, Schürmann C. Chronic abdominal wall pain-a poorly recognized clinical problem. Dtsch Arztebl Int. 2016;113(4):51-7. https://doi.org/10.3238/arztebl.2016.0051 [ Links ]
13. Akhnikh S, de Korte N, de Winter P. Anterior cutaneous nerve entrapment syndrome: the forgotten diagnosis. Eur J Pediatr. 2014;173(4):445-9. https://doi.org/10.1007/s00431-013-2140-2 [ Links ]
14. Takada T, Ikusaka M, Ohira Y, Noda K, Tsukamoto T. Diagnostic usefulness of Carnett’s test in psychogenic abdominal pain. Intern Med. 2011;50(3):213-7. https://doi.org/10.2169/internalmedicine.50.4179 [ Links ]
15. Boelens OBA, Scheltinga MF, Houterman S, Roumen RM. Randomized clinical trials on trigger point infiltration with lidocaine to diagnose anterior cutaneous nerve entrapment syndrome. Br J Surg. 2013;100(2):217-21. https://doi.org/10.1002/bjs.8958 [ Links ]
16. Clarke S, Kanakarajan S. Abdominal cutaneous nerve entrapment syndrome. Contin Educ Anaesth Crit Care Pain. 2015;15(2):60-3. https://doi.org/10.1093/bjaceaccp/mku016 [ Links ]
17. Peleg R, Gohar J, Koretz M, Peleg A. Abdominal wall pain in pregnant women caused by thoracic lateral cutaneous nerve entrapment. Eur J Obstet Gynecol Reprod Biol. 1997;74(2):169-71. https://doi.org/10.1016/S0301-2115(97)00114-0 [ Links ]
18. Simons DG, Hong CZ, Simons LS. Endplate potentials are common to midfiber myofascial trigger points. Am J Phys Med Rehabil. 2002;81(3):212-22. https://doi.org/10.1097/00002060-200203000-00010 [ Links ]
19. van Assen T, Boelens OB, van Eerten PV, Perquin C, Scheltinga MR, Roumen RM. Long-term success rates after an anterior neurectomy in patients with an abdominal cutaneous nerve entrapment syndrome. Surgery. 2015:157(1):137-43. https://doi.org/10.1016/j.surg.2014.05.022 [ Links ]
20. Kuan LC, Li YT, Chen FM, Tseng CJ, Wu SF, Kuo TC. Efficacy of treating abdominal wall pain by local injection. Taiwanese J Obstet Gynecol. 2006;45(3):239-43. https://doi.org/10.1016/S1028-4559(09)60232-1 [ Links ]
21. Boelens OB, Scheltinga MR, Houterman S, Roumen RM. Management of anterior cutaneous nerve entrapment syndrome in a cohort of 139 patients. Ann Surg. 2011;254(6):1054‐1058. https://doi.org/10.1097/SLA.0b013e31822d78b8 [ Links ]
22. Nazareno J, Ponich T, Gregor J. Long-term follow-up of trigger point injections for abdominal wall pain. Can J Gastroenterol. 2005;19(9):561-5. https://doi.org/10.1155/2005/274181 [ Links ]
23. Kamboj AK, Hoversten P, Oxentenko AS. Chronic abdominal wall pain: a common yet overlooked etiology of chronic abdominal pain. Mayo Clin Proc. 2019;94(1):139-44. https://doi.org/10.1016/j.mayocp.2018.09.01 [ Links ]
24. Álvarez D, Rockwell PAG. Trigger points: diagnosis and management. Am Acad Fam Phys. 2002; 65: 653-60. [ Links ]
Received: January 30, 2019; Accepted: May 15, 2019











 texto em
texto em