Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957versão On-line ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.2 Bogotá abr./jun. 2020
https://doi.org/10.22516/25007440.262
Review articles
Is the videocapsule endoscopy the best option for diagnosis of possible bleeding from the small intestine?
1 Médico cirujano. Residente de medicina interna, Facultad de Medicina, Universidad Nacional de Colombia. Bogotá D. C., Colombia
2 Profesor de Medicina, Unidad de Gastroenterología, Universidad Nacional de Colombia, Hospital Universitario Nacional de Colombia. Bogotá D. C., Colombia
When neither upper nor lower gastrointestinal endoscopy can find a clear cause of gastrointestinal bleeding, it will eventually be found in the small intestine in up to 77% of cases. Given the excellent diagnostic performance of video capsule endoscopy for studying this segment of the gastrointestinal tract, the question of whether it should become the initial diagnostic method for patients with possible bleeding from the small intestine arises. The alternatives are to perform additional upper and lower endoscopic procedures or to use some alternative method of studying the small intestine. This review documents and evaluates the superior diagnostic performance and greater safety of videocapsule endoscopy as the initial approach for possible bleeding from the small intestine and compares it with other methods. However, the cost-effectiveness of this approach, clearly demonstrated elsewhere, is questioned in our setting.
Keywords: Digestive endoscopy; capsule endoscopy; gastrointestinal hemorrhages; small intestine
En pacientes sin una causa clara de sangrado gastrointestinal luego de una endoscopia digestiva alta y baja, la causa se encontrará en el intestino delgado hasta en el 77 % de los casos. Ante el excelente rendimiento diagnóstico de la videocápsula endoscópica (VCE) para el estudio de este segmento del tracto gastrointestinal, surge la duda de si debería ser el método diagnóstico inicial de este grupo de pacientes con posible sangrado del intestino delgado (PSID) o si la realización de una nueva endoscopia alta y baja o algún método alternativo de estudio del intestino delgado debería serlo. En esta revisión se evalúa y evidencia el rendimiento diagnóstico superior y la mayor seguridad de la VCE como abordaje inicial de pacientes con PSID en relación con otros métodos. Sin embargo, se pone en tela de juicio la mejor costo-efectividad de este abordaje en nuestro medio, que en otros ha sido claramente demostrada.
Palabras clave: Endoscopía del sistema digestivo; endoscopia por cápsula; hemorragia gastrointestinal; intestino delgado
Introduction
Two to ten percent of gastrointestinal bleeding occurs in the small intestine, 1,2,3 but 77% of cases not identified by upper gastrointestinal endoscopy (esophagogastroduodenoscopy - EGD) and total colonoscopy are located in the small intestine. 4-7
In the past, when initial endoscopic examinations did not find the etiology of bleeding, the condition was called obscure gastrointestinal bleeding (OGIB). 8 OGIB could be designated as occult GI bleeding in cases of iron deficiency anemia or occult blood detected in the stool, or it could be designated as manifest GI bleeding when there were clinical manifestations of bleeding such as melena, rectal bleeding or hematochezia. 8 Currently the nomenclature has changed: when endoscopic procedures are negative, the condition is called potential small bowel bleeding (SBB). The term OGIB is now reserved for situations in which EGD, total colonoscopy and other tests that evaluate the small intestine are negative. 9
The most common causes of SBB are angiectasis (20% -55%), especially in the elderly, followed by tumors (10% -20%) and Crohn’s disease (CD) (2% - 10%). 10 Other less common causes include celiac disease, Meckel’s diverticulum, non-steroidal anti-inflammatory drugs (NSAIDs) enteropathy, Dieulafoy’s lesion, ectopic varices, portal hypertensive enteropathies, and radiation enteritis. 10
The small intestine can be evaluated with various methods including enteroscopies, magnetic resonance enterography (MRE) and video capsule endoscopy (VCE). 9 Since introduction, VCE has facilitated evaluation of the small intestine and is currently considered the test of choice for the study of diseases in this segment. 11,12 Nevertheless, several authors and guidelines recommend repeating EGD and total colonoscopy before using VCE to study the small intestine study in some patients with suspected SBB. 9,13 This approach arises from studies of patients which used different methods to evaluate the small intestine which found that the cause of bleeding was within the reach of EGD or total colonoscopy in 2% to 25% of cases and in 6% to 23% of cases, respectively. 14-16 Colombian publications also recommend this approach. 17 However, this approach is controversial, and a number of authors, including some from our country, consider VCE to be the first line of evaluation for this group of patients. 10,18,19
The objective of this review is to describe and evaluate the usefulness of VCE as the study of choice for suspected SBBfollowing negative results from upper and lower endoscopic examination and to compare VCE with the more traditional approach of second upper and lower endoscopic examinationsas well as with other methods of evaluation of the small intestine.
Methodology
A bibliographic search was carried out in the PubMed database for 5 years to May 14, 2018. The following terms and methodology were used: “((((Capsule Endoscopes OR Capsule Endoscope OR Endoscope, Capsule OR Endoscopes, Capsule OR Video Capsule Endoscopes OR Capsule Endoscope, Video OR Capsule Endoscopes, Video OR Endoscope, Video Capsule OR Endoscopes, Video Capsule OR Video Capsule Endoscope))) AND ((Endoscopy, Digestive System OR Digestive System Endoscopies OR Digestive System Endoscopy OR Endoscopies, Digestive System OR Digestive System Endoscopic Surgical Procedures OR Endoscopic, Digestive System, Surgery OR Endoscopic, Digestive System, Surgical Procedure OR Procedure, Digestive System, Endoscopic, Surgical OR Surgical Procedures, Endoscopic, Digestive System OR Procedures, Digestive System, Endoscopic, Surgical OR Procedures, Endoscopic , Digestive System, Surgical OR Surgery, Digestive System Endoscopic OR Surgery, Endoscopic, Digestive System OR Surgical Procedure, Endoscopic, Digestive System OR Digestive System Endoscopic Surgery OR Procedure, Endoscopic, Digestive System, Surgical OR Esophagogastroduodenoscopy OR Eso-phagogastroduodenoscopies OR Colonoscopy OR Colonoscopies OR Colonoscopic Surgical Procedures OR Colonoscopic Surgical Procedure OR Procedure, Colonoscopic Surgical OR Surgical Procedures OR Colonoscopic Surgical Procedure, Surgical OR Procedures , Colonoscopic OR Surgery, Colonoscopic OR Surgical Procedures, Colonoscopic OR Colonoscopic Surgery OR Colonoscopic Surgeries OR Surgeries, Colonoscopic)))) AND ((((Intestine, Small OR Intestines, Small OR Small Intestines OR Small Intestine OR Duodenum OR Ileum OR Jejunum OR Small Bowel))) AND ((Hemorrhage OR Hemorrhages OR Bleeding)))”. The presence in the title or abstract for each of the search terms was specified without date limits and only in the Spanish or English languages. Subsequently, the titles and abstracts of all the results were reviewed to identify articles the authors believed deserved complete review. In addition, some references from selected articles selected and other articles and guidelines of which the authors were aware were reviewed.
Results
VCE
VCE was conceived more than 30 years ago and subsequently developed simultaneously and independently by an Israeli and an English group. 20-22 Since then it has become an excellent method of visualizing the gastrointestinal tract, especially the small intestine and especially when other methods have poor diagnostic yields or logistical problems. 17,23 Technological refinement has not ceased since conception, and new models allow better yields and offer different utilities. 11,24,25. There are currently anumber of models available for examining different gastrointestinal segments. Of these, PillCam (GivenImaging®; Yoqneam, Israel) was the first and has been studied most (Table 1) 26.
Table 1 Endoscopic video capsules available in the market 22
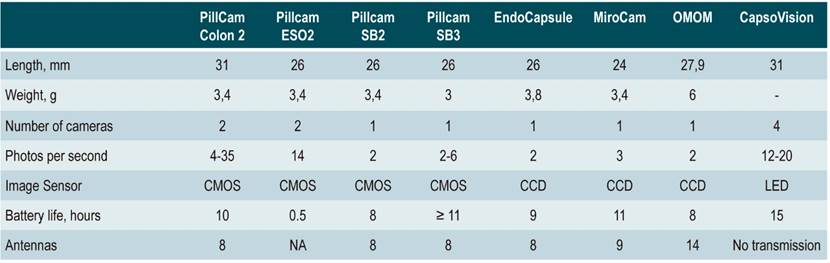
CCD: charge coupled device; CMOS: complementary metal oxide semiconductor; ESO: esophagus; LED: light emitting diode; SB: small bowel. Modified from: Gerber J et al. Gastrointest Endosc. 2007; 66 (6): 1188-95.
Over the years, viewing of the small intestine by VCE has found numerous diagnostic and monitoring applications for pathologies such as CD, celiac disease, small intestine tumors and NSAID-induced enteropathies. 27-30 VCE can also identify the cause of iron deficiency anemia in up to 66% of those patients whose anemia has no apparent cause. 31-33 In the last decade its use has expanded, and it has even been suggested as a strategy for colorectal cancer screening and diagnosis of Barrett’s esophagus and esophageal varices. 26,34-40 More recently, the possibility of using real-time intraoperative VCE as a therapeutic instrument for treating digestive tract bleeding has been studied. 41 Making these gains will depend on achievement of necessary technological refinements which is currently a focus of intense research. 11,25
In 2003, the Food and Drug Administration (FDA) designated VCE the first line method for intraluminal study of the small intestine due to its high sensitivity. Previously, the FDA had indicated it be used only as a coadjuvant diagnostic method. 12 In 2006, the technology committee of the American Society for Gastrointestinal Endoscopy (ASGE) concluded that VCE outperformed contrast-enhanced radiographic studies and push enteroscopy in evaluating suspected SBB. 33 Since then, there has been insistence that it be the method of choice for displaying the small intestine after ruling out upper and lower GI tract bleeding. 13,33,42 Some even consider it to be the gold standard for diagnosing suspected SBB. 23,43 Suspected SBBis currently the most common indication for VCE (66%). 11,44 The possibility of finding the cause of bleeding in the small intestine in these patients ranges between 35% and 77% depending on whether the bleeding is occult or overt. 6 A series of 100 patients with suspected SBBfound the cause of bleeding in 12% of patients with prior overt bleeding, in 44% of patients with fecal occult blood and iron deficiency anemia, and in 92% of patients with current overt bleeding. 45
VCE Evaluation of the Small Intestine Compared to Repeatition of Upper and Lower Endoscopy
When upper and lower endoscopic examination cannot find the source of GI tract bleeding, the possibility that the source is in the small intestine becomes greater than that it is in the upper or lower gastrointestinal tract (Table 2). 10 Therefore, the small intestine has been considered the next organ to be studied. This has been corroborated by comparison of the frequency with which causes of bleeding are found in patients who undergo VCE with this frequency among those who undergo a second EGD and total colonoscopy. An Australian study found that repeating EGD and total colonoscopy found only one missed lesion (4% of patients) while VCE found probably or potentially causative lesions in at least 62%. 18
Table 2 Causes of bleeding in suspected SBB(10)
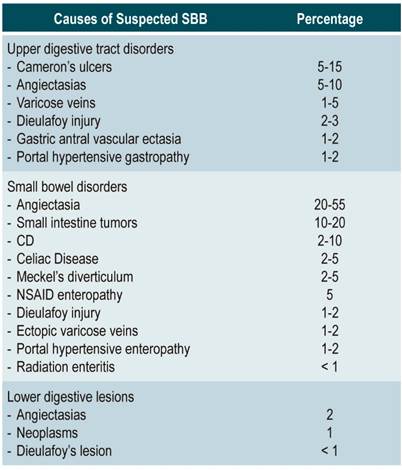
Modified from: Liu K et al. Aliment Pharmacol Ther. 2011; 34 (4): 416-23.
On the other hand, it has been found that the push enteroscopy identifies lesions in cases of suspected SBBthat were within the scope of the EGD in 10% to 64% of cases. 14,15,46,47 Double balloon enteroscopy (DBE) identifies lesions within the scope of an EGD in 24% to 25% of cases within the scope of an EGD and in 7% of the cases within the scope of a total colonoscopy. 5,48 VCE finds lesions within the reach of an EGD in 2% to 14% of patients. 45,49-55 However, it is necessary to take into account two fundamental issues. First, the performance of VCE and other methods of studying small intestine continues to be greater than a second endoscopy in almost all scenarios. 18,42 Second, although these lesions were within the reach of a second try at endoscopy, they were not found with endoscopy but with an alternative method.
Among the variables explaining the diagnostic yield of VCE is the fact that it does not use insufflation and does not distend gastrointestinal segments. Consequently, it becomes physiological endoscopy which has a greater chance of identifying lesions such as vascular ectasias which conventional endoscopy usually cannot identify. Similarly, visualization of many of these lesions requries perseverance, dedication and time. Busy endoscopists often do not have enough time to thoroughly inspect the stomach, including adequate retrovision. In the case of the colon, they may not be sure that they have actually reached the cecum. 42,51
In 2010, the American Society for Gastrointestinal Endoscopy recommended repeating EGD in cases of suspected SBBwhen there was suspicion of upper GI bleeding and repeating colonoscopy in cases when there was suspicion of lower GI bleeding, but proceeding immediately to VCE if neither was suspected. 56 However, it also indicated VCE was a reasonable first option in most cases. 56 Other authors have suggested repeating the upper and lower endoscopies only if the endoscopist is aware that adequate visualization of the upper or lower digestive tract had not been achieved. 10
The European Society for Gastrointestinal Endoscopy published an update of its guidelines in 2006, in which it ambiguously suggests that VCE is the method of choice for suspected SBB. 57 Finally, the most recent 2015 guidelines from the American College of Gastroenterology (ACG) on the diagnosis and management of SBB recommend repeating EGD in cases of suspected SBB if the patient presented melena or hematemesis and if the first EGD did not adequately visualize the mucosa. It recommended repeating colonoscopy if there was recurrent hematochezia, suspicion of lower intestinal origin, or if inspection of the mucosa in the first colonoscopy was inadequate. 57 However, the guideline authors recognized that these recommendations were based a “low” or “very low” levels of evidence and were based on findings of causes of suspected SBB that were within the scope of conventional endoscopic methods of studying the small intestine. 5,14,15,45-55 Similarly, these guidelines suggest proceeding directly to VCE if the indications described for the second endoscopy do not exist. 9. However, the lack of evidence is manifested by recognition within the text of those guidelines that push enteroscopy can be considered instead of a second EGD and that VCE can be used without a second endoscopy to speed up the approach. This course is even more important given that a second endoscopy is not cost-effective. 9
Video Capsules vs. Push Enteroscopy
A 2005 publication compared performance of VCE against push enteroscopy in the seven prospective studies published to that date on suspected SBB. It found that the diagnostic yield of VCE was 71% versus 29% for push enteroscopy. 58 A metaanalysis from the same year that included 14 studies found a yield of 63% for VCE and only 28% for push enteroscopy. 3 A second metaanalysis covering 17 studies found a 37% difference in favor of VCE in suspected SBB cases over other methods. Push enteroscopy was the main comparator. 59 The odds ratio (OR) of a positive finding from VCE 4.3 (95% confidence interval: 3.1 to 6.0). 59 More recently, a randomized study confirmed these findings with the cause of SBB identified in 50% of the cases with VCE and in 24% with push enteroscopy (p = 0.02). 60
Saurin et al. 61 used final clinical diagnoses as the gold standard. They found that VCE had a sensitivity and specificity of 92% and 48%, respectively, compared to 80% and 69% for push enteroscopy.
Video Capsule Performance versus Double Balloon Enteroscopy (DBE)
Some small studies have directly compared VCE and DBE. One of them, which included 13 patients, found the diagnostic value for suspected SBB was similar for the two methods. 62 A subsequent metaanalysis covering 227 patients compared the two methods and found that VCE detected more causes than DBE when the latter was not done by combining the anal and oral approaches (OR: 1.61; 95 CI %: 1.07-2.43), but less when the combined DBE approach was used. 63 However, a study from the same year concluded that VCE resulted in an etiological diagnosis more frequently than DBE by combined anal and oral approach (59% vs 42%) although the difference was not statistically significant (p = 0.30). This was probably due to the small number of patients (n = 32). 64 In general, the performance of both methods is considered similar, but VCE has the advantage that it is a non-invasive method with fewer side effects. 13,65-67
Video Capsule versus Intraoperative Enteroscopy (IOE)
Some consider intraoperative enteroscopy (IOE) to be the best method for fully studying the small intestine and the one with the highest etiological yield (58% to 88%). 9,68 There are only a few studies that compare VCE with IOE. One of the studies that stands out is that of Hartmann et al. 69 VCE found the cause of bleeding in 74% of cases compared to 72% with IOE without statistically significant differences. In the aforementioned metaanalysis by Triester et al., 3 a single study comparing the two methods was found. It concluded that their yields were similar performance (83%) but that VCE should be the preferred method since it is non-invasive and lacks the complications and risks of IOE. 17,69
Video Capsule versus Other Methods
Some small studies have found that VCE more frequently identify causes of bleeding than does computerized axial tomography (CT) enteroclysis (n = 8) (70) or magnetic resonance imaging (MRI) enteroclysis (n = 14). 71 Conventional enteroclysis’ diagnostic yield ranges from 0% to 21%. 72-75 The previously mentioned metaanalysis found three studies that compared VCE with conventional enteroclysis. VCE found a possible cause in 67% of cases while conventional enteroclysis found potential causes in only 8%. 3 Similarly, it has been calculated that VCE allows treatment to be modified in 66% of patients with suspected SBB while conventional enteroclysis allows modification in only 10% of cases. 76,72 This comparison’s validity is limited because these studies were in different populations. The superiority of VCE over standard angiography has also been demonstrated by yields of 53% and 20%, respectively. 77 Saperás et al. found that VCE had a 72% yield while CT angiography’s yield was only 24%, and with standard angiography’s was 56%. 78
Disadvantages of Video Capsules
The most important potential complication of VCE is retention in the gastrointestinal tract. 44 This can occur due to scars, masses and other causes of lumen stenosis. At present, there is no adequate way to predict it with certainty except for of signs and symptoms suggestive of intestinal obstruction. 17,19 VCE retention occurs in 0% to 21% of patients depending on the population. It is most frequent in cases of CD. 13,59,80 In case of clinical suspicion of retention risk, either CT enteroclysis or MRI enteroclysis is recommended. These imaging methods can evaluate the risk of “patency” and identify any stenosis. Nevertheless, spontaneous disintegration of the capsule does not constitute emergency total obstruction of the small intestine. 13,81
Other potential adverse events are related to technical difficulties. They include capsule malfunction due to battery problems and data transfer problems. 76,82-84 In cases of delayed gastric emptying, the capsule can remain in the stomach for a long time with unnecessary drain on the battery. In these cases, the battery can completely lose its charge before the small intestine is fully examined. 82,83 Since the capsule does not insuflate air, it does not have the ability to distend the small intestine and cannot adequately expose the mucosal surface of some areas. Consequently, VCE cannot identify lesions at these sites. 13,22. An inherent limitation of VCE is that it is still currently a diagnostic method that cannot be used to take biopsy samples or for performing therapeutic interventions. 13 Contraindications include pregnancy (there is no research about this group) and swallowing problems due to the risk of tracheal aspiration. When there are swallowing problems it is necessary to advance the capsule endoscopically. 6,26
Despite these limitations, VCE is the safest of the methods with similar yields for evaluating the small intestine. For example, postoperative IOE complications include mesenteric vessel damage, prolonged ileus, hematomas, infections, perforations, and even mortality. 17,69 Similarly, DBE’s invasive nature means that patients’ do not tolerate it as well, and it requires sedation or anesthesia. It is currently recommended only when VCE has found lesions that can be treated with DBE, when biopsies are required, and if VCE finds no problems but suspicion of SBB persists. 65-67,85-87
Video Capsule Cost-effectiveness Compared to Second Upper and/or Lower Endoscopy
One variable that can help decide between these two strategies is cost. A retrospective study carried out in Greece evaluated the performance of VCE in suspected SBB and concluded that it is more cost-effective than repeating EGD and total colonoscopy. 42 Performing a new EGD and total colonoscopy on all patients would have cost € 50,050 (143 patients x € 350) which would have avoided 9 unnecessary VCEs. The necessary VCEs cost € 80,400 for the (134 patients X € 600) for a € 130,450 total with this strategy. The reverse strategy, with VCE performed on all patients, had a cost of € 85,800 (143 patients x € 600). This represents a saving of € 312.20 per patient. It should be noted that these patients had been evaluated in the past on average with 2 EGDs (Range 1-3) and 2 colonoscopies (Range 1-3), so it cannot be ruled out that more causes within the reach of these traditional methods might have been found.
An attempt could be made to extrapolate these data to local costs for these diagnostic methods even though there are clear limitations of this type of extrapolation. For our calculations, we used the rates that the Hospital Universitario de la Universidad Nacional offers to entities that refer patients: EGD with sedation: COP (Colombian pesos) 375,000, total colonoscopy with sedation: COP 413,000 and VCE: COP 6,000,000. Initial EGD and total colonoscopy followed by second repititions followed by VCE in cases of no findings would have a cost of COP 916,684,000 (143 X COP 788,000 + 134 X COP 6,000,000) while initial performance of VCE alone on all patients would cost COP 858,000,000 (143 X COP 6,000,000) which represents a savings of $ 410,377.60 per patient.
In the Australian study mentioned previously, a higher cost was also found for the strategy of repeating the upper and lower endoscopy and, in case of no findings, proceeding to VCE than for initial use of VCE alone for all patients. 18 Fifty patients were evaluated using first strategy with both endoscopies ($ 1,273.00 per patient) and 47 patients were evaluated using VCE alone ($ 1,801.90 per patient). Fifty VCEs were performed and, at most, 26 new upper and lower endoscopies. This led to a total cost of $ 148,364.00 with a second upper and lower endoscopy, while the cost was $ 123,199 with VCE alone which represents a savings of $ 503,000 per patient. If the findings of this study were extrapolated to the costs of our institution, the initial strategy of a new EGD and total colonoscopy would cost COP 321,400,000 (50 X COP 788,000 + 47 X COP 6,000,000), while the strategy with initial VCE followed by new endoscopies in case of no findings would cost COP 320,488,000 (50 X COP 6,000,000 + 26 X COP 788,000). In this case, there would be a saving of COP 18,240 per patient with VCE as the initial strategy.
A third international study conducted in Italy also found that VCE was more cost-effective for diagnosing suspected SBB that other methods for evaluating these patients including PE, enteroclysis, EGD, colonoscopy, CT scans, angiography, MRI, ultrasound, scintigraphy, and IOE. 43 The average cost of VCE to reach a diagnosis was € 2,091 while the average cost for the other methods was € 3,829.
In Colombia, no studies have yet compared the different methods of investigating suspected SBB much less their cost-effectiveness. However, two retrospective case series describing the use of VCE to diagnose suspected SBB, one with 97 patients and the other with 50 patients, have been published. 19,88 In these studies, the cause of bleeding was identified in 91.7% (89/97) and 58% (29/50) of cases, respectively. In the study by Galiano et al., 19 the lesions found were within reach of the standard endoscope in 24.7% of the patients with suspected SBB(24/97): esophagus: 1, stomach: 10, duodenum: 8 and colon: 5. In the case of the study by García del Risco et al., 88 14% of the patients presented lesions within reach of the standard endoscope (7/50), distributed as follows: one in the esophagus, two in the stomach, one in the duodenum and three in the right colon.
Performance of a cost-effectiveness analysis with these data shows that if a new EGD and total colonoscopy were carried out for all patients in the first study, COP 76,436,000 would have been spent on endoscopies (97 X COP 788,000) which which would have avoided the use of 24 VCEs with an expenditure per VCE of COP 438,000,000 (73 X COP 6,000,000) for a total of COP 514,436,000. In contrast, initial VCE alone for all patients would have cost COP 582,000,000 (97 X COP 6,000,000), representing an additional expense of COP 696,536 per patient. For the second study, performance of a new EGD and total colonoscopy followed by VCE in cases of not finding the cause of the suspected SBB, would have cost COP 297,400,000 (50 X COP 788,000 + 43 X COP 6,000,000) while initial VCE alone would have cost COP 300,000,000 (50 X COP 6,000,000). This represents an additional cost of COP 52,000 per patient for initial VCE alone. However, it should be emphasized that these studies were not designed to analyze cost-effectiveness, but there are no other studies that allow analysis of this for Colombia.
If international findings are extrapolated to local costs, better cost-effectiveness is also found with VCE as the initial strategy after negative initial endoscopic examinations. However, if the calculations take into account the findings of the two published Colombian series, this strategy may be less cost-effective. The cost of VCE in other countries is less than twice that of repeated EGD and colonoscopy which implies that VCE is the most cost-effective initial study for patients with suspected SBB. This has been manifested in the three international studies to date that have included economic analyses. 18,42,43 In contrast, in Colombia VCE is around 7.6 times more expensive than a second upper and lower endoscopy resulting in a cost ratio that is much higher than the one found internationally. Given this high ratio, the cost-effectiveness of VCE cannot be assured when a second EGD and total colonoscopy are avoided. Therefore, we consider that specific comparative studies of VCE’s cost-effectiveness be performed here in Colombia.
Conclusions
Video capsule endoscopy is an excellent method for evaluating the small intestine which is recognized as such by the main scientific societies of the world. Its diagnostic yield for suspected SBB is excellent, and is considered to be the gold standard by some. Similarly, it is evident that its performance is better than that of a second upper and lower endoscopy in these patients. It can even detect causes that these initial endoscopic overlook even though they are within their reach. In the light of the world scientific literature published so far, and given its yields, safety and non-invasive nature compared to other methods, VCE seems to be the best option for the study of suspected SBB after a first EGD and colonoscopy. Similarly, the greater cost-effectiveness of VCE has been clearly demonstrated in the international arena. Nevertheless, in our setting VCE is 7.6 times more expensive than a second EGD and total colonoscopy, so there are doubts about which of the two strategies is more cost-effective in our country. This uncertainty will only change if local VCE prices become more competitive or if properly designed local prospective studies are carried out. One recommendation that has emerged from international and Colombian findings from studies of VCE is that EGDs and total colonoscopys performed in patients with overt or occult bleeding need to be performed to the highest quality standard to avoid overlooking lesions that are within the scope of these endoscopic procedures.
Referencias
1. Szold A, Katz LB, Lewis BS. Surgical approach to occult gastrointestinal bleeding. Am J Surg. 1992;163(1):90-2; discussion 2-3. https://doi.org/10.1016/0002-9610(92)90258-S [ Links ]
2. Longstreth GF. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1997;92(3):419-24. [ Links ]
3. Triester SL, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2005;100(11):2407-18. https://doi.org/10.1111/j.1572-0241.2005.00274.x [ Links ]
4. Chong J, Tagle M, Barkin JS, Reiner DK. Small bowel push-type fiberoptic enteroscopy for patients with occult gastrointestinal bleeding or suspected small bowel pathology. Am J Gastroenterol. 1994;89(12):2143-6. [ Links ]
5. Tee HP, Kaffes AJ. Non-small-bowel lesions encountered during double-balloon enteroscopy performed for obscure gastrointestinal bleeding. World J Gastroenterol. 2010;16(15):1885-9. https://doi.org/10.3748/wjg.v16.i15.1885 [ Links ]
6. ASGE Technology Committee, Wang A, Banerjee S, Barth BA, Bhat YM, Chauhan S, Gottlieb KT, Konda V, Maple JT, Murad F, Pfau PR, Pleskow DK, Siddiqui UD, Tokar JL, Rodriguez SA. Wireless capsule endoscopy. Gastrointest Endosc. 2013;78(6):805-15. https://doi.org/10.1016/j.gie.2013.06.026 [ Links ]
7. Ell C, Remke S, May A, Helou L, Henrich R, Mayer G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy. 2002;34(9):685-9. https://doi.org/10.1055/s-2002-33446 [ Links ]
8. American Gastroenterological Association. American Gastroenterological Association medical position statement: evaluation and management of occult and obscure gastrointestinal bleeding. Gastroenterology. 2000;118(1):197-201. https://doi.org/10.1016/S0016-5085(00)70429-X [ Links ]
9. Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015;110(9):1265-87; quiz 88. https://doi.org/10.1038/ajg.2015.246 [ Links ]
10. Liu K, Kaffes AJ. Review article: the diagnosis and investigation of obscure gastrointestinal bleeding. Aliment Pharmacol Ther. 2011;34(4):416-23. https://doi.org/10.1111/j.1365-2036.2011.04744.x [ Links ]
11. Hale MF, Sidhu R, McAlindon ME. Capsule endoscopy: current practice and future directions. World J Gastroenterol. 2014;20(24):7752-9. https://doi.org/10.3748/wjg.v20.i24.7752 [ Links ]
12. Gay G, Delvaux M, Rey JF. The role of video capsule endoscopy in the diagnosis of digestive diseases: a review of current possibilities. Endoscopy. 2004;36(10):913-20. https://doi.org/10.1055/s-2004-825868 [ Links ]
13. Nakamura T, Terano A. Capsule endoscopy: past, present, and future. J Gastroenterol. 2008;43(2):93-9. https://doi.org/10.1007/s00535-007-2153-6 [ Links ]
14. Zaman A, Katon RM. Push enteroscopy for obscure gastrointestinal bleeding yields a high incidence of proximal lesions within reach of a standard endoscope. Gastrointest Endosc. 1998;47(5):372-6. https://doi.org/10.1016/S0016-5107(98)70221-4 [ Links ]
15. Descamps C, Schmit A, Van Gossum A. “Missed” upper gastrointestinal tract lesions may explain “occult” bleeding. Endoscopy. 1999;31(6):452-5. https://doi.org/10.1055/s-1999-151 [ Links ]
16. Tang SJ, Christodoulou D, Zanati S, Dubcenco E, Petroniene R, Cirocco M, Kandel G, Haber GB, Kortan P, Marcon NE. Wireless capsule endoscopy for obscure gastrointestinal bleeding: a single-centre, one-year experience. Can J Gastroenterol. 2004;18(9):559-65. https://doi.org/10.1155/2004/205685 [ Links ]
17. Sandoval Riveros C, Lúquez Mindiola A, Marulanda Fernandez H, Otero Regino W. Sangrado del intestino delgado: enfoque y tratamiento Rev Colomb Gastroenterol. 2017;32(3):245-57. https://doi.org/10.22516/25007440.156 [ Links ]
18. Gilbert D, O’Malley S, Selby W. Are repeat upper gastrointestinal endoscopy and colonoscopy necessary within six months of capsule endoscopy in patients with obscure gastrointestinal bleeding? J Gastroenterol Hepatol. 2008;23(12):1806-9. https://doi.org/10.1111/j.1440-1746.2008.05643.x [ Links ]
19. Galiano de Sánchez MT, Sánchez Arciniegas F, Pineda Ovalle LF. Experiencia clínica del uso de la videocápsula endoscópica en el diagnóstico de patología del intestino delgado. Rev Col Gastroenterol. 2009;24(1):17-25. [ Links ]
20. Swain P. Wireless capsule endoscopy. Gut. 2003;52 Suppl 4:iv48-50. https://doi.org/10.1136/gut.52.suppl_4.iv48 [ Links ]
21. Swain CP, Gong F, Mills TN. Wireless transmission of a color television moving image from the stomach using a miniature CCD camera, light source and microwave transmitter [abstract]. Gut. 1996;39:A26. https://doi.org/10.1016/S0016-5107(97)80063-6 [ Links ]
22. Gerber J, Bergwerk A, Fleischer D. A capsule endoscopy guide for the practicing clinician: technology and troubleshooting. Gastrointest Endosc. 2007;66(6):1188-95. https://doi.org/10.1016/j.gie.2007.06.003 [ Links ]
23. Mustafa BF, Samaan M, Langmead L, Khasraw M. Small bowel video capsule endoscopy: an overview. Expert Rev Gastroenterol Hepatol. 2013;7(4):323-9. https://doi.org/10.1586/egh.13.20 [ Links ]
24. Hartmann D, Eickhoff A, Damian U, Riemann JF. Diagnosis of small-bowel pathology using paired capsule endoscopy with two different devices: a randomized study. Endoscopy. 2007;39(12):1041-5. https://doi.org/10.1055/s-2007-966943 [ Links ]
25. Schostek S, Schurr MO. European research on wireless endoscopy--the VECTOR project. Stud Health Technol Inform. 2013;189:193-9. [ Links ]
26. Bouchard S, Ibrahim M, Van Gossum A. Video capsule endoscopy: perspectives of a revolutionary technique. World J Gastroenterol. 2014;20(46):17330-44. https://doi.org/10.3748/wjg.v20.i46.17330 [ Links ]
27. Kalla R, McAlindon ME, Drew K, Sidhu R. Clinical utility of capsule endoscopy in patients with Crohn’s disease and inflammatory bowel disease unclassified. Eur J Gastroenterol Hepatol. 2013;25(6):706-13. https://doi.org/10.1097/MEG.0b013e32835ddb85 [ Links ]
28. Rokkas T, Niv Y. The role of video capsule endoscopy in the diagnosis of celiac disease: a meta-analysis. Eur J Gastroenterol Hepatol. 2012;24(3):303-8. https://doi.org/10.1097/MEG.0b013e32834fa914 [ Links ]
29. Cobrin GM, Pittman RH, Lewis BS. Increased diagnostic yield of small bowel tumors with capsule endoscopy. Cancer. 2006;107(1):22-7. https://doi.org/10.1002/cncr.21975 [ Links ]
30. Endo H, Hosono K, Inamori M, Kato S, Nozaki Y, Yoneda K, Akiyama T, Fujita K, Takahashi H, Yoneda M, Abe Y, Kirikoshi H, Kobayashi N, Kubota K, Saito S, Matsuhashi N, Nakajima A. Incidence of small bowel injury induced by low-dose aspirin: a crossover study using capsule endoscopy in healthy volunteers. Digestion. 2009;79(1):44-51. https://doi.org/10.1159/000204465 [ Links ]
31. Riccioni ME, Urgesi R, Spada C, Cianci R, Pelecca G, Bizzotto A, Costamagna G. Unexplained iron deficiency anaemia: Is it worthwhile to perform capsule endoscopy? Dig Liver Dis. 2010;42(8):560-6. https://doi.org/10.1016/j.dld.2010.01.023 [ Links ]
32. Koulaouzidis A, Rondonotti E, Giannakou A, Plevris JN. Diagnostic yield of small-bowel capsule endoscopy in patients with iron-deficiency anemia: a systematic review. Gastrointest Endosc. 2012;76(5):983-92. https://doi.org/10.1016/j.gie.2012.07.035 [ Links ]
33. Mishkin DS, Chuttani R, Croffie J, Disario J, Liu J, Shah R, Somogyi L, Tierney W, Song LM, Petersen BT; Technology Assessment Committee, American Society for Gastrointestinal Endoscopy. ASGE Technology Status Evaluation Report: wireless capsule endoscopy. Gastrointest Endosc. 2006;63(4):539-45. https://doi.org/10.1016/j.gie.2006.01.014 [ Links ]
34. Van Gossum A, Devière J. Colon capsule endoscopy: a new tool for colon examination? Discov Med. 2010;9(44):46-50. [ Links ]
35. Sánchez-Yagüe A, Caunedo-Alvarez A, García-Montes JM, Romero-Vázquez J, Pellicer-Bautista FJ, Herrerías-Gutiérrez JM. Esophageal capsule endoscopy in patients refusing conventional endoscopy for the study of suspected esophageal pathology. Eur J Gastroenterol Hepatol. 2006;18(9):977-83. https://doi.org/10.1097/01.meg.0000230094.21911.f8 [ Links ]
36. Chavalitdhamrong D, Chen GC, Roth BE, Goltzer O, Sul J, Jutabha R. Esophageal capsule endoscopy for evaluation of patients with chronic gastroesophageal reflux symptoms: findings and its image quality. Dis Esophagus. 2011;24(5):295-8. https://doi.org/10.1111/j.1442-2050.2010.01136.x [ Links ]
37. Romero-Vázquez J, Jiménez-García VA, Herrerías-Gutiérrez JM. Esophageal capsule endoscopy and Barrett’s esophagus: where are we in 2013? Rev Gastroenterol Mex. 2013;78(2):55-6. https://doi.org/10.1016/j.rgmx.2013.02.002 [ Links ]
38. Ishiguro H, Saito S, Imazu H, Aihara H, Kato T, Tajiri H. Esophageal Capsule Endoscopy for Screening Esophageal Varices among Japanese Patients with Liver Cirrhosis. Gastroenterol Res Pract. 2012;2012:946169. https://doi.org/10.1155/2012/946169 [ Links ]
39. Lu Y, Gao R, Liao Z, Hu LH, Li ZS. Meta-analysis of capsule endoscopy in patients diagnosed or suspected with esophageal varices. World J Gastroenterol. 2009;15(10):1254-8. https://doi.org/10.3748/wjg.15.1254 [ Links ]
40. Romero-Vázquez J, Argüelles-Arias F, García-Montes JM, Caunedo-Álvarez Á, Pellicer-Bautista FJ, Herrerías-Gutiérrez JM. Capsule endoscopy in patients refusing conventional endoscopy. World J Gastroenterol. 2014;20(23):7424-33. https://doi.org/10.3748/wjg.v20.i23.7424 [ Links ]
41. Yamashita K, Okumura H, Oka Y, Urakami A, Shiotani A, Nakashima H, Matsumoto H, Hirai T, Nakamura M. Minimally invasive surgery using intraoperative real-time capsule endoscopy for small bowel lesions. Surg Endosc. 2013;27(7):2337-41. https://doi.org/10.1007/s00464-012-2777-3 [ Links ]
42. Vlachogiannakos J, Papaxoinis K, Viazis N, Kegioglou A, Binas I, Karamanolis D, Ladas S. Bleeding lesions within reach of conventional endoscopy in capsule endoscopy examinations for obscure gastrointestinal bleeding: is repeating endoscopy economically feasible? Dig Dis Sci. 2011;56(6):1763-8. https://doi.org/10.1007/s10620-011-1592-3 [ Links ]
43. Marmo R, Rotondano G, Rondonotti E, de Franchis R, D’Incà R, Vettorato MG, Costamagna G, Riccioni ME, Spada C, D’Angella R, Milazzo G, Faraone A, Rizzetto M, Barbon V, Occhipinti P, Saettone S, Iaquinto G, Rossini FP; Club Italiano Capsula Endoscopica - CICE. Capsule enteroscopy vs. other diagnostic procedures in diagnosing obscure gastrointestinal bleeding: a cost-effectiveness study. Eur J Gastroenterol Hepatol. 2007;19(7):535-42. https://doi.org/10.1097/MEG.0b013e32812144dd [ Links ]
44. Liao Z, Gao R, Xu C, Li ZS. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc. 2010;71(2):280-6. https://doi.org/10.1016/j.gie.2009.09.031 [ Links ]
45. Pennazio M, Santucci R, Rondonotti E, Abbiati C, Beccari G, Rossini FP, De Franchis R. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: report of 100 consecutive cases. Gastroenterology . 2004;126(3):643-53. https://doi.org/10.1053/j.gastro.2003.11.057 [ Links ]
46. Chak A, Cooper GS, Canto MI, Pollack BJ, Sivak MV. Enteroscopy for the initial evaluation of iron deficiency. Gastrointest Endosc. 1998;47(2):144-8. https://doi.org/10.1016/S0016-5107(98)70347-5 [ Links ]
47. Landi B, Tkoub M, Gaudric M, Guimbaud R, Cervoni JP, Chaussade S, Couturier D, Barbier JP, Cellier C. Diagnostic yield of push-type enteroscopy in relation to indication. Gut. 1998;42(3):421-5. https://doi.org/10.1136/gut.42.3.421 [ Links ]
48. Fry LC, Bellutti M, Neumann H, Malfertheiner P, Mönkemüller K. Incidence of bleeding lesions within reach of conventional upper and lower endoscopes in patients undergoing double-balloon enteroscopy for obscure gastrointestinal bleeding. Aliment Pharmacol Ther . 2009;29(3):342-9. https://doi.org/10.1111/j.1365-2036.2008.03888.x [ Links ]
49. Viazis N, Papaxoinis K, Theodoropoulos I, Sgouros S, Vlachogiannakos J, Pipis P, Markoglou C, Avgerinos A. Impact of capsule endoscopy in obscure small-bowel bleeding: defining strict diagnostic criteria for a favorable outcome. Gastrointest Endosc. 2005;62(5):717-22. https://doi.org/10.1016/j.gie.2005.06.049 [ Links ]
50. Estévez E, González-Conde B, Vázquez-Iglesias JL, de Los Angeles Vázquez-Millán M, Pértega S, Alonso PA, Clofent J, Santos E, Ulla JL, Sánchez E. Diagnostic yield and clinical outcomes after capsule endoscopy in 100 consecutive patients with obscure gastrointestinal bleeding. Eur J Gastroenterol Hepatol. 2006;18(8):881-8. https://doi.org/10.1097/00042737-200608000-00014 [ Links ]
51. Kitiyakara T, Selby W. Non-small-bowel lesions detected by capsule endoscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005;62(2):234-8. https://doi.org/10.1016/S0016-5107(05)00292-0 [ Links ]
52. Chong AK, Taylor AC, Miller AM, Desmond PV. Initial experience with capsule endoscopy at a major referral hospital. Med J Aust. 2003;178(11):537-40. https://doi.org/10.5694/j.1326-5377.2003.tb05354.x [ Links ]
53. Sturniolo GC, Di Leo V, Vettorato MG, De Boni M, Lamboglia F, De Bona M, Bellumat A, Martines D, D›Inca R. Small bowel exploration by wireless capsule endoscopy: results from 314 procedures. Am J Med. 2006;119(4):341-7. https://doi.org/10.1016/j.amjmed.2005.08.029 [ Links ]
54. Carey EJ, Leighton JA, Heigh RI, Shiff AD, Sharma VK, Post JK, Fleischer DE. A single-center experience of 260 consecutive patients undergoing capsule endoscopy for obscure gastrointestinal bleeding. Am J Gastroenterol. 2007;102(1):89-95. https://doi.org/10.1111/j.1572-0241.2006.00941.x [ Links ]
55. Hoedemaker RA, Westerhof J, Weersma RK, Koornstra JJ. Non-small-bowel abnormalities identified during small bowel capsule endoscopy. World J Gastroenterol. 2014;20(14):4025-9. https://doi.org/10.3748/wjg.v20.i14.4025 [ Links ]
56. ASGE Standards of Practice Committee, Fisher L, Lee Krinsky M, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Cash BD, Decker GA, Fanelli RD, Friis C, Fukami N, Harrison ME, Ikenberry SO, Jain R, Jue T, Khan K, Maple JT, Strohmeyer L, Sharaf R, Dominitz JA. The role of endoscopy in the management of obscure GI bleeding. Gastrointest Endosc. 2010;72(3):471-9. https://doi.org/10.1016/j.gie.2010.04.032 [ Links ]
57. Rey JF, Ladas S, Alhassani A, Kuznetsov K, Committee EG. European Society of Gastrointestinal Endoscopy (ESGE). Video capsule endoscopy: update to guidelines (May 2006). Endoscopy. 2006;38(10):1047-53. https://doi.org/10.1055/s-2006-944874 [ Links ]
58. Melmed GY, Lo SK. Capsule endoscopy: practical applications. Clin Gastroenterol Hepatol. 2005;3(5):411-22. https://doi.org/10.1016/S1542-3565(05)00019-4 [ Links ]
59. Marmo R, Rotondano G, Piscopo R, Bianco MA, Cipolletta L. Meta-analysis: capsule enteroscopy vs. conventional modalities in diagnosis of small bowel diseases. Aliment Pharmacol Ther . 2005;22(7):595-604. https://doi.org/10.1111/j.1365-2036.2005.02625.x [ Links ]
60. de Leusse A, Vahedi K, Edery J, Tiah D, Fery-Lemonnier E, Cellier C, Bouhnik Y, Jian R. Capsule endoscopy or push enteroscopy for first-line exploration of obscure gastrointestinal bleeding? Gastroenterology . 2007;132(3):855-62; quiz 1164-5. https://doi.org/10.1053/j.gastro.2006.12.002 [ Links ]
61. Saurin JC, Delvaux M, Vahedi K, Gaudin JL, Villarejo J, Florent C, Gay G, Ponchon T. Clinical impact of capsule endoscopy compared to push enteroscopy: 1-year follow-up study. Endoscopy. 2005;37(4):318-23. https://doi.org/10.1055/s-2005-861114 [ Links ]
62. Matsumoto T, Esaki M, Moriyama T, Nakamura S, Iida M. Comparison of capsule endoscopy and enteroscopy with the double-balloon method in patients with obscure bleeding and polyposis. Endoscopy. 2005;37(9):827-32. https://doi.org/10.1055/s-2005-870207 [ Links ]
63. Chen X, Ran ZH, Tong JL. A meta-analysis of the yield of capsule endoscopy compared to double-balloon enteroscopy in patients with small bowel diseases. World J Gastroenterol. 2007;13(32):4372-8. https://doi.org/10.3748/wjg.v13.i32.4372 [ Links ]
64. Nakamura M, Niwa Y, Ohmiya N, Miyahara R, Ohashi A, Itoh A, Hirooka Y, Goto H. Preliminary comparison of capsule endoscopy and double-balloon enteroscopy in patients with suspected small-bowel bleeding. Endoscopy. 2006;38(1):59-66. https://doi.org/10.1055/s-2005-870446 [ Links ]
65. Arakawa D, Ohmiya N, Nakamura M, Honda W, Shirai O, Itoh A, Hirooka Y, Niwa Y, Maeda O, Ando T, Goto H. Outcome after enteroscopy for patients with obscure GI bleeding: diagnostic comparison between double-balloon endoscopy and videocapsule endoscopy. Gastrointest Endosc. 2009;69(4):866-74. https://doi.org/10.1016/j.gie.2008.06.008 [ Links ]
66. Hadithi M, Heine GD, Jacobs MA, van Bodegraven AA, V Bodegraven AA, Mulder CJ. A prospective study comparing video capsule endoscopy with double-balloon enteroscopy in patients with obscure gastrointestinal bleeding. Am J Gastroenterol . 2006;101(1):52-7. https://doi.org/10.1111/j.1572-0241.2005.00346.x [ Links ]
67. Pasha SF, Leighton JA, Das A, Harrison ME, Decker GA, Fleischer DE, Sharma VK. Double-balloon enteroscopy and capsule endoscopy have comparable diagnostic yield in small-bowel disease: a meta-analysis. Clin Gastroenterol Hepatol . 2008;6(6):671-6. https://doi.org/10.1016/j.cgh.2008.01.005 [ Links ]
68. Douard R, Wind P, Panis Y, Marteau P, Bouhnik Y, Cellier C, Cugnenc P, Valleur P. Intraoperative enteroscopy for diagnosis and management of unexplained gastrointestinal bleeding. Am J Surg . 2000;180(3):181-4. https://doi.org/10.1016/S0002-9610(00)00447-5 [ Links ]
69. Hartmann D, Schmidt H, Bolz G, Schilling D, Kinzel F, Eickhoff A, Huschner W, Möller K, Jakobs R, Reitzig P, Weickert U, Gellert K, Schultz H, Guenther K, Hollerbuhl H, Schoenleben K, Schulz HJ, Riemann JF. A prospective two-center study comparing wireless capsule endoscopy with intraoperative enteroscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005;61(7):826-32. https://doi.org/10.1016/S0016-5107(05)00372-X [ Links ]
70. Voderholzer WA, Ortner M, Rogalla P, Beinhölzl J, Lochs H. Diagnostic yield of wireless capsule enteroscopy in comparison with computed tomography enteroclysis. Endoscopy. 2003;35(12):1009-14. https://doi.org/10.1055/s-2003-44583 [ Links ]
71. Gölder SK, Schreyer AG, Endlicher E, Feuerbach S, Schölmerich J, Kullmann F, Seitz J, Rogler G, Herfarth H. Comparison of capsule endoscopy and magnetic resonance (MR) enteroclysis in suspected small bowel disease. Int J Colorectal Dis. 2006;21(2):97-104. https://doi.org/10.1007/s00384-005-0755-0 [ Links ]
72. Malik A, Lukaszewski K, Caroline D, Parkman H, DeSipio J, Banson F, Bazir K, Reddy L, Srinivasan R, Fisher R, Miller L. A retrospective review of enteroclysis in patients with obscure gastrointestinal bleeding and chronic abdominal pain of undetermined etiology. Dig Dis Sci . 2005;50(4):649-55. https://doi.org/10.1007/s10620-005-2551-7 [ Links ]
73. Kepczyk T, Kadakia SC. Prospective evaluation of gastrointestinal tract in patients with iron-deficiency anemia. Dig Dis Sci . 1995;40(6):1283-9. https://doi.org/10.1007/BF02065539 [ Links ]
74. Moch A, Herlinger H, Kochman ML, Levine MS, Rubesin SE, Laufer I. Enteroclysis in the evaluation of obscure gastrointestinal bleeding. AJR Am J Roentgenol. 1994;163(6):1381-4. https://doi.org/10.2214/ajr.163.6.7992733 [ Links ]
75. Rex DK, Lappas JC, Maglinte DD, Malczewski MC, Kopecky KA, Cockerill EM. Enteroclysis in the evaluation of suspected small intestinal bleeding. Gastroenterology . 1989;97(1):58-60. https://doi.org/10.1016/0016-5085(89)91415-7 [ Links ]
76. Mylonaki M, Fritscher-Ravens A, Swain P. Wireless capsule endoscopy: a comparison with push enteroscopy in patients with gastroscopy and colonoscopy negative gastrointestinal bleeding. Gut. 2003;52(8):1122-6. https://doi.org/10.1136/gut.52.8.1122 [ Links ]
77. Leung WK, Ho SS, Suen BY, Lai LH, Yu S, Ng EK, Ng SM, Chiu PW, Sung JY, Chan FK, Lau JY. Capsule endoscopy or angiography in patients with acute overt obscure gastrointestinal bleeding: a prospective randomized study with long-term follow-up. Am J Gastroenterol . 2012;107(9):1370-6. https://doi.org/10.1038/ajg.2012.212 [ Links ]
78. Saperas E, Dot J, Videla S, Alvarez-Castells A, Perez-Lafuente M, Armengol JR, Malagelada JR. Capsule endoscopy versus computed tomographic or standard angiography for the diagnosis of obscure gastrointestinal bleeding. Am J Gastroenterol . 2007;102(4):731-7. https://doi.org/10.1111/j.1572-0241.2007.01058.x [ Links ]
79. Rana SS, Bhasin DK, Nagi B, Zargar SA, Malhi NS, Sinha SK, Singh K. Comparative evaluation of barium meal follow-through and barium enteroclysis before capsule endoscopy in obscure gastrointestinal bleeding. Hepatogastroenterology. 2012;59(114):418-21. https://doi.org/10.5754/hge10312 [ Links ]
80. Sachdev MS, Leighton JA, Fleischer DE, Heigh RI, Hara AK, Post JA, Erickson PJ, Sharma VK. A prospective study of the utility of abdominal radiographs after capsule endoscopy for the diagnosis of capsule retention. Gastrointest Endosc. 2007;66(5):894-900. https://doi.org/10.1016/j.gie.2007.06.066 [ Links ]
81. Enns RA, Hookey L, Armstrong D, Bernstein CN, Heitman SJ, Teshima C, Leontiadis G, Tse F, Sadowski D. Clinical Practice Guidelines for the Use of Video Capsule Endoscopy. Gastroenterology . 2017;152(3):497-514. https://doi.org/10.1053/j.gastro.2016.12.032 [ Links ]
82. Saurin JC, Delvaux M, Gaudin JL, Fassler I, Villarejo J, Vahedi K, Bitoun A, Canard JM, Souquet JC, Ponchon T, Florent C, Gay C. Diagnostic value of endoscopic capsule in patients with obscure digestive bleeding: blinded comparison with video push-enteroscopy. Endoscopy. 2003;35(7):576-84. https://doi.org/10.1055/s-2003-40244 [ Links ]
83. Mata A, Bordas JM, Feu F, Ginés A, Pellisé M, Fernández-Esparrach G, Balaguer F, Piqué JM, Llach J. Wireless capsule endoscopy in patients with obscure gastrointestinal bleeding: a comparative study with push enteroscopy. Aliment Pharmacol Ther . 2004;20(2):189-94. https://doi.org/10.1111/j.1365-2036.2004.02067.x [ Links ]
84. Costamagna G, Shah SK, Riccioni ME, Foschia F, Mutignani M, Perri V, Vecchioli A, Brizi MG, Picciocchi A, Marano P. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology . 2002;123(4):999-1005. https://doi.org/10.1053/gast.2002.35988 [ Links ]
85. Kameda N, Higuchi K, Shiba M, Machida H, Okazaki H, Yamagami H, Tanigawa T, Watanabe K, Watanabe T, Tominaga K, Fujiwara Y, Oshitani N, Arakawa T. A prospective, single-blind trial comparing wireless capsule endoscopy and double-balloon enteroscopy in patients with obscure gastrointestinal bleeding. J Gastroenterol . 2008;43(6):434-40. https://doi.org/10.1007/s00535-008-2182-9 [ Links ]
86. Li X, Dai J, Lu H, Gao Y, Chen H, Ge Z. A prospective study on evaluating the diagnostic yield of video capsule endoscopy followed by directed double-balloon enteroscopy in patients with obscure gastrointestinal bleeding. Dig Dis Sci . 2010;55(6):1704-10. https://doi.org/10.1007/s10620-009-0911-4 [ Links ]
87. Heine GD, Hadithi M, Groenen MJ, Kuipers EJ, Jacobs MA, Mulder CJ. Double-balloon enteroscopy: indications, diagnostic yield, and complications in a series of 275 patients with suspected small-bowel disease. Endoscopy. 2006;38(1):42-8. https://doi.org/10.1055/s-2005-921188 [ Links ]
88. García del Risco F, Arrieta López E. Rendimiento diagnóstico y hallazgos con la cápsula endoscópica en pacientes con sangrado digestivo de origen oscuro en la Clínica Universitaria San Juan de Dios en Cartagena, Colombia. Rev Col Gastroenterol . 2014;29(2):101-11. [ Links ]
Received: May 18, 2018; Accepted: August 13, 2018











 texto em
texto em 


