Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.2 Bogotá Apr./June 2020
https://doi.org/10.22516/25007440.338
Case report
Ruptured hepatic artery aneurysm: an infrequent cause of abdominal pain and gastrointestinal bleeding
1 Residente de segundo año de Medicina Interna. Hospital Nuestra Señora del Prado; Talavera de la Reina, España
2 Médico adjunto en el servicio de medicina interna. Hospital Nuestra Señora del Prado; Talavera de la Reina, España
Upper gastrointestinal bleeding is defined as bleeding originating in the upper digestive tract proximal to the Treitz angle and is the most important gastroenterological emergency. Its incidence varies, depending on the area studied, between 48 and 160 cases per 100,000 inhabitants per year. Although it can be caused by numerous etiologies, we must not forget the less common ones such as a ruptured hepatic artery aneurysm since they can condition high mortality. We present a representative case.
Keywords: Digestive hemorrhage; abdominal pain; visceral aneurysm; fungal aneurysm
La hemorragia digestiva alta se define como el sangrado originado en el tracto digestivo superior, proximalmente al ángulo de Treitz, y constituye la urgencia gastroenterológica más importante. Tiene una incidencia que varía, según el área estudiada, entre 48 y 160 casos por 100 000 habitantes y año. Aunque puede ser causada por numerosas etiologías, no debemos olvidar aquellas menos comunes, ya que pueden condicionar una alta mortalidad, como es el caso de la rotura de un aneurisma de la arteria hepática. A continuación, mostramos un caso representativo.
Palabras clave: Hemorragia digestiva; dolor abdominal; aneurisma visceral; aneurisma micótico
Clinical history
A 66-year-old man with a history of smoking, hypertension, and diabetes mellitus was admitted in January 2014 due to an ulcerated lesion in his right foot. An abscess was drained and the second toe was partially amputated. Later, an atypical amputation of his right foot was performed.
The patient was readmitted in September 2014 due to cellulitis in the right lower limb. Methicillin-resistant Staphylococcus aureus (MRSA) and Enterococcus Faecalis were isolated. The man was treated with vancomycin, levofloxacin, and linezolid with negative blood cultures.
While hospitalized, he complained of epigastric pain. Abdominal ultrasound and endoscopy in the digestive department of the hospital found hepatomegaly and ulcerative lesions in the duodenum which were probably related to stress ulcers. A CT scan found hepatomegaly, bilateral pleural effusion, and focal lesions in the liver and spleen which were suggestive of simple cysts. His proton pump inhibitor dosage was increased.
Given the finding of bilateral pleural effusion, heart failure was suspected, and the patient was evaluated by internal medicine. An echocardiogram revealed a calcified and unstructured aortic valve with moderate stenosis and mild to moderate insufficiency.
A month later, he was readmitted due to sepsis secondary to an infected wound on his right foot plus secondary osteomyelitis. Stenotrophomonas maltophila, Pseudo-monas aeruginosa and MRSA were isolated. An infracondylar amputation was performed and antibiotic therapy with Tazocel® and linezolid was started.
During this hospitalization, MRSA bacteremia was observed by transthoracic echocardiogram. Later, aortic regurgitation progressed from moderate to severe, and pulmonary hypertension and bi-atrial dilation which had not previously existed were observed. The patient was discharged with linezolid, but abdominal pain persisted.
Evolution
The patient returned to the emergency department 48 hours after being discharged due to persistent epigastric pain and cardiorespiratory arrest. After advanced cardiopulmonary resuscitation, the man recovered and was admitted to the intensive care unit. A transesophageal echocardiogram diagnosed endocarditis on the native aortic valve, and the patient was transferred to the referral center for cardiac surgery.
An aortic stent was placed and treatment with Daptomycin, gentamicin, and rifampin was started. Shortly afterwards, the patient was transferred to the cardiology department of our center to complete the antibiotic treatment.
During his stay in cardiology, he began to suffer abdominal pain and cholestasis. His alanine aminotransferase (ALT) level was 207 U/L, (2-33) his aspartate aminotransferase (AST) level was 74 U/L, (1-31) his alkaline phosphatase level was 825 U/L, (35-129) and his γ-glutamyltransferase level was 1987 U/L. (7-40)
An abdominal CT scan revealed dilation of the bilateral intrahepatic biliary tree and the hyper-uptake proximal common bile duct, with a distal filiform caliber. Abdominal ultrasound confirmed the patency of the portal vein and its branches and of the superior mesenteric vein. Upper digestive endoscopy was normal. The patient was transferred to the digestive service.
He continued to suffer epigastric pain and presented several episodes of melena, “coffee ground” vomiting and rectal bleeding with anemia that required transfusions. Thus, several upper digestive endoscopies found only three esophageal erosions and chronic gastritis. A colonoscopy was performed without findings.
A physical examination found nothing relevant to the patient’s condition, but 24 hours after his last normal endoscopy, the patient experienced an episode of rectal bleeding and hematemesis with secondary hemorrhagic shock. He was admitted to the ICU.
Another urgent upper endoscopy was performed. It found abundant blood in the stomach and an elongated clot in the papilla with adjacent leakage suggestive of hemobilia.
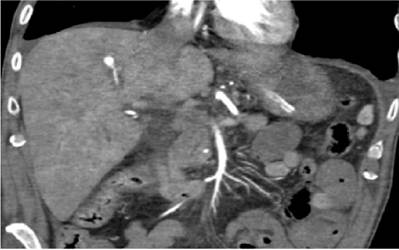
Based on these findings, CT-angiography was performed (Figure 1). It identified an aneurysm of a segmental branch of the right hepatic artery which had fusiform content suggestive of a biliary intraluminal hematoma.
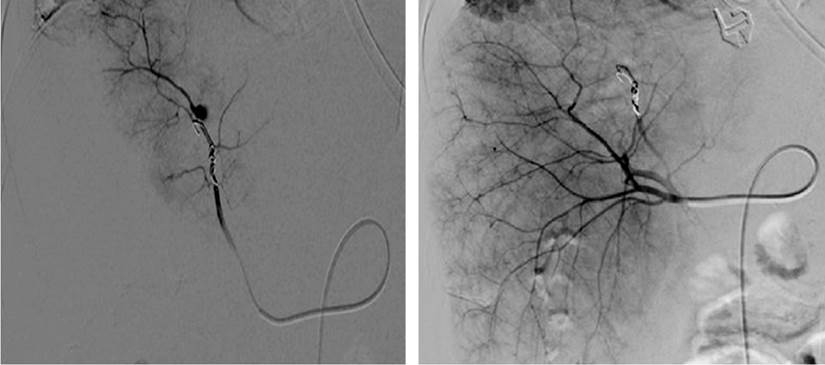
The aneurysm was then embolized (Figure 2), and the patient evolved favorably without further episodes of digestive bleeding and with complete resolution of the biliary obstruction.
Diagnosis
Our final diagnosis was an upper gastrointestinal hemorrhage caused by the rupture of an aneurysm of a segmental branch of the right hepatic artery.
Discussion
Abdominal artery aneurysms are among the most infrequent of the many possible causes of abdominal pain. A review of the literature also shows that hemobilia is an unusual trigger for upper gastrointestinal bleeding. It does not directly occur in the small intestine, is therefore not directly detectable by endoscopy, and is most often considered only as a cause of digestive bleeding of obscure origin. 1,2
Hemobilia’s symptoms, all of which occurred in our patient, include jaundice, pain in the right upper quadrant, and upper gastrointestinal bleeding. 3-5 Its cause can be traumatic, iatrogenic, inflammatory, infectious, neoplastic and vascular such as aneurysms, vasculitis and arteriovenous malformations.
Consequently, diagnosis must be made by imaging with a CT scan or MRI or by endoscopy. 8. The treatment of choice is selective embolization, but there are other options such as insertion of an endovascular stent or surgery. 3,9,10
In our case, the origin was an aneurysm of the hepatic artery, considered the second most common visceral arterial aneurysm (after aneurysms of the splenic artery). 11-13 If we focus specifically on the etiology of hepatic artery aneurysms, we observe that their causes are diverse and include arteriosclerosis (the most frequent), liver trauma, mycosis (up to 10%), IV drug addiction, iatrogenic causes and autoimmune diseases. 14
Our patients etiology of a visceral aneurysm could be attributed to two causes: arteriosclerosis, observed in various imaging tests, and a mycotic aneurysm due to the recent history of endocarditis with MRSA bacteremia (the most frequent cause in infected aneurysms).
In most cases, the diagnosis is made with incidental findings from imaging because both the symptoms and the examination of visceral aneurysms are usually unremarkable. The exception to this is when these aneurysms rupture and cause hemobilia towards the bile duct. In this scenario, treatment must be early since reported mortality is 50% and 100% depending on the case series. 3,11,14
Conclusions
The association between upper gastrointestinal bleeding and cholestasis should lead us to think about hemobilia and its causes. Differential diagnosis of abdominal pain and upper gastrointestinal bleeding of unknown origin must include visceral artery aneurysms. Despite their rarity, they can cause a patient’s death if they are not acted on in time.
Referencias
1. Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015;110(9):1265‐1288. http://doi.org/10.1038/ajg.2015.246 [ Links ]
2. Welch GH, Anderson JR, Leiberman DP. Aneurysms of the hepatic artery: a report of three cases. J R Coll Surg Edinb. 1986;31(2):91‐94. [ Links ]
3. Bellmunt-Montoya S, Maeso-Lebrún J, Royo-Serrando J, Bofill-Brosa R, Allegue-Allegue N, Matas-Docampo M. Aneurismas de la arteria hepática. Descripción de cinco casos y revisión de la literatura. Angiología. 2001;53(1):33-41. http://doi.org/10.1016/S0003-3170(01)74675-5 [ Links ]
4. Santos VM, Villaça RB, Almeida AC, Oliveira ER, Nogueira PR, Damasceno EA. Rupture of hepatic artery aneurysm associated with ischemic hepatitis. An Sist Sanit Navar. 2010;33(2):221-225. http://doi.org/10.4321/s1137-66272010000300011 [ Links ]
5. Galindo P, Martínez JD, Rey MH. Hemobilia secundaria a aneurisma de la arteria hepática. Rev Colomb Gastroenterol. 2017;32(2):171-173. https://doi.org/10.22516/25007440.145 [ Links ]
6. Rencuzogullari A, Okoh AK, Akcam TA, Roach EC, Dalci K, Ulku A. Hemobilia as a result of right hepatic artery pseudoaneurysm rupture: An unusual complication of laparoscopic cholecystectomy. Int J Surg Case Rep. 2014;5(3):142‐144. http://doi.org/10.1016/j.ijscr.2014.01.005 [ Links ]
7. Panno C, Gutiérrez SC, Echeverría R, Garbe C, Milocco M, Ianniccillo H, Valenzuela M, Cubilla A, Álvarez F, Álvarez E. Hemobilia secundaria a pseudoaneurisma de la arteria hepática. Acta Gastroenterol Latinoam. 2015;45(2):133-136. [ Links ]
8. Busuttil RW, Brin BJ. The diagnosis and management of visceral artery aneurysms. Surgery. 1980;88(5):619‐624. [ Links ]
9. Beltrán F, Castillo A, Hidalgo H. Hemobilia secundaria a pseudoaneurisma roto: reporte de caso. Rev Gastroenterol Perú. 2015;35(1):89-92. [ Links ]
10. Jonsson K, Bjernstad A, Eriksson B. Treatment of a hepatic artery aneurysm by coil occlusion of the hepatic artery. AJR Am J Roentgenol. 1980;134(6):1245‐1247. http://doi.org/10.2214/ajr.134.6.1245 [ Links ]
11. Puppo AM, Pareja F, Muñoz J, Forastero A, Bernardos A. Aneurisma de la arteria hepática. Cir Esp. 2007;81(6):348-50. http://doi.org/10.1016/S0009-739X(07)71336-2 [ Links ]
12. Stanley JC, Wakefield TW, Graham LM, Whitehouse WM Jr, Zelenock GB, Lindenauer SM. Clinical importance and management of splanchnic artery aneurysms. J Vasc Surg. 1986;3(5):836‐840. https://doi.org/10.1016/0741-5214(86)90059-5 [ Links ]
13. Graham JM, McCollum CH, DeBakey ME. Aneurysms of the splanchnic arteries. Am J Surg. 1980;140(6):797. http://doi.org/10.1016/0002-9610(80)90120-8 [ Links ]
14. Cases-Baldó MJ, Guillen-Paredes MP, Moreno-Egea A, Torres-Del Río S, Aguayo-Albasini JL. Rotura aneurismática de la arteria hepática común. Cir Esp. 2010;87(1):46- 58. http://doi.org/ 10.1016/j.ciresp.2008.10.014 [ Links ]
Received: January 15, 2019; Accepted: March 23, 2019











 text in
text in