Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957versão On-line ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.2 Bogotá abr./jun. 2020
https://doi.org/10.22516/25007440.339
Case report
A case of adult hepatoblastoma
1 Hospital Manuel Ascunce Domenech; Camagüey, Cuba
Background:
In contrast to childhood hepatoblastoma, adult hepatoblastoma (HBA) is a rare and not-fully-understood liver tumor with a poor prognosis. To date, about 50 cases have been adequately reported in the medical literature.
Objective:
We present the case of a patient who was discharged from our hospital with a diagnosis of hepatocellular carcinoma approximately 3 months before returning.
Clinical case:
A 60-year-old male patient with a history of alcoholism and heavy smoking was admitted to our hospital for abdominal pain. Physical examination revealed a palpable tumor in the right hypochondrium region. This patient had been discharged approximately 3 months previously with a diagnosis of hepatocellular carcinoma in the course of liver cirrhosis. The patient died, and the autopsy revealed an HBA.
Conclusions:
Adult hepatoblastoma is an infrequent tumor with a severe prognosis. Many cases are asymptomatic until the time of diagnosis, and the tumor is usually very large. Liver enzymes, alpha-fetus protein, and imaging studies lead to a diagnosis of hepatocellular carcinoma which is a common tumor in adults. Histological study confirms the diagnosis. Due to the poor prognosis for HBA in contrast to better prospects for treatment of hepatoblastoma in children, it is logical to use pediatric treatment in adults. More research is needed for the optimal treatment of HBA.
Keywords: Liver tumors; hepatoblastoma; liver cancer; adults
Fundamento:
el hepatoblastoma del adulto (HBA) es un tumor hepático poco frecuente y con un mal pronóstico, lo cual contrasta con el hepatoblastoma infantil (HBI). Esta patología aún no ha sido comprendida completamente y hasta la fecha, no se han reportado de forma adecuada más de 50 casos en la literatura médica.
Objetivo:
presentar el caso de un paciente que fue egresado de nuestro hospital con el diagnóstico de carcinoma hepatocelular, aproximadamente con 3 meses de anterioridad.
Caso clínico:
paciente masculino de 60 años con historia de alcoholismo y de ser un fumador inveterado. Fue ingresado en nuestro hospital por dolor abdominal, en el momento del examen físico, puso de manifiesto un tumor palpable en la región del hipocondrio derecho. Este paciente había sido egresado aproximadamente 3 meses atrás, con el diagnóstico de carcinoma hepatocelular, en el curso de una cirrosis hepática. El hombre falleció por causa de la progresión de la enfermedad y la autopsia reveló la existencia de un HBA.
Conclusiones:
el HBA es un tumor infrecuente, de grave pronóstico y muchos casos son asintomáticos hasta el momento del diagnóstico. Dicho tumor, por lo regular, presenta un gran tamaño. Las enzimas hepáticas, la alfafetoproteína y los estudios imagenológicos revelan el diagnóstico de un hepatocarcinoma, el cual es un tumor frecuente en los adultos. Asimismo, el estudio histológico confirma el diagnóstico. Debido a su mal pronóstico, y a las mejores perspectivas de tratamiento en niños, hoy en día es lógico utilizar el tratamiento pediátrico en los adultos. Se necesitan más estudios de investigación para el manejo óptimo del HBA.
Palabras clave: Tumores del hígado; hepatoblastoma; cáncer hepático; adultos
Introduction
Among the malignant liver tumors, hepatoblastomas are common at early ages. This type of tumor has different names but is most frequently called a malignant mixed tumor of the liver due to the different classes of cells found within it. In the past, the term blastoma was not used for this type of tumor in adults, but it has been accepted since it was found that there are no differences between adult hepatoblastoma (AHB) and childhood hepatoblastoma (CHB). 1
AHB is a rare liver tumor whose prognosis is poor, unlike the prognosis of CHB. AHB is not yet fully understood. 2 It was first described as a mixed liver tumor by Marx in 1904. 1 Since then only about 50 cases have been adequately reported in the medical literature. 3
In contrast to CHB, AHB has a fatal prognosis with a mean life expectancy of two months and a one-year survival rate of only 24%. 4 Many theories posit an embryonic origin of hepatoblastomas and give an important role to hepatic stem cells. 5 This study presents the first case of a patient with an ABH described and diagnosed in our hospital.
Clinical case
The patient was a 60-year-old farmer who was an alcoholic and inveterate smoker. He was admitted to our service due to abdominal pain and a tumor mass in the right upper quadrant. He had been discharged from this hospital three months earlier following diagnosis of hepatocellular carcinoma and liver cirrhosis.
The patient reported suffering general malaise, dyspepsia, epigastric pain and pain in the right upper quadrant for several months prior to admission. He had lost 12 kg of weight. He stated that he had had no contact with toxic substances but had had contact with multiple domestic animals. Physical examination revealed a great alteration of his constitutional state including paleness and sweating. He was afebrile, and without lymphadenopathy, but the whites of his eyes were mildly jaundiced.
His cardiorespiratory apparatus was normal, with a blood pressure of 110/70 mm Hg, and a heart rate of 112 bpm. A hard tumor with a smooth surface was found in his abdomen. On palpation, the patient experienced pain in the right upper quadrant that extended 12 cm beyond the costal margin.
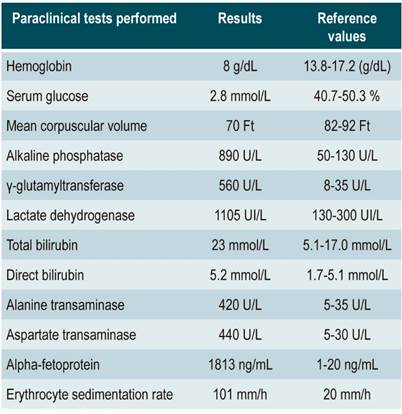
No alterations were found in other organs or systems including the urological system and the fundus which were normal. Positive test results are described in Table 1.
All other tests including ions, pancreatic enzymes, coagulation, and kidney function were normal. Tests for hepatitis B virus surface antigens and the antibody against the hepatitis C virus were negative.
A chest x-ray showed pulmonary emphysema, an electrocardiogram confirmed a sinus tachycardia, and abdominal ultrasound found a 12-15 cm solid mass with fine edges, a firm consistency, and a nodular surface.
A CT scan found a large liver mass with areas of necrosis measuring approximately 15 cm that had the same characteristics found with ultrasound.
The patient’s relatives refused to allow fine needle aspiration biopsy (FNA) of the liver given the patient’s very serious condition and the fact that his diagnosis was already known.
The patient died as a consequence of the severity of his illness. Based on the institutional policy for improvements in medical practice, a post-mortem study was carried. An enlarged liver (approximately 15 cm) with fine borders was observed macroscopically (Figure 1).
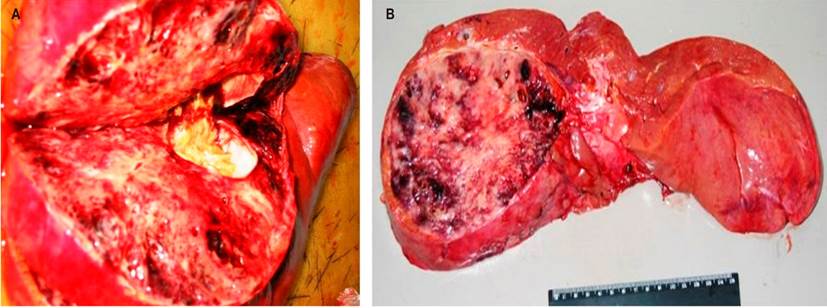
Figure 1 A. Right lobe section showing apparently well-defined tumor mass with a motley appearance and whitish hemorrhagic areas. B. Typical tumor.
The histopathological study was compatible with a mixed epithelial hepatoblastoma of the liver, as shown below (Figures 2 and 3).
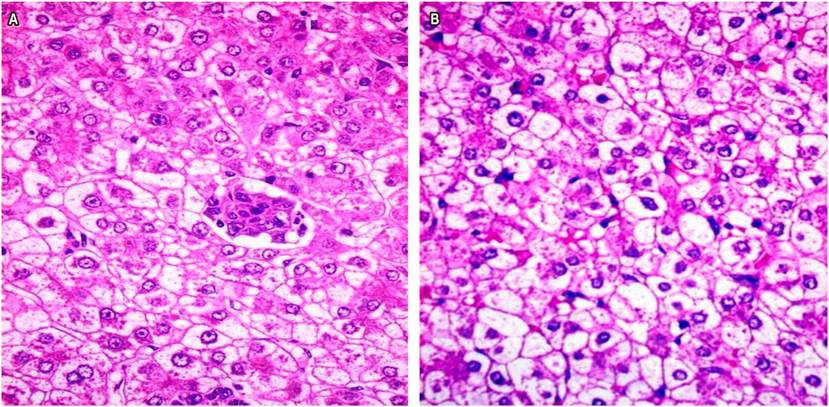
Figure 2 Photomicrographs showing the epithelial area with a characteristic fetal pattern, uniform, polyhedral cells, and abundant fat and glycogen.
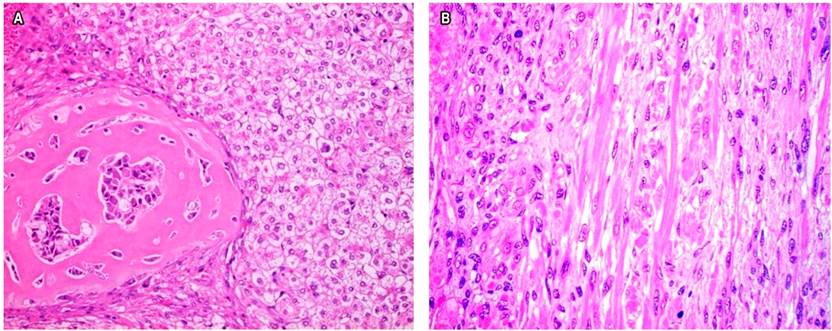
Figure 3 A. Histological image of a tumor field shows a thick trabecular pattern and collagen with central immature cells within a typical epithelial area. B. Histological image of another field of the tumor, epithelial type, showing an embryonic differentiation pattern with a less cohesive cell arrangement plus the presence of trabeculae. Note the irregular chromatin and prominent nucleolus. H/E- 40X.
Discussion
A hepatoblastoma is a malignant tumor of the liver which usually affects children under 2 years of age. They can be fatal if they are not removed. 4 This type of tumor has two anatomical variants: the epithelial type and the mixed epithelial and mesenchymal type. The latter contains foci of mesenchymal differentiation consisting of primitive mesenchyme, osteoid, cartilage, and striated muscle. 6
These tumors have received somewhat confusing names including mixed embryonal liver tumor, mixed tumor of the liver, adult hepatoblastoma, and mixed adult hepatoblastoma. This last term is the most commonly accepted today. 7
Hepatoblastomas are rare tumor in childhood: their annual incidence is only 0.5-1.5 per 1,000,000 people. They usually occur in children from six months to five years of age. 8
According to some authors, the first case of AHB was reported in 1958. 9 According to Xiao et al., as of this date only 50 cases of this pathology have been recognized. 3
AHB presents in a way that is similar to CHB with the appearance of a mass, usually in the right upper quadrant. These hepatoblastomas are usually asymptomatic and affect both sexes equally. The average age of patients at diagnosis is 52 years. 5,7
AHB is not commonly associated with liver cirrhosis. In fact, radiologically visible tumor calcifications are common, and they are not usual in other malignant liver tumors. 4,7 They were not reported in our case.
AHB is a slow-growing tumor which is well tolerated by patients and has few symptoms. There is usually pain, and a palpable mass frequently appears 2 to 4 months after diagnosis. 10 this was observed in our patient at a time when the tumor had grown to a large size and had already disseminated. 10
Our patient had manifestations of an important constitutional syndrome with symptoms including asthenia, anorexia, great weight loss and jaundice due to compression of the biliary tree. 1,6,7
In 25% of cases, AHB has been associated with liver diseases such as liver cirrhosis, hepatitis B and hepatitis C. 1 Hepatitis was not observed or demonstrated in our case.
The diagnosis of AHB has always been the result of the histological study of surgical specimens or autopsies. 1-7 Our patient’s autopsy confirmed the diagnosis. It was performed following the institutional policy of improvements in medical practice.
Imaging, including abdominal ultrasound, axial tomography and magnetic resonance imaging, is of great value. These tests allow observation of a large nodular mass measuring 5-24 cm in diameter that is circumscribed by a fine fibrous capsule or pseudocapsule. 1 Our patient’s tumor measured 15 cm and had no calcifications or capsule that could be seen by imaging. It should also be mentioned that alpha-fetoprotein levels have been elevated in more than 50% of the reported cases of ABH. 1,5
The histology of AHB has been compared to that of CHB which has been subdivided into 4 histological categories: the fetal form (1/3 of all cases), the mixed embryonic-fetal form (20%), the macrotrabecular form (30%), and a form composed of small undifferentiated cells (2-3%). 6,9,10
About 25% of the published ABH cases have conditions such as fibrosis and cirrhosis. (4) Also, findings of mesenchymal components that resemble fibrosarcoma, osteosarcoma, chondrosarcoma, angiosarcoma, and rhabdomyosarcoma have been described. 1,10
The most common cellular components are hepatoblasts, the hepatic endoderm cells, and bipotential progenitor cells which can differentiate into either hepatocytes or cholangiocytes. 1,7,8
A mutation in the Wnt/β-catenin pathway, reported in 50% to 90% of cases, has recently been found to be a signal that orients hepatoblastomas in childhood. 11
A pleomorphic finding of hepatoblastomas denotes common origin of stem cells which allows observation of epithelial factors including hepatocytes and cholangiocytes as well as mesenchymal phenotypes in the endothelium and sinusoids. 5,10,11 Nevertheless, diagnosis remains the result of histological study of surgical or autopsy specimens. 1,9
In this context, AHB requires surgery (as do all liver tumors) when the diagnosis is made before spread or overgrowth of the hepatoblastoma. Consequently, complete oncological resection is the cornerstone of treatment and avoids complete liver resection especially in those cases in which the patient does not present symptoms.
At the time of diagnosis, the vast majority of patients have an unresectable tumor. 12 Surgical treatment has shown very poor results: an overall one year survival rate of 24%. However, one year survival in cases of unresectable tumors is 0% while it is 41% for resectable tumors. 1
It has been reported that patients who whose tumors have been resected when they are under 45 years of age have a better prognosis (42%) than do patients over the age of 45 years managed in the same way whose one year survival rate is 0%. 1,7
Tumors that have not been operated on have shown good responses to systemic transcatheter arterial chemoembolization with cisplatin and pirarubicin. 13
Thus, the treatment and prognosis for CHB is much better than for AHB. Various types of vincristine, cisplatin, and 5-fluoracil therapies have been used as adjunctive treatments. Other methods include hepatectomy and liver transplantation.
Thanks to these alternatives, the 5-year survival rate has reached 75%, and the five-year recurrence-free survival rate has reached 66%. In contrast, prognoses for adults are usually poor, so that the only currently valid treatment option is radical surgery, whenever it is possible), both for primary tumors and for metastases. 14
Conclusions
AHB is an uncommon tumor in people over 5 years of age, and its prognosis is fatal in adults. Often, it is asymptomatic, and when symptoms appear, the tumor is already large making therapy difficult.
This pathology requires high levels of diagnostic suspicion with protocol studies, such as liver enzymes and alpha-fetoprotein screening, pointing to a liver tumor. In the case of our patient, it was hepatocellular carcinoma rather than a hepatoblastoma, as described. The patient died, but his diagnosis was made through a histological study which is usually omitted in the procedures of these cases given their poor prognoses and the inexperience that is common for management of hepatoblastomas in adults.
In view of the biological similarities, it seems logical to implement the stratification and control schemes for management of ABH that are usually used in the approach to the pediatric population.
Referencias
1. Rougemont AL, McLin VA, Toso C, Wildhaber BE. Adult hepatoblastoma: learning from children. J Hepatol. 2012;56(6):1392‐1403. http://doi.org/10.1016/j.jhep.2011.10.028 [ Links ]
2. de Bree K, Westermann AM, Klümpen HJ, Verheij J, Phoa SS, Oomen M, van Gulik TM. Two Cases of Hepatoblastoma in Young Adults. J Adolesc Young Adult Oncol. 2018;7(3):404‐408. http:// doi.org/10.1089/jayao.2017.0125 [ Links ]
3. Duan XF, Zhao Q. Adult hepatoblastoma: a review of 47 cases. ANZ J Surg. 2018;88(1-2):E50‐E54. http//doi.org/10.1111/ans.13839 [ Links ]
4. von Schweinitz D. Hepatoblastoma: recent developments in research and treatment. Semin Pediatr Surg. 2012;21(1):21‐30. http://doi.org/10.1053/j.sempedsurg.2011.10.011 [ Links ]
5. Darwiche H, Petersen BE. Biology of the adult hepatic progenitor cell: “ghosts in the machine”. Prog Mol Biol Transl Sci. 2010;97:229‐249. http://doi.org/10.1016/B978-0-12-385233-5.00008-8 [ Links ]
6. Cotran RS, Kumar V, Collins J. Hígado y vías biliares. En. Cotran RS, Kumar V, Collins J. Patología Estructural y Funcional de Robbins. Madrid: McGraw-Hill Interamericana; 2006. p. 926. [ Links ]
7. Wang YX, Liu H. Adult hepatoblastoma: systemic review of the English literature. Dig Surg. 2012;29(4):323‐330. http://doi.org/10.1159/000342910 [ Links ]
8. Litten JB, Tomlinson GE. Liver tumors in children. Oncologist. 2008;13(7):812‐820. http://doi.org/10.1634/theoncologist.2008-0011 [ Links ]
9. Barnett WH, Erickson EE, Halpert B. Embryonic tumor of the liver in an adult. Cancer. 1958;11(2):306‐309. http://doi.org/10.1002/1097-0142(195803/04)11:2<306::aid-cncr2820110211>3.0.co;2-r [ Links ]
10. Zimmerman A, Saxena R. Hepatoblastoma. En: Bosman F, Carneiro F, Hurban R, Theise ND. WHO Classification of Tumours of the Digestive System. Lyon: International Agency for Research on Cancer ; 2010. p. 228-35. [ Links ]
11. Cairo S, Armengol C, Buendia MA. Activation of Wnt and Myc signaling in hepatoblastoma. Front Biosci (Elite Ed). 2012;4:480‐486. http://doi.org/10.2741/393 [ Links ]
12. Diehl AM. Neighborhood watch orchestrates liver regeneration. Nat Med. 2012;18(4):497‐499. http://doi.org/10.1038/nm.2719 [ Links ]
13. Boulter L, Govaere O, Bird TG, Radulescu S, Ramachandran P, Pellicoro A, Ridgway RA, Seo SS, Spee B, Rooijen NV, Sansom OJ, Iredale JP, Lowell S, Roskams T, Forbes SJ. Macrophage-derived Wnt opposes Notch signaling to specify hepatic progenitor cell fate in chronic liver disease. Nat Med. 2012;18(4):572‐579. http://doi.org/10.1038/nm.2667 [ Links ]
14. Caso-Maestro Ó, Justo-Alonso I, Cambra-Molero F, Manrique-Municio A, Calvo-Pulido J, Jiménez-Romero C. Adult hepatoblastoma: case report with adrenal recurrence. Rev Esp Enferm Dig. 2013;105(10):638‐639. http:/doi.org/10.4321/s1130-01082013001000014 [ Links ]
Received: January 13, 2019; Accepted: February 18, 2019











 texto em
texto em