Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957versão On-line ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.2 Bogotá abr./jun. 2020
https://doi.org/10.22516/25007440.409
Original articles
Clinical-epidemiological description of patients with inflammatory bowel disease in a fourth level clinic in Cali
1 Médico internista y gastroenterólogo de la Fundación Valle del Lili y docente de medicina interna y gastroenterología de la Universidad ICESI. Cali, Colombia
2 Residente de medicina interna, Universidad ICESI. Cali, Colombia
3 Estudiante de medicina, Universidad ICESI. Cali, Colombia
Objectives:
In Latin America, inflammatory bowel disease (IBD) is rare, and information about it is limited. This article describes characteristics of IBD patients in a gastroenterology unit at a high-level clinic in Cali, Colombia.
Materials and methods:
This is a descriptive study of patients diagnosed with Crohn’s disease (CD) or ulcerative colitis (UC) at the Clínica Fundación Valle de Lili between January 2011 and December 2015. Statistical analysis was performed with SPSS version 19. Medians and interquartile ranges were calculated for numerical variables. Frequencies were calculated for qualitative variables.
Results:
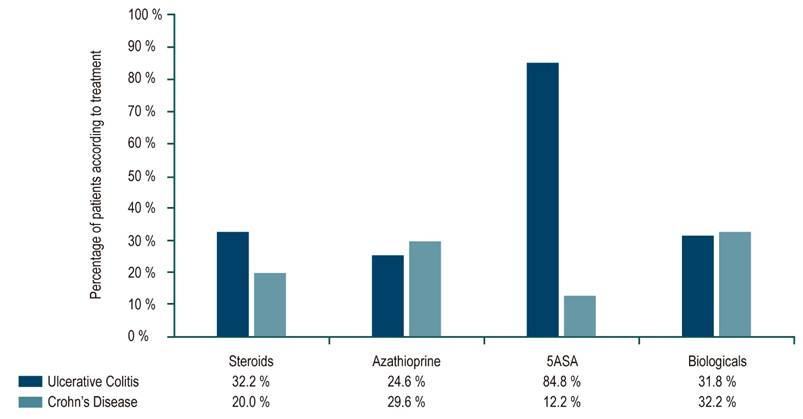
The 416 participants included 115 with CD and 301 with UC. Of the total cases, 41% were classified as mild, 23.5% as moderate and 35.3% as severe. Surgery was performed in 24 patients (9.0%) with UC and 53 (46.1%) with CD. CD was most frequently managed with biologicals (32.2%), followed by immunomodulators (27.8%), steroids (20%) and 5-ASA (11.3%). The most frequent treatment for UC was 5-ASA (84.8%), but 32.19% received steroids, 24.6% received azathioprine and 15.9% received biologicals.
Conclusions:
Early diagnosis remains a challenge. The severity of UC but not CD in the patients studied was less than that reported elsewhere in the world. The difference could be related to diagnostic delay. The use of biologicals was close to that reported in the first world. It is difficult to determine if lower surgery rates are due to better clinical response or to difficult access to these interventions.
Keywords: Inflammatory bowel diseases; ulcerative colitis; Crohn’s disease
Introducción:
en América Latina, la enfermedad inflamatoria intestinal (EII) es poco frecuente y la información, limitada. Se describieron características de los pacientes con EII en una unidad de gastroenterología de una clínica de alto nivel de atención en Cali, Colombia.
Materiales y métodos:
estudio descriptivo de pacientes que consultaron con diagnóstico de enfermedad de Crohn (EC) o colitis ulcerativa (CU) a la Clínica Fundación Valle del Lili entre enero de 2011 y diciembre de 2015. Se realizó un análisis con Statistical Package for the Social Sciences de IBM (SPSS) versión 19, se calcularon la mediana y el rango intercuartílico para las variables numéricas, y frecuencias para las variables cualitativas.
Resultados:
se incluyeron 416 participantes, 115 con EC y 301 con CU. El 41 % se clasificó como enfermedad leve, 23,5 % moderada y 35,3 % grave. Se realizó cirugía a 24 pacientes (9,0 %) con CU y 53 (46,1 %) con EC. En esta última, el manejo más frecuente fue los medicamentos biológicos (32,2 %), seguidos de inmunomoduladores (27,8 %), esteroides (20 %) y ácido 5-aminosalicílico (5-ASA) (11,3 %). El tratamiento más frecuente de CU fue 5-ASA (84,8 %), seguido de esteroides (32,19 %), azatioprina (24,6 %) y biológicos (15,9 %).
Conclusiones:
el diagnóstico precoz sigue siendo un reto. La gravedad de la CU en los pacientes estudiados fue menor a la reportada en el mundo, lo cual no ocurrió con los pacientes con EC y podría estar en relación con el retraso diagnóstico. El uso de medicamentos biológicos se acercó a lo reportado en el primer mundo. Es difícil determinar si las menores tasas de cirugía se deben a una mejor respuesta clínica o a un difícil acceso a estas intervenciones.
Palabras clave: Enfermedades inflamatorias del intestino; colitis ulcerativa; enfermedad de Crohn
Introduction
Crohn’s disease (CD) and ulcerative colitis (UC) are rare chronic conditions of the gastrointestinal tract whose etiologies are only partially understood. Diagnosis is complex and is often delayed due to low incidence and low levels of clinical suspicion. CD affects the gastrointestinal tract transmurally from the mouth to the anus while UC affects the colonic mucosa.
Various studies have evaluated the epidemiology of inflammatory bowel disease (IBD) in different parts of the world. In North America, incidence of UC ranges from 2.2 to 19.2 cases per 100,000 person-years while for CD it ranges from 3.1 to 20.2 cases per 100,000 person-years. 1 In Latin America, an Argentine study found IBD’s incidence to be 2.2 per 100,000 inhabitants. A Chilean study did not establish incidence, but did establish that there is a higher proportion of UC cases and characteristics similar to those reported in Europe. 2 In general, as developing countries raise their standard of living, the incidence of IBD also increases. 3
Information available in Colombia is limited. The first series of cases was published in 1991, 4 and a more recent study found that UC’s behavior is relatively benign with low rates of surgery and mortality although the trend is towards a more frequent diagnosis of CD due to its severity in our population. 5 These data confirmed a smaller study. 6 Prior to this study, there had been no studies in southwestern Colombia. Our study seeks to describe the demographic and clinical characteristics of patients with IBD at the Clínica Fundación Valle del Lili.
Materials and methods
This is a descriptive study based on retrospective data collection. Patients who consulted the Fundación Valle del Lili who were diagnosed with CD and UC from January 2011 to December 2015 were included. Diagnoses were based on the international classification of diseases-10th edition (ICD-10). Patients were pre-selected through manual review of medical records in the Valle del Lili Foundation’s computer documentation system (SAP) which listed CD and UC diagnoses by ICD-10 codes between January 2011 and December 2015. All patients were 18 years or older of both sexes, had been diagnosed with CD or UC on the bases of clinical, serum, histological and/or endoscopic criteria, and had attended the gastroenterology outpatient clinic between January 2011 and December 2015. It was estimated that approximately 100 patients were treated annually. Whether or not they had been assigned an ICD-10 code for IBD, patients under 18 years of age and those who did not meet clinical, serum, histological or endoscopic criteria for a clear diagnosis were excluded.
The following information from the database of the Centro de Investigaciones Clínicas de la Fundación Valle del Lili (BD Clinic) was collected and broken down by diagnosis for further analysis:
Patient characteristics including date of diagnosis, age at diagnosis, sex, type of IBD, time from diagnostic impression to admission, time from admission to first gastroenterology consultation, associated hospital stays, comorbidities, and any history of smoking or alcohol consumption.
Disease characteristics including surgeries related to IBD, IBD in first and second degree relatives, positive autoantibodies of any type (antineutrophil cytoplasmic antibodies (ANCA), perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA), and cytoplasmic staining ANCA (c-ANCA)), albumin and hemoglobin levels, and types of treatment administered.
UC characteristics including initial severity according to the Montreal Classification, presence or absence of extraintestinal manifestations, and remission (defined as complete resolution of symptoms and clinical, endoscopic or histological healing of the colonic mucosa). (7)
Characteristics of CD including Montreal classification, Crohn’s Disease Activity Index (CDAI) n at the time of diagnosis, presence or absence of fistulizing disease, presence or absenc of extraintestinal manifestations, adequate response (defined as an improvement of more than 100 points on the CDAI over previous score), relapse (defined as increased number/intensity of symptoms related to IBD that required medical consultation and which led to increased dosage of medication, a new medication or surgery). Early relapse was defined as relapse with a new onset of symptoms in less than three months after remission. Steroid refractoriness was defined as a requirement for steroid doses greater than 0.75 mg/kg/day of prednisolone per day 4 weeks after initiation of treatment. Recurrences were recorded according to the Rutgeerts’s scoring system, 9 and endoscopic and histological findings were recorded as explicitly indicated in the medical history. 7,8
Histopathological studies were considered positive if they mentioned the diagnosis explicitly in the report or if they reported some characteristic considered typical in the histological definitions of the European Consensus on the histopathology of IBD. 10
A descriptive analysis of the data registered in the BD Clinic was done with the IBM Statistical Package for the Social Sciences (SPSS) version 19. The median and interquartile range (IQR) were calculated for numerical variables while qualitative variables were frequently described. As this was a retrospective analysis of a review of medical records, unregistered variables were reported as no data in the results and were excluded from the analysis by variables.
Results
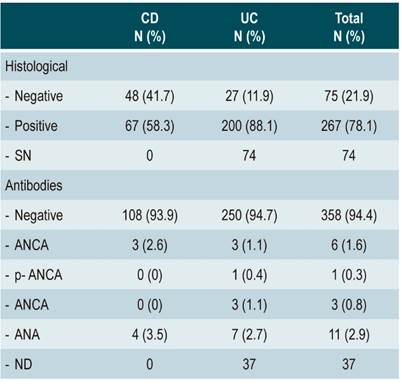
We included 416 participants: 115 (27.6%) with CD and 301 with UC (72.4%), with a ratio of 2.61 UC patients to 1 CD patient and a higher incidence of UC. The median age of CD patients was 43 years (IQR: 29 to 57 years). It was 42 for patients with UC (IQR: 30 to 55 years). Most were women who had similar frequencies of comorbidities. Less than 10% reported tobacco or alcohol use. Family histories of IBD were more frequent for CD. The average time between the first consultation and diagnosis was 9.29 months (IQR: 1 to 36 months) for CD and 6 months (IQR: 2 to 18 months) for UC. In total, 105 patients (32.5%) were hospitalized in general wards because of their illness and 38 (9.1%) were hospitalized at some point in the intensive care unit (ICU). Patients with CD were more likely to be hospitalized (Table 1).
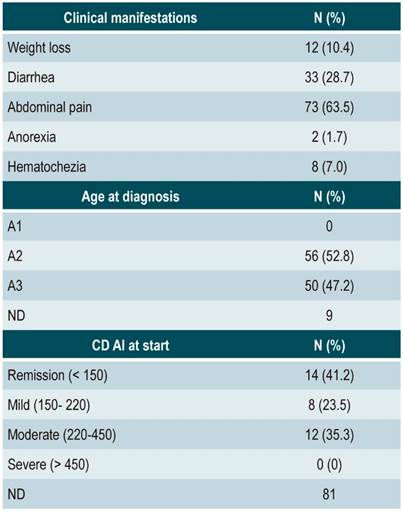
The majority of patients (94.4%) did not test positive for antibodies. The mean hemoglobin level in patients with CD was 12.3 g/dL (IQR: 6.7-16.9) while it 13 g/dL (IQR: 11-14) for UC patients. Histopathological samples were positive in 67 patients with CD (58.3%) and in 200 patients with UC (88.1%) (Table 2).
Table 1 Characteristics of the study population and hospital stays
* IBD in first degree relatives. ND: no data.
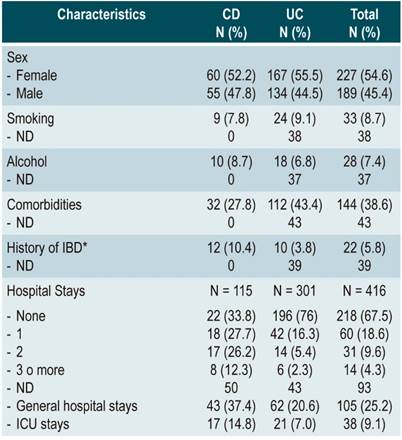
According to the Montreal Classification, 114 of the UC patients (53.3%) had ulcerative proctitis, 43 (20.1%) had left colitis, and 57 (26.6%) had pancolitis. The most common location of CD was ileal (54%) (Figure 1). At the initial consultation was 23 patients UC patients were asymptomatic in (10.7%), 105 (49.1%) had mild cases, 55 (25.7%) had moderate cases, and 31 (14.5 %) had severe cases. Almost half of the patients with CD (48.6%) had non-stenosing and non-penetrating behavior. Two patients (1.7%) had perianal disease, one classified as B2, the other classified as B3. Thirty-four patients (40%) presented fistulas (Figure 2).
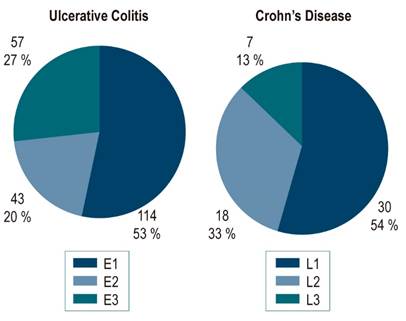
Figure 1 Extent of disease according to the Montreal classification. E1: ulcerative proctitis; E2: left colitis; E3: ulcerative pancolitis; L1: terminal ileum; L2: colon; L3: ileal colon. L4 was not included because there were no L4 patients in our study.
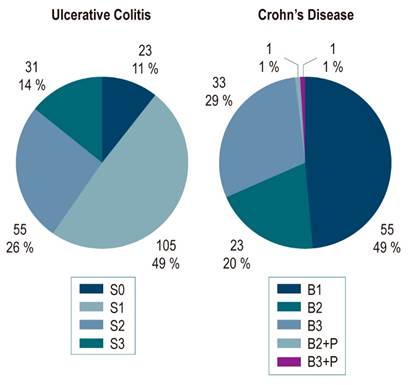
Figure 2 Severity of ulcerative colitis and behavior of Crohn’s disease according to the Montreal classification. S0: clinical remission; S1: mild; S2: moderate; S3: severe; B1: non-stenosing and non- penetrating; B2: stenosing; B3: penetrating; P: perianal.
The predominant clinical manifestation of CD was abdominal pain, followed by diarrhea. According to the CDAI classification, 41% of the patients had mild disease; 23.5% had moderate disease; and 35.29% had severe disease (Table 3). Extraintestinal manifestations were found in 28 patients with UC (10.3%) and in 33 patients with CD (44%). In both cases, the majority were articular (Figure 3). Adequate responses were found in 11 patients (25.6%) while it was inadequate in 32 patients (74.4%). Two (4.4%) had early relapses, and 8 (17.4%) were refractory to treatment. Twenty-four patients with UC (9.0%), and 53 with CD (46.1%) underwent some type of surgery related to their base diagnoses. Ileocecal resections were done in 11 patients with CD (9.5%) and colectomies were done in 6 (5.22%), with no reports of recurrences. Colectomies were performed in 16 patients with UC (6.67%) and were the most frequent surgical interventions. Only 1 patient with UC underwent a fistulectomy (4.16%).
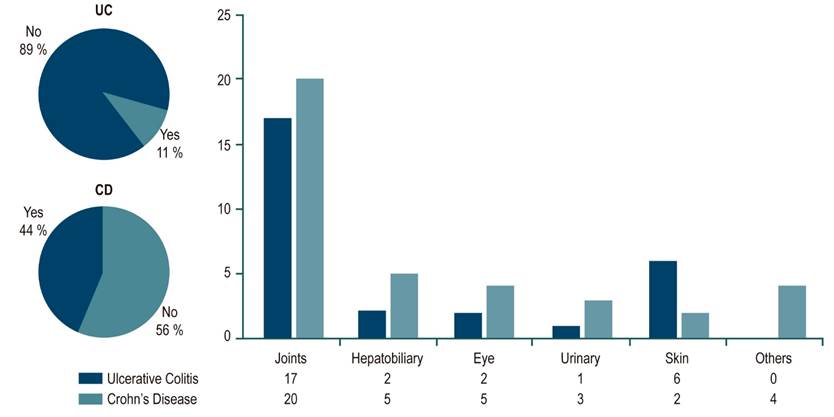
Figure 3 Extraintestinal manifestations. The pie charts show the distribution of patients with and without extraintestinal manifestations for ulcerative colitis and Crohn’s disease. The distribution of each type of manifestation is shown in the bar graph. UC: ulcerative colitis; CD: Crohn’s disease.
Of the patients diagnosed with CD, 23 (20%) were treated with steroids, 32 (27.82%) received azathioprine, 14 (12.17%) were given derivatives of 5-aminosalicylic acid (5-ASA), and 37 (32.17%) were treated with biological medicine. Of the patients diagnosed with UC, 85 (32.19%) received steroids, 65 (24.62%) received azathioprine, 224 (84.8%) received derivatives of 5-ASA and 42 (15.9%) received biological medicine (Figure 4).
Discussion
This study gathered 416 medical records of patients who had been diagnosed with IBD at a referral center in Cali and evaluated them retrospectively to determine their characteristics and natural histories. The proportion of patients with CD and UC (27.6% versus 72.3%) was similar to that reported in the Colombian series by Juliao (15.8% versus 80.7%), 5 Yepes (23.1% versus 76.9%), 6 and Reyes (24.2% versus 75.8%), 11 as well as to reports in the world literature. 12,13 The proportion reported in the first Colombian IBD series of 9.3% CD versus 90.7% UC) was striking but consistent with observations in countries where IBD is an emerging disease. 6,14 The median age at diagnosis in our study was similar to those reported by Reyes and other international series. 2,11,15,16
Of the 115 patients with CD, 32 (27.8%) had at least one comorbidity. There were six patients (5.21%) with both solid and hematological oncological diseases, five patients (4.34%) with arterial hypertension, and three patients (2.6%) with rheumatological diseases. Of the 301 patients with UC, 112 (43.4%) had and comorbidities: 30 (11.6%) had arterial hypertension, 18 (6.97%) had rheumatological diseases, 8 (3.1%) had oncological diseases (including two cases of colon cancer), and 7 (2.71%) had psychiatric diseases (including four cases of depression). The lower prevalence of psychiatric disorders in our population than those reported in other series was striking. 17,18
A first-degree relative had a history of IBD in 10.4% of our patients with CD and in 3.8% of our patients with UC. A Danish study established family histories IBD among 12.2% of new CD cases and among 8.8% of new UC cases. 19 Interestingly, a metaanalysis reported a higher frequency of IBD family histories among UC patients (12%) than among CD patients (2%). 20
Most of the variables recorded in this study were more severe among CD patients than among UC patients. More than half of the UC patients (53.3%) had disease limited to the rectum while 26.6% had pancolitis. This is in line with previous Colombian studies but differs from studies elsewhere which show that the frequency of pancolitis has increased. 5,6, In several countries it is the most frequent manifestation. 21-23 Something similar has occurred in patients with CD. Only 12.7% of our patients had ileocolonic disease, while a frequency close to 50% has been reported in the literature. Of our UC patients, 49.7% had mild cases, 25.7% had moderate cases, and 14.5% were severe. For CD patients these frequencies were 41.17%, 23.5% and 35.3%, respectively. No CD patients were in remission while 10.7% of UC patients were asymptomatic. Hospitalization and ICU admissions were both more frequent for CD patients than for those with UC. Extraintestinal manifestations were also more frequent in CD patients. These frequenciea coincide with those reported in the literature.
CD took longer to diagnosis in our medical center than did UC: on average 9.2 months versus 6.0 months. This is consistent with what has been published in Colombian studies although these times are greater than those reported in the international literature. An Italian multicenter study found diagnostic delay for CD was 7.1 months while it was only two months for UC. Delays were longer in a historical cohort than in a modern one. 24 A South Korean study showed that surgery was required more often by patients with longer diagnostic delays than by other patients. 25 The presence of autoantibodies was very low compared to countries with a higher incidences of IBD such as Japan. 26 In our center, 58.3% of the patients with CD and 88.1% of the patients with UC had some typical histological finding or were reported as positive for the diagnosis in question. Comparison of these findings with those of other authors is difficult due to the lack of standardization in the reporting of histopathological specimens from patients with IBD. A Brazilian study suggests that standardization of histopathological diagnoses could result in a higher percentage of conclusive diagnoses, especially for CD. 27
The proportions of our patients who received biological drugs is similar to that registered in a recent series in the Colombian population, 35% for CD and 16% for UC. 11 It seems their use is increasing as demonstrated in an economic study that reported that the percentage of CD patients receiving biologicals increased from 21.8% to 43.8% while that of UC patients increased from 5.1% to 16.2% from 2007 to 2015. 28
In our population there was a notable difference in the percentages of CD and UC patients who underwent abdominal surgery: 46.1% of the CD patients required surgery, but only 9.0% of the UC patients did. Even when appendectomies are excluded, 33% of CD patients underwent abdominal surgery. Excluding appendectomies, the most frequent operations were ileocecal resections in CD patients (9.5%) and colectomies in UC patients (6.67%). Colectomies were performed in 5.22% of CD patients. The frequency of intervention in our study was higher than that reported by Reyes (27.5% versus 4.8%) and similar to that published by Juliao (50% versus 5.9%) in Colombian populations, but it is lower than those reported in studies with high-frequency populations which range between 37.9% and 50% for CD and between 8.3% and 32.4% for UC. 13,29,16,30 In this study there were no reports of postoperative recurrence even though the reported rate is around 80%. 31
IBD increasingly affects the Colombian population, so it has become imperative for us to gain a better understanding of this disease and its behavior in our environment. Early diagnosis, especially of CD, continues to be a very important challenge, not only for our center but for everyone in the country. UC was less severe in our patients than in cases reported elsewhere in the world, but this did not occur in patients with CD which could be related to diagnostic delay. The proportion of patients treated with biological medicines is getting closer and closer to proportions reported in the first world. This will bring clinical and quality of life benefits to our patients. It is difficult to determine whether the lower rates of surgery are due to better clinical responses or to poorer access to these interventions. More studies should be carried out in our population to continue characterizing the phenotype of the disease and its long-term evolution, as the incidence in our environment increases and new therapeutic options become available.
REFERENCES
1. Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW, Kaplan GG. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(1):46-54.e42. https://doi.org/10.1053/j.gastro.2011.10.001 [ Links ]
2. Figueroa CC, Quera PR, Valenzuela EJ, Jensen BC. Enfermedades inflamatorias intestinales: Experiencia de dos centros chilenos. Rev Med Chil. 2005;133(11):1295-304. https://doi.org/10.4067/S0034-98872005001100004 [ Links ]
3. Kamm MA. Rapid changes in epidemiology of inflammatory bowel disease. Lancet. 2017;390(10114):2741-2. https://doi.org/10.1016/S0140-6736(17)32669-7 [ Links ]
4. Lega-Siccar J, Lega LI. Colitis ulcerativa y enfermedad de Crohn del colon. Acta Médica Colomb. 1991;16(3):140-52. [ Links ]
5. Juliao-Baños F, Ruiz-Vélez MH, Flórez-Arango JF, Donado-Gómez JH, Marín-Zuluaga JI, Monsalve-Arango C, Jiménez-Gómez CA, Agudelo-Zapata Y, Velayos FS. Fenotipo e historia natural de la enfermedad inflamatoria intestinal en un centro de referencia en Medellín-Colombia. Rev Colomb Gastroenterol. 2010;25(3):240-51. [ Links ]
6. Yepes-Barreto IJ, Carmona R, Díaz F, Marín-Jiménez I. Prevalencia y características demográficas de la enfermedad inflamatoria intestinal en Cartagena, Colombia. Rev Colomb Gastroenterol. 2010;25(2):107-11. [ Links ]
7. Silverberg M, Satsangi J, Ahmad T. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: Report of a Working Party of the 2005 Montreal World Congress of Gastroenterology . Can J Gastroenterol. 2005;19(Suppl A):5-36. https://doi.org/10.1155/2005/269076 [ Links ]
8. Best W, Becktel J, Singleton J, Kern F. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology. 1976;70(3):439-44. https://doi.org/10.1016/S0016-5085(76)80163-1 [ Links ]
9. Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn’s disease. Gastroenterology. 1990;99(4):956-63. https://doi.org/10.1016/0016-5085(90)90613-6 [ Links ]
10. Magro F, Langner C, Driessen A, Ensari A, Geboes K, Mantzaris GJ, Villanacci V, Becheanu G, Borralho Nunes P, Cathomas G, Fries W, Jouret-Mourin A, Mescoli C, de Petris G, Rubio CA, Shepherd NA, Vieth M, Eliakim R; European Society of Pathology (ESP); European Crohn’s and Colitis Organisation (ECCO). European consensus on the histopathology of inflammatory bowel disease. J Crohn’s Colitis. 2013;7(10):827-51. https://doi.org/10.1016/j.crohns.2013.06.001 [ Links ]
11. Reyes GA, Gil FL, Carvajal GD, Sánchez CB, Aponte DM, González CA, Gamba JI, Preciado JA, Marulanda JC, Sabbagh LC. Enfermedad inflamatoria intestinal: características de fenotipo y tratamiento en un hospital universitario de Bogotá. Rev Col Gastroenterol. 2018;117-26. https://doi.org/10.22516/25007440.196 [ Links ]
12. Höie O, Wolters F, Riis L, Aamodt G, Solberg C, Bernklev T, Odes S, Mouzas IA, Beltrami M, Langholz E, Stockbrügger R, Vatn M, Moum B; European Collaborative Study Group of Inflammatory Bowel Disease (EC-IBD). Ulcerative colitis: Patient characteristics may predict 10-yr disease recurrence in a European-wide population-based cohort. Am J Gastroenterol. 2007;102(8):1692-701. https://doi.org/10.1111/j.1572-0241.2007.01265.x [ Links ]
13. Wolters FL, Russel MG, Sijbrandij J, Ambergen T, Odes S, Riis L, Langholz E, Politi P, Qasim A, Koutroubakis I, Tsianos E, Vermeire S, Freitas J, van Zeijl G, Hoie O, Bernklev T, Beltrami M, Rodriguez D, Stockbrügger RW, Moum B. Phenotype at diagnosis predicts recurrence rates in Crohn’s disease. Gut. 2006;55(8):1124-30. https://doi.org/10.1136/gut.2005.084061 [ Links ]
14. Argüello M, Archila P, Sierra F, Otero W. Enfermedad inflamatoria intestinal. Rev Col Gastroentol. 1991;6(4):237-72. [ Links ]
15. Ka-Ho L, Hiu-Gong H, Chi-Ho N. Epidemiology and clinical characteristics of ulcerative colitis in Chinese population: Experience from a single center in Hong Kong. J Gastroenterol Hepatol. 2008;23(3):406-10. https://doi.org/10.1111/j.1440-1746.2007.05079.x [ Links ]
16. Langholz E, Munkholm P, Davidsen M, Binder V. Course of ulcerative colitis: analysis of changes in disease activity over year. Gastroenterology. 1994;107(1):3-11. https://doi.org/10.1016/0016-5085(94)90054-x [ Links ]
17. Larion S, Tavakoli H, Dececchis D, Arnold J, Vanslyke J. Psychiatric comorbidities in inflammatory bowel disease. Curr Psychiatry Rev. 2015;11(2):124-9. https://doi.org/10.2174/157340051102150502083333 [ Links ]
18. Goodhand JR, Wahed M, Mawdsley JE, Farmer AD, Aziz Q, Rampton DS. Mood disorders in inflammatory bowel disease: Relation to diagnosis, disease activity, perceived stress, and other factors. Inflamm Bowel Dis. 2012;18(12):2301-9. https://doi.org/10.1002/ibd.22916 [ Links ]
19. Trier Moller F, Andersen V, Andersson M, Jess T. Hospital admissions, biological therapy, and surgery in familial and sporadic cases of inflammatory bowel disease: A population-based cohort study 1977-2011. Inflamm Bowel Dis . 2015;21(12):2825-32. https://doi.org/10.1097/MIB.0000000000000545 [ Links ]
20. Childers RE, Eluri S, Vazquez C, Weise RM, Bayless TM, Hutfless S. Family history of inflammatory bowel disease among patients with ulcerative colitis: A systematic review and meta-analysis. J Crohn’s Colitis. 2014;8(11):1480-97. https://doi.org/10.1016/j.crohns.2014.05.008 [ Links ]
21. Ng S, Tang W, Ching J. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-Pacific Crohn’s and colitis epidemiology study. Gastroenterology. 2013;145(1):158-65. https://doi.org/10.1053/j.gastro.2013.04.007 [ Links ]
22. Lakatos L, Kiss LS, David G, Pandur T, Erdelyi Z, Mester G, Balogh M, Szipocs I, Molnar C, Komaromi E, Lakatos PL. Incidence, disease phenotype at diagnosis, and early disease course in inflammatory bowel diseases in Western Hungary, 2002-2006. Inflamm Bowel Dis . 2011;17(12):2558-65. https://doi.org/10.1002/ibd.21607 [ Links ]
23. Nuij V, Zelinkova Z, Rijk M. Phenotype of inflammatory Netherlands: Bowel disease at diagnosis in the Delta, a population-based inception cohort study (the Delta Cohort). Inflamm Bowel Dis . 2013;19(10):2215-22. https://doi.org/10.1097/MIB.0b013e3182961626 [ Links ]
24. Cantoro L, Di Sabatino A, Papi C, Margagnoni G, Ardizzone S, Giuffrida P, Giannarelli D, Massari A, Monterubbianesi R, Lenti MV, Corazza GR, Kohn A. The time course of diagnostic delay in inflammatory bowel disease over the last sixty years: An Italian multicentre study. J Crohns Colitis. 2017;11(8):975-80. https://doi.org/10.1093/ecco-jcc/jjx041 [ Links ]
25. Lee DW, Koo JS, Choe JW, Suh SJ, Kim SY, Hyun JJ, Jung SW, Jung YK, Yim HJ, Lee SW. Diagnostic delay in inflammatory bowel disease increases the risk of intestinal surgery. World J Gastroenterol. 2017;23(35):6474-81. https://doi.org/10.3748/wjg.v23.i35.6474 [ Links ]
26. Mitsuyama K, Niwa M, Takedatsu H, Yamasaki H, Kuwaki K, Yoshioka S, Yamauchi R, Fukunaga S, Torimura T. Antibody markers in the diagnosis of inflammatory bowel disease. World J Gastroenterol . 2016;22(3):1304-10. https://doi.org/10.3748/wjg.v22.i3.1304 [ Links ]
27. Svoboda Baldin RK, Telles JEQ, Bonardi RA, Amarante HMB dos S, Júnior AB. Do standardization and quantification of histopathological criteria improve the diagnosis of inflammatory bowel disease? J Bras Patol e Med Lab. 2014;50(3):221-8. https://doi.org/10.5935/1676-2444.20140019 [ Links ]
28. Shi HY. Market share and costs of biologic therapies for inflammatory bowel disease in the USA. Aliment Pharmacol Ther. 2018 ;47(3):364-70. https://doi.org/10.1111/apt.14430 [ Links ]
29. Romberg-Camps MJ, Dagnelie PC, Kester AD, Hesselink-van de Kruijs MA, Cilissen M, Engels LG, Van Deursen C, Hameeteman WH, Wolters FL, Russel MG, Stockbrügger RW. Influence of phenotype at diagnosis and of other potential prognostic factors on the course of inflammatory bowel disease. Am J Gastroenterol . 2009;104(2):371-83. https://doi.org/10.1038/ajg.2008.38 [ Links ]
30. Solberg IC, Lygren I, Jahnsen J, Aadland E, Høie O, Cvancarova M, Bernklev T, Henriksen M, Sauar J, Vatn MH, Moum B; IBSEN Study Group. Clinical course during the first 10 years of ulcerative colitis: results from a population-based inception cohort (IBSEN Study). Scand J Gastroenterol. 2009;44(4):431-40. https://doi.org/10.1080/00365520802600961 [ Links ]
31. Bailey EH, Glasgow SC. Challenges in the medical and surgical management of chronic inflammatory bowel disease. Surg Clin North Am. 2015;95(6):1233-44. https://doi.org/10.1016/j.suc.2015.08.003 [ Links ]
Received: May 27, 2019; Accepted: October 15, 2019











 texto em
texto em