Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.2 Bogotá Apr./June 2020
https://doi.org/10.22516/25007440.402
Case report
Rapunzel Syndrome: Myth or Reality
1 Especialista en Gastroenterología, Universidad Nacional de Colombia. Especialista en Medicina Interna, Pontificia Universidad Javeriana. Hospital Occidente de Kennedy, Hospital Universitario Nacional; Bogotá, Colombia
2 Profesor asociado de Gastroenterología, Universidad Nacional de Colombia. Hospital Universitario Nacional, Hospital Occidente de Kennedy, Unidad de Gastroenterología y Ecoendoscopia-UGEC; Bogotá, Colombia
3 Fellow de Gastroenterología, Universidad Nacional de Colombia. Especialista en Medicina Interna, Universidad Nacional de Colombia, Hospital Universitario Nacional; Bogotá, Colombia
A 35-year-old patient was admitted to the emergency department of a third-level hospital following six months of early satiety and weight loss. Upon physical admission, the patient had signs of malnutrition. Upper digestive tract endoscopy found a trichobezoar that occupied the entire gastric chamber and extended into the third portion of the duodenum. This diagnosis was confirmed by an abdominal CT scan. Surgery confirmed the diagnosis of Rapunzel Syndrome. Following surgery the patient’s evolution was good and symptoms resolved. Nutritional and psychological interventions were initiated to manage malnutrition and an underlying psychiatric disorder.
Keywords: Endoscopy; stomach; bezoar; trichobezoar; Rapunzel; surgery; anxiety
Se presenta el caso de una paciente de 35 años, quien ingresa al servicio de urgencias de un hospital de tercer nivel, por causa de un cuadro de 6 meses de saciedad precoz, pérdida de peso y, en el momento del examen físico de ingreso, se observan signos de desnutrición. En consecuencia, se realiza una endoscopia de las vías digestivas altas en las que se descubre un tricobezoar que ocupa toda la cámara gástrica y se extiende más allá de la tercera porción del duodeno. Mediante una tomografía axial computarizada (TAC) de abdomen, se confirma la presencia de una lesión que ocupa la cámara gástrica y el duodeno, por lo que la paciente es conducida a cirugía. Allí se encuentra el tricobezoar que confirma el diagnóstico de síndrome de Rapunzel. Luego de la cirugía, la paciente presenta una adecuada evolución posoperatoria, con resolución de los síntomas de ingreso. Asimismo, se inicia una intervención por nutrición y psicología, a fin de manejar la desnutrición y el trastorno psiquiátrico de base.
Palabras claves: Endoscopia; estómago; bezoar; tricobezoar; Rapunzel; cirugía; ansiedad
Introduction
Bezoars are defined as the accumulation of organic substances within the gastrointestinal tract. Only 30% Of patients with trichotillomania develop trichophagia, and only 1% require surgical treatment. Initially described by Vaughan and colleagues 1, Rapunzel syndrome is a rare form of trichobezoar that extends beyond the stomach. Fewer than 100 cases have been reported in the literature.
Although there are reports of trichobezoars that extend from the stomach to the jejunum, ileum, and even the colon, 2-5 authors disagree about which trichobezoars should be defined as Rapunzel syndrome. For some, the true Rapunzel syndrome is one in which the trichobezoar extends to the ileocecal valve, while others consider that any trichobezoar that reaches the jejunum, whether or not it reaches the ileocecal valve, should be included. Other authors define Rapunzel syndrome as any trichobezoar that occurs together with an intestinal obstruction. 6
Ninety percent of trichobezoars occur in women, and 80% occur in people under 30 years of age. In fact, they are rare in the adult population. 7-9 Symptoms depend on the trichobezoar’s size, duration of evolution and location. 10 In 70% of cases, patients present abdominal pain, early satiety, hyporexia, nausea, and vomiting (64%). Hematemesis (61%), weight loss (38%), diarrhea or constipation (32%), and halitosis can also occur.
Symptoms associated with larger bezoars include a sensation of mass, malabsorption, obstructive jaundice, traumatic gastric or duodenal ulcers, obstruction and perforations. 3,10 Below, we present the clinical case of a patient with a typical picture of Rapunzel syndrome and discuss diagnosis and treatment of this rare pathology.
Case presentation
A 35-year-old woman came to the hospital due to 6 months of early satiety, loss of 10 kg of weight, and oral intolerance for the final three weeks prior to admission. The patient had a history of depression which had been irregularly treated due to her poor adherence to therapy.
At the time of physical examination, the patient had sarcopenia and a mucocutaneous pallor and was underweight. Laboratory tests performed upon admission showed hypoalbuminemia, hypochromic microcytic anemia, and hypokalemia with hypomagnesemia. These findings were compatible with protein-calorie malnutrition.
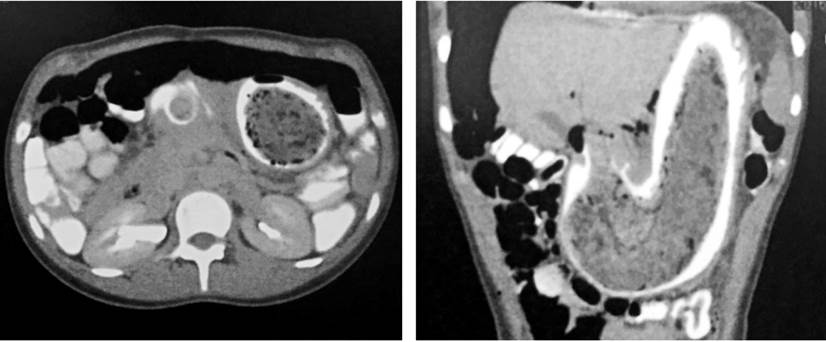
A double contrast abdominal CT scan showed that the gastric chamber was distended and occupied by a lesion of variable densities which partially obstructed passage of the contrast medium. After evaluating the radiographic findings, we decided to perform esophagogastroduodenoscopy. It found a compact conglomerate composed of a foreign body (bezoar) that extended from the cardia to beyond the fourth duodenal portion and which caused distal obstruction (Figure 1).
Endoscopy had discovered a bezoar-type intragastric foreign body that occupied the gastric chamber and the duodenum in its entirety, thereby constituting Rapunzel syndrome (Figure 2).

Figure 2 Endoscopy of the upper digestive tract. There is abundant hair coming from the stomach, which prevented passage of the endoscopy equipment.
In view of the obstruction and because it was not possible to extract the bezoar endoscopically, we decided to refer the patient to surgery. A laparotomy was performed to explore the gastric chamber. A trichobezoar that extended from the stomach to the jejunum was found and extracted without complications (Figure 3).
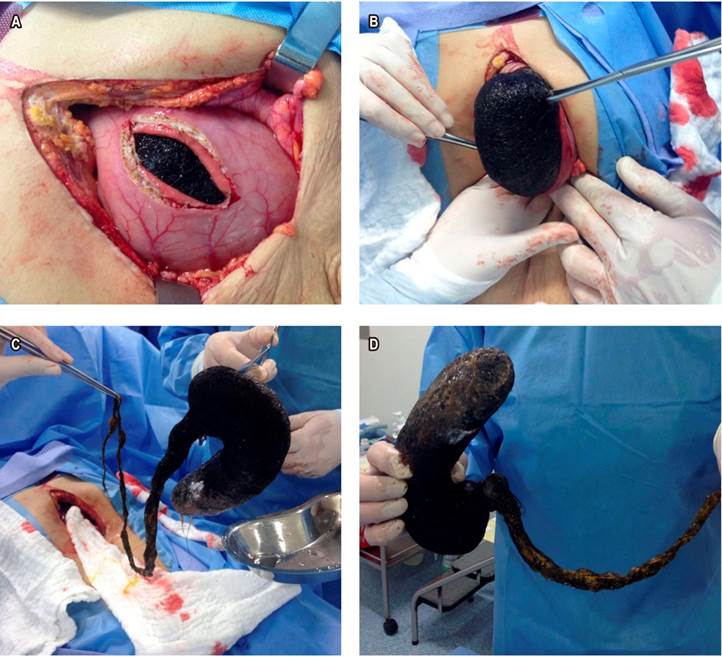
Figure 3 Surgical removal of the trichobezoar (A, B and C). Surgical piece of the trichobezoar, molded to the shape of the stomach and small intestine (D).
After surgery, the patient’s symptoms significantly improved, she showed adequate tolerance to oral feeling. route, and her abdominal pain resolved. In parallel, the Psychiatry, Psychology, Nutrition and Social Work departments focused on management of the patient’s anxiety disorder including providing her with medication and psychological therapy.
Meanwhile, the Nutrition area began nutritional supplementation. The patient was assessed during a medical control and was found to have gained weight. Other nutritional indices had improved as well. Based on these interventions, the patient reported fewer symptoms of anxiety and said that she had stopped compulsively eating her hair.
Discussion
This case clearly meets the criteria defined for Rapunzel syndrome since the patient had a trichobezoar that extended from the stomach to beyond the jejunum which produced intestinal obstruction.
In general, information provided by patients is of little use for the diagnosis of trichobezoar since patients tend to hide details of trichophagia. However, the presence of hair in the stool or vomit can indicate this diagnosis.
Contrast CT scans and esophagogastroduodenoscopy are the best diagnostic tools for Rapunzel syndrome. A CT scan usually shows a well-circumscribed gastric lesion composed of concentric spirals of different densities with entangled air bubbles. Oral contrast fills most peripheral interstices of the lesion and produces a thin band of contrast that circumscribes the lesion. 11
Upper gastrointestinal endoscopy can generally provide immediate diagnosis of bezoars and can be used for to administer a proteolytic such as papain or acetylcysteine to remove organic material. However, the success rate of these methods is less than 50%, so endoscopic, laparoscopic or open surgery is preferred. 12-16
When endoscopic surgery is required, general anesthesia should be administered with orotracheal intubation in order to reduce the risk of aspiration. 15 However, when there is an intragastric foreign body that extends throughout the gastric chamber to the small intestine as in this case, open surgery is required given the high rate of complications. 17
Recurrences of this syndrome are rare, and only three have been reported in the literature. 16 In any case, psychological intervention and endoscopic follow-up have been shown to reduce recurrences. 17
Acknowledgements
We would like to thank Doctors Salin Jose Barrios Marenco and Moises Monsalve, general surgeons at the Hospital de Engativá ESE in Bogotá D. C., Colombia
REFERENCES
1. Vaughan ED Jr, Sawyers JL, Scott HW Jr. The Rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery. 1968;63(2):339‐343. [ Links ]
2. Rodríguez HM, Schleske A. Tricobezoar: Reporte de un caso. Cir Gen. 2006;28(2):113-117. [ Links ]
3. Rabie ME, Arishi AR, Khan A, Ageely H, Seif El-Nasr GA, Fagihi M. Rapunzel syndrome: the unsuspected culprit. World J Gastroenterol. 2008;14(7):1141‐1143. http://dx.doi.org/10.3748/wjg.14.1141 [ Links ]
4. Sánchez W, Rodríguez DF, Luna-Pérez P. Síndrome de Rapunzel. Rev Gastroenterol Mex. 1997;62:84-6. [ Links ]
5. Harikumar R, Kumar S, Kumar B, Balakrishnan V. Rapunzel syndrome: a case report and review of literature. Trop Gastroenterol. 2007;28(1):37‐38. [ Links ]
6. Naik S, Gupta V, Naik S, Rangole A, Chaudhary AK, Prashant J, Sharma AK. Rapunzel syndrome reviewed and redefined. Dig Surg. 2007;24(3):157‐161. http://doi.org/10.1159/000102098 [ Links ]
7. Gutiérrez JO. Tricobezoar gástrico. Rev Colomb Cir. 2000;15(1):30-2. [ Links ]
8. Alvarado R, Uribe E, Gallego JE. Tricobezoar. Presentación de dos casos. Acta Pediatr Mex. 2001;22(4):264-7. [ Links ]
9. Velasco B, Paredes RM. Tricobezoar: un problema psicológico. An Esp Pediatr. 2001;55(4): 383-384. http://doi.org/10.1016/S1695-4033(01)77707-7 [ Links ]
10. Quraishi AH, Kamath BS. Rapunzel syndrome. Gastrointestinal Endoscopy. 2005;62(4):611. http://doi.org/10.1016/S0016-5107(05)01579-8 [ Links ]
11. Balik E, Ulman I, Taneli C, Demircan M. The Rapunzel syndrome: a case report and review of the literature. Eur J Pediatr Surg. 1993;3(3):171‐173. http://doi.org/10.1055/s-2008-1063536 [ Links ]
12. Loja D, Alvizuri J, Vilca M, Sánchez M. Síndrome de Rapunzel: tricobezoar gastroduodenal. An Fac Med. 2003;64(1):71-77. https://doi.org/10.15381/anales.v64i1.1427 [ Links ]
13. Dorn HF, Gillick JL, Stringel G. Laparoscopic intragastric removal of giant trichobezoar. JSLS. 2010;14(2):259‐262. http://doi.org/10.4293/108680810X12785289144520 [ Links ]
14. Chogle A, Bonilla S, Browne M, Madonna MB, Parsons W, Donaldson J, Alonso E. Rapunzel syndrome: a rare cause of biliary obstruction. J Pediatr Gastroenterol Nutr. 2010;51(4):522‐523. http://doi.org/10.1097/MPG.0b013e3181cb950a [ Links ]
15. Gorter RR, Kneepkens CM, Aronson DC, Heij HA. Management of trichobezoar: case report and literature review. Pediatr Surg Int. 2010;26:457-463. https://doi.org/10.1007/s00383-010-2570-0 [ Links ]
16. Tiwary SK, Kumar S, Khanna R, Khanna AK. Recurrent Rapunzel syndrome. Singapore Med J. 2011;52(6):e128‐e130. [ Links ]
17. Wolski M, Gawłowska-Sawosz M, Gogolewski M, Wolańczyk T, Albrecht P, Kamiński A. Trichotillomania, trichophagia, trichobezoar - summary of three cases. Endoscopic follow up scheme in trichotillomania. Psychiatr Pol. 2016;50(1):145‐152. http://doi.org/10.12740/PP/43636 [ Links ]
Received: January 30, 2018; Accepted: June 20, 2018











 text in
text in